Physical, Mental, and General Health Outcomes Among Childhood Cancer Survivors From the Behavioral Risk Factor Surveillance System Survey
Objectives: To examine the physical, mental, and general health among young adult childhood cancer survivors (CCS).
Sample & Setting: This secondary analysis study used data from the Behavioral Risk Factor Surveillance System. The analytic sample included 697 young adult CCS (537 women; 160 men).
Methods & Variables: Chi-square tests of independence were done to compare the rates across cancer survivorship groups on categorical variables. Logistic regression was performed to determine correlates with physical, mental, and general health.
Results: Female CCS had a significantly (p < 0.0001) greater number of “no days” in which they reported good physical, mental, and general health compared to male CCS. Female CCS were more likely to experience 30 days of poor physical health compared to male CCS (odds ratio [OR] = 1.8, p < 0.05) when controlling for education, race, and age. Depressed female CCS had higher odds of being in poor physical, mental, and general health (OR = 2.9, 7.6, and 2.6, respectively).
Implications for Nursing: Findings support the need for continued screening, following published practice guidelines, among young adult female CCS for emotional distress with the use of well-established distress and psychosocial assessment measures.
Jump to a section
In 2020, there were approximately 429,000 adult childhood cancer survivors (CCS) in the United States, which equates to 1 in 530 adults, ages 20–39 years (CureSearch for Children’s Cancer, 2020). As of January 1, 2021, it was estimated that there were 47,760 older adolescent and young adult CCS aged 15–19 years living in the United States (American Cancer Society, 2022). Phillips et al. (2015) reported that nearly 84% of CCS have survived five or more years post-diagnosis, and the estimated prevalence of CCS reflects a rapidly expanding clinical population. Despite these survival rates, Philips et al. (2015) also identified that approximately 70% of CCS have a mild or moderate chronic condition, and 32% were estimated to have a severe, disabling, or life-threatening condition. These morbidity prevalence estimates have a profound impact on survivors’ ability to manage their survivorship care needs, and negatively affect their health-related quality of life (HRQOL) (Hayek et al., 2020; Lie et al., 2017; Vuotto et al., 2017; Wilson et al., 2020). Among survivors aged 20–49 years, an estimated 16% have compromised physical HRQOL, and 18% have compromised mental HRQOL (Philips et al., 2015). Recent evidence continues to support poor HRQOL among CCS. In a sample of 227 Swedish adult survivors of childhood leukemia, survivors scored significantly lower on the HRQOL for general health (p = 0.004) and emotional health (p = 0.014) compared to their siblings and to Swedish norms (Aili et al., 2021).
Female CCS have been identified as most at risk for poor physical and psychosocial outcomes and a diminished HRQOL. Older adolescent and young adult female CCS experience higher levels of psychological distress and depression when compared to male CCS and healthy siblings (Armstrong, et al., 2007; Philips et al., 2015; Wu et al., 2007). Psychological distress and depression have been identified as strong negative predictors of the psychological domain of HRQOL among older adolescent and young adult female CCS (Lund et al., 2010; Yağc-Küpeli et al., 2012; Zeltzer et al., 2009). Perhaps the most compelling evidence to suggest that female survivors are at greater risk for lower HRQOL are the findings reported by Zeltzer et al. (2009), who reviewed the findings of 11 published studies from the landmark Childhood Cancer Survivor Study (CCSS) and concluded that female gender was a major risk factor for psychological distress, which is a component of individuals’ HRQOL.
In addition, female CCS are at increased risk for adverse physical health status. Armstrong et al. (2007) conducted a systematic review of 161 published studies on seven long-term health outcomes of CCS, and found the following effects more prevalent in women: increased risks for cognitive dysfunction, anthracycline-mediated cardiotoxicity, obesity, early onset of puberty, primary hypothyroidism, breast cancer, and osteonecrosis, depending on various treatments received. In a more recent nationwide study of young adult CCS, van Erp et al. (2021) reported that a risk factor (p < 0.05) for impaired physical HRQOL was female gender. In summary, past and current evidence suggests that female CCS have greater threats to their HRQOL in survivorship, and in many cases have more long-term complications.
The present study aimed to add to the evidence of HRQOL outcomes among young adult CCS, particularly in women. In this study, researchers aimed to do the following: (a) examine the physical, mental, and general health domains of HRQOL in young adult female CCS, and compare those findings to male CCS, age-matched young adult females with no reported cancer diagnosis, female survivors of adult cancer, and the overall general population; (b) examine the relationships among age, sex, level of education, and race between physical, mental, and general health in young adult CCS; and (c) examine the relationships between depression, physical, mental, and general health and physical activity limitations among young adult female CCS.
This study examined data among individuals using unrelated controls to address a known limitation in the CCS literature. A substantial body of evidence has compared psychosocial outcomes among CCS with those of their siblings. Because siblings of CCS have similarities in ethnicity, culture, community, socioeconomic status, genetics, and environment, researchers have deemed them as a good comparison group for psychological health outcomes (Leisenring et al., 2009). However, Zeltzer et al. (2009) raised concern that some siblings are also affected by the cancer experience, which may contribute to psychological distress. There is published evidenced that some siblings of CCS experience significant symptoms of post-traumatic stress disorder (Alderfer et al., 2003), have a low overall quality of life (Houtzager et al., 2004), are at risk for long-term psychological adjustments (Buchbinder et al., 2010), and endure long-term psychological effects (Barrett et al., 2020).
Wilson and Cleary (1995) developed a conceptual model that links clinical variables with HRQOL and patient outcomes while placing health on a continuum encompassing five aspects (symptom status, biologic/physiologic variables, functional status, general health perceptions, and overall HRQOL), which are influenced by environmental factors, nonmedical factors, and individual characteristics. The revised model by Ferrans et al. (2005) focused on five types of patient outcome measures: biologic function, symptoms, functional status, general health perception, and overall quality of life. This revised model was applied to guide this study and specifically examine the relationship among symptoms (depression), functional status (activity limitations), as well as the influence of individual characteristics that included age, age at cancer diagnosis, gender, level of education, and those interactions with survivors’ physical, mental, and general health HRQOL.
Methods
Design
Large population-based data sets have been used to examine the health outcomes of CCS in the general U.S. population. The Centers for Disease Control and Prevention (CDC) used the Behavioral Risk Factor Surveillance System (BRFSS), a cross-sectional national state-based survey, to collect yearly data regarding health-related risk behaviors and health outcomes. Phillips-Salimi et al. (2011) examined BRFSS data and compared CCS to healthy young adults on a variety of indicators for physical and mental health status, including depression and health behavior variables. Control factors were in place to adjust for age, sex, and minority statuses. CCS had significantly (p < 0.001) poorer outcomes than individuals without cancer for the following categories: socioeconomic status, comorbid conditions, life satisfaction, social and emotional support, general health, and good days per month for physical, mental, and general health (Phillips-Salimi et al., 2011). Using the same BRFSS data, Warner et al. (2016) evaluated health behaviors between older adolescent and young adult CCS with same-age peers without a history of cancer. That study found 31.3% of female CCS reported fair or poor general health compared to 15.4% of female controls, and 27% reported poor social or emotional support compared to 20.5% of female controls.
The present study was also a secondary data analysis of BRFSS data, extending the work of Phillips-Salimi et al. (2011) and Warner et al. (2016) by examining data for health outcomes using pooled data from three BRFSS survey years. Phillips-Salimi et al. (2011) and Warner et al. (2016) examined CCS health outcomes using BRFSS at only one time point. Pooled data were analyzed from survey years 2014, 2016, and 2017. Institutional review board approval (exempt status) was obtained.
Although BRFSS is a national survey, states can elect to include an optional module, which uses questions about cancer survivorship. For this analysis, a total of 14 states are represented: nine midwestern states, two southern states, one state from the mid-Atlantic region, one U.S. territory, and Alaska. The select survey years’ optional module included the following question: At what age were you told by a healthcare provider that you had cancer? A delimitation of the sample was done to identify those who were initially diagnosed at the age of 22 years or younger (childhood cancer), those who were diagnosed with cancer in adulthood (aged older than 22 years), and those who had never been diagnosed with cancer. BRFSS data from 2015 were not included in the analysis because the survey year did not include this question. BRFSS respondents who were diagnosed with cancer but did not identify the age they were diagnosed were excluded (n = 906). The total sample size for the study, representative of all three survey years combined, included 697 respondents who were diagnosed with cancer before the age of 22 years, 22,465 respondents who were diagnosed with cancer in adulthood, and 1,376,915 adult respondents who were never diagnosed with cancer.
The standard four-item set of the CDC Healthy Days measurement (CDC HRQOL–4) has been included in the BRFSS since 1993 (CDC, 2022). The CDC HRQOL–4 assesses physical, mental, and general health by asking participants to rank their general health, to list how many days each month they would rate their physical or mental health as poor, and how many days of poor mental or physical health prevent them from completing their daily tasks. The response options included a fill-in response, none, do not know/unsure, and refuse to answer. Physical, mental, and general health responses were analyzed by categorizing responses as “no days,” “some days,” and “all 30 days” in which health status was reported as being poor.
The psychometric properties of the CDC HRQOL–4 have been well established among healthy and clinical populations (CDC, 2022). No published data on the measure’s reliability and validity among samples of CCS were reported in the published literature. Zullig et al. (2004) reported preliminary evidence of construct and known-groups validity among 5,220 high-schoolers. Among adult cancer survivors, Kapp et al. (2009) reported the test-retest reliability to be moderate to excellent, and Andresen et al. (2003) reported it had moderate to excellent test-retest reliability among a sample of Missouri adults (Andresen et al., 2003).
Missing data were identified for each domain of HRQOL–4. For physical health, missing data were identified for 7 (1%) CCS, 522 (2.3%) adults diagnosed with cancer, and 29,276 (2.1%) respondents who reported never being diagnosed with cancer. For mental health, missing data were identified for 14 (2.1%) CCS, 300 (1.5%) adults diagnosed with cancer, and 22,732 (1.7%) respondents who reported never being diagnosed with cancer. For general health, missing data were identified for 1 (0.1%) CCS, 60 (0.3%) adults diagnosed with cancer, and 4,113 (0.3%) respondents who reported never being diagnosed with cancer. Cases that had missing data were excluded from the analyses.
All analyses were done in R, version 4.0.3, and RStudio, version 1.4.1103. Chi-square tests of independence were done to compare the rates across cancer survivorship groups on categorical variables. Independent sample t tests were done to compare mean values across cancer survivorship groups of all numeric variables. Logistic regression was performed to determine correlates with physical, mental, and general health. All tests were two-sided and used a significance level of 0.05.
Results
Comparing HRQOL of Female CCS to Other Groups
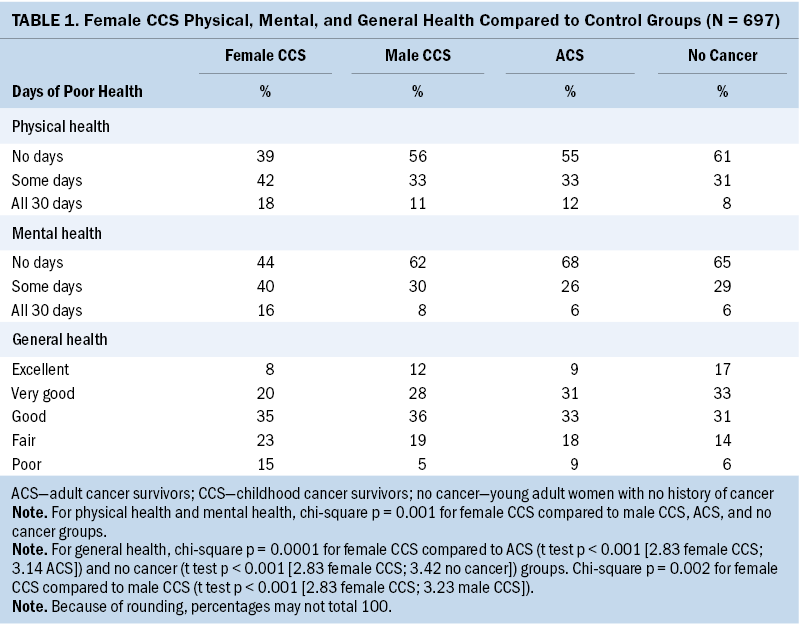
Female CCS had a statistically significant higher number of poor physical, mental, and general health days compared to young adult male CCS, young adult females with no history of cancer, female survivors of adult cancer, and the general population (see Table 1). In addition, female CCS reported a significantly greater number of “no days” in which they reported good physical, mental, and general health compared to male CCS, female survivors of adult cancer, and the general population.
Demographic Variables on HRQOL in CCS
Logistic regression models examined the relationships of age, sex, education, and race, individually and in the presence of the other variables, on physical, mental, and general health in male and female young adult CCS. Female CCS were significantly more likely to experience 30 days of poor physical (odds ratio [OR] = 1.8, p < 0.05), mental (OR = 0.6, p < 0.05), and general health (OR = 1.6, p < 0.05) compared to male CCS when controlling for education, race, and age. There was no difference between CCS who were high school graduates and those with some college credits for mental and general health statuses. For physical health, CCS with only a high school education were more likely than those with a college degree to experience 30 days of poor health (OR = 2.6, p < 0.001). Having a high school diploma or some college education credits were not predictors of 30 days of poor health among young adult CCS when controlling for age and race.
This analysis was then extended by calculating a series of logistic regression models to explore any interaction effects among these variables on survivors’ physical, mental, and general health. The only significant interaction effect (p < 0.05) was between sex and education for physical health. Physical health was lower for male CCS without a high school degree.
Depression and HRQOL in Female CCS
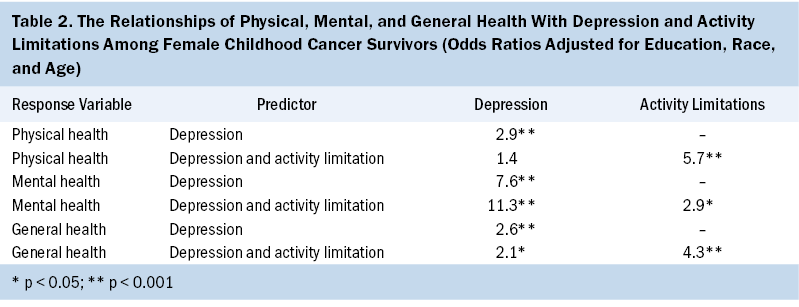
Regression models were constructed to explore the relationship between depression and physical, mental, and general health among young adult female CCS, adjusting for education, race, and age. Activity limitations were also included in this analysis as a covariate (see Table 2). Young adult female CCS who self-identified as being depressed had significantly higher odds of being in poor physical (OR = 2.9, p < 0.001), mental (OR = 7.6, p < 0.001), and general health (OR = 2.6, p < 0.001). When activity limitations were added to the models, the magnitude of the relationship increased between depression and poor mental health (OR = 11.3, p < 0.001), decreased between depression and poor general health (OR = 2.1, p < 0.05), and was not statistically significant between depression and poor physical health.
One finding from this analysis was the very high OR of low general health among young adult Hispanic female CCS. Although this estimate is not generalizable because of the small sample size (n = 8), with one Hispanic female CCS reporting very high general health and seven reporting low general health, it requires acknowledgment. Although this finding must be viewed with extreme caution, it supports findings from Ward et al. (2014), who found that overall Hispanic CCS experience poorer health outcomes compared to CCS from other cultural groups.
Discussion
According to the findings, this study was the first published study that took advantage of a large state-based national survey using pooled data from several survey years to examine health-related survivorship outcomes among young adult CCS, adult cancer survivors, and the general population. A comparison between the outcomes of physical, mental, and general health between CCS and adult survivors of cancer may be confounded by a myriad of physical and psychological developmental and treatment variables. However, viewed within the context of having cancer, despite the age at diagnosis, the findings of this study provide strong evidence of the startling differences in physical, mental, and general health for young adult female CCS compared to male CCS, adult cancer survivors, and the general population.
This study adds to the existing evidence reporting the poor physical, mental, and general health outcomes among young adult CCS (Armstrong et al., 2007; Philips et al., 2015; van Erp et al., 2021; Wu et al., 2007), particularly poorer findings among female CCS (Lund et al., 2010; Yağc-Küpeli et al., 2012; Zeltzer et al., 2009). This finding aligns with those by Cantrell and Posner (2014), who examined depressive symptoms in 66 young adult female CCS and 8,186 young adult women with no history of cancer. Cantrell and Posner (2014) used randomized, nonparametric testing to construct 10,000 different age-matched female cohort samples from the general population in National Longitudinal Study of Adolescent Health. Young adult female CCS had statistically significant more depressive symptoms than age-matched cohorts surveyed in 589 of the 10,000 matched sample (Cantrell & Posner, 2014).
In consideration of published findings from other studies on CCS, there is evidence of a relationship among the constructs of emotional status, physical health, general health, and activity limitations. Specifically, this study examined physical limitations as a covariate in the relationship between depression and physical, mental, and general health, which has not been done previously. Regarding physical limitations, Ness et al. (2009) examined the findings of 22 studies that included samples from the CCSS cohort assessing physical performance limitations in CCS. Overall, Ness et al. (2009) concluded that physical performance limitations are prevalent among CCS and may increase as the survivors age. Differences between men and women in age-adjusted models found female CCS to have a greater risk than male CCS for late effects, including physical disability. Hayek et al. (2020) estimated the prevalence of frailty among CCS (n = 10,889) compared to their siblings (n = 2,097) to determine the direct and indirect effects of treatment exposures, lifestyle factors, and severe, disabling, and life-threatening chronic conditions on frailty. Frailty was measured by low lean mass, exhaustion, low energy expenditure, walking limitations, and weakness. The overall prevalence of frailty among CCS was three times higher compared to survivors’ siblings (Hayek et al., 2020). Among CCS, the three frailty components with the highest prevalence were walking limitations, low energy expenditure, and self-reported exhaustion. In addition, the prevalence of female CCS prefrailty and frailty was higher compared to male CCS and siblings in most age groups (Hayek et al., 2020).
Although no studies were found that examined the relationship between depression and physical limitations among CCS to corroborate the findings of the current study, empirical evidence among these constructs exists in adult samples. As noted by Choi et al. (2019), randomized clinical trials have suggested that physical activity is linked to reduced depressive symptoms in at-risk populations, and prospective studies have demonstrated associations between higher levels of physical activity and decreased risk for later depression. Choi et al. (2019) posited that questions remain as to whether physical activity has a protective role in developing depression or conversely, depression is a causal factor in an individual’s degree of physical activity. Choi and colleagues (2019) identified studies that have supported the hypothesis that physical activity has a protective role for experiencing depression; however, they noted the findings of other studies have provided evidence that depression may lead to reduced physical activity. Among 611,583 adults, higher levels of physical activity (indexed by objective accelerometer data) were linked to reduced odds for major depression (Choi et al., 2019).
In an examination of specific risks of adverse physical outcomes of late mortality, subsequent neoplasms, and chronic health conditions among CCS, Lie et al. (2017) reported that non-Hispanic Black CCS (n = 694, 5%) and Hispanic CCS (n = 757, 5.4%) experienced greater burden of morbidity and mortality compared to non-Hispanic White CCS (n = 12,397, 89.6%). The limited existing evidence as to whether Hispanic CCS have poorer psychosocial health outcomes compared to CCS of other ethnicities is mixed. Casillas et al. (2006) compared the similarities and differences in HRQOL among Hispanic and non-Hispanic adult long-term CCS using focus groups and individual semistructured telephone interviews. Hispanic CCS reported good HRQOL, similar to what non-Hispanic CCS reported (Casillas et al., 2006). In contrast, Rosales et al. (2021) explored differences in perceived satisfaction, resilience, and achievement between Hispanic and non-Hispanic White CCS. Resilience and achievement scores were lower (p = 0.003 and p = 0.005, respectively).
The findings of this study provide evidence of the relationships among the constructs in the revised conceptual model for HRQOL by Ferrans et al. (2005). The findings of comparing HRQOL of female CCS to other groups provide empirical support as to how the individual characteristic of female gender influences physical, mental, and general health. Likewise, the findings for depression and HRQOL in CCS support the proposed causal links within the model among the health domains of symptoms, functional status, general health perception, and quality of life. Specifically, young adult female CCS who self-identified as being depressed had significantly higher odds of being in poor physical, mental, and general health.
Strengths
This study used a large population-based national sample to compare health outcomes of young adult CCS with unrelated matched controls and gender and age-matched controls for comparison between young adult female CCS, groups of adult cancer survivors, and the general population. In contrast, a substantial body of evidence has compared psychosocial outcomes among CCS with those of their siblings. Because siblings of CCS have similarities in ethnicity, culture, community, socioeconomic status, genetics, and environment, researchers have deemed them as a good comparison group for psychological health outcomes (Leisenring et al., 2009). However, Zeltzer et al. (2009) noted that some siblings are also affected by the cancer experience, which may contribute to psychological distress.
Limitations
It must be acknowledged that data for age at diagnosis, type of cancer diagnosis, treatment, and late treatment effects influence CCS HRQOL. Findings of previous studies have provided evidence that CCS HRQOL is influenced by these clinical variables. No data were collected for these variables for BRFSS years of 2014, 2016, and 2017, nor were data collected for CCS support systems, including marital status, which has been found to influence HRQOL. The measurement of HRQOL, using CDC HRQOL–4, was limited to one question on physical health, mental health, and activity limitations. An examination of five indexes of HRQOL by Cherepanov et al. (2010) found that the three main dimensions of HRQOL among adults in the United States were physical, psychosocial, and pain. The CDC HRQOL–4 did not include the dimension of pain. In addition, the CDC HRQOL–4 was not developed specifically for CCS. Zebrack (2009) developed a 45-item, eight-factor (life challenges, body and health, personal growth, thinking/memory problems, health literacy, socializing, sibling concerns, relationship concerns) HRQOL instrument, the Impact of Cancer Scale for young adult survivors of childhood cancer. The CDC HRQOL–4 did not measure many of the subscales in the Impact of Cancer Scale, and the findings of this study may not provide a full examination of HRQOL among CCS. Finally, the sample size, particularly for underrepresented subgroups of CCS, was small.
Implications for Nursing
The relevance and implications of this study’s findings support the need for continued screening of CCS, particularly in women, with the use of well-established distress and psychosocial assessment tools, and to follow scheduled screenings as recommended by the Children’s Oncology Group (2018) Long-Term Follow-Up Guidelines for adverse psychosocial and quality of life effects. Of particular concern are the findings that young adult female CCS reported a significantly greater number of “no days” in which they reported good physical, mental, and general health compared to male CCS, adult cancer survivors, and the general population. Depression and poor general health are associated with suicidal ideation among CCS (Recklitis et al., 2010). Ernst et al. (2020) found that suicidal ideation was most closely related to social and psychological factors, concurrent distress symptoms (depression, anxiety, social phobia), previous suicide attempts, current loneliness, and present living situation. Screening young adult female CCS for depression and poor health should be a routine part of survivorship care, given their relationship with suicidal ideation. These findings support the need to develop and test for targeted interventions to improve HRQOL among these survivors, and suggest the need for continued research examining racial disparities for health outcomes in young adult CCS.
Conclusion
Evidence for poorer HRQOL outcomes among young adult female CCS continues to highlight them as an at-risk group. The results of this study demonstrate poorer physical, mental, and general health for young adult female CCS compared to young adult male CCS, healthy young adult females, female survivors of adult cancer, and the general population with no history of cancer. These results highlight a bleak trajectory for young adult female CCS HRQOL in long-term survivorship. Depressive symptoms among these young adult female CCS should be of particular concern for healthcare providers. These CCS require routine screening for assessment and treatment of mental health functioning to decrease risk of self-harming behaviors.
About the Authors
Mary Ann Cantrell, PhD, RN, CNE, ANEF, FAAN, is a professor and PhD program director in the Fitzpatrick College of Nursing, and Michael A. Posner, PhD, PStat®, is an associate professor of statistics and data science in the Department of Mathematics and Statistics, both at Villanova University in Pennsylvania. No financial relationships to disclose. Cantrell contributed to the conceptualization and design. Posner completed the data collection and contributed to the manuscript preparation. Both authors provided statistical support and analysis. Cantrell can be reached at mary.ann.cantrell@villanova.edu, with copy to ONFEditor@ons.org. (Submitted June 2021. Accepted December 20, 2021.)
References
Alderfer, M.A., Labay, L.E., & Kazak A.E. (2003). Brief report: Does posttraumatic stress apply to siblings of childhood cancer survivors? Journal of Pediatric Psychology, 28(4), 281–286. https://doi.org/10.1093/jpepsy/jsg016
Aili, K., Arvidsson, S., & Nygren, J.M. (2021). Health related quality of life and buffering factors in adult survivors of acute pediatric lymphoblastic leukemia and their siblings. Health and Quality of Life Outcomes, 19, 55. https://doi.org/10.1186/s12955-021-01700-4
American Cancer Society. (2022). Cancer Statistics Center. Retrieved April 2, 2022 from http://cancerstatisticscenter.cancer.org
Andresen, E.M., Catlin, T.K., Wyrwich, K.W., & Jackson-Thompson, J. (2003). Retest reliability of surveillance questions on health related quality of life. Journal of Epidemiology and Community Health, 57(5), 339–343. https://doi.org/10.1136/jech.57.5.339
Armstrong, G.T., Sklar, C.A., Hudson, M.M., & Robison, L.L. (2007). Long-term health status among survivors of childhood cancer: Does sex matter? Journal of Clinical Oncology, 25(28), 4477–4489. https://doi.org/10.1200/JCO.2007.11.2003
Barrett, P.M., Mullen, L., & McCarthy, T. (2020). Enduring psychological impact of childhood cancer on survivors and their families in Ireland: A national qualitative study. European Journal of Cancer Care, 29(5), E13275. https://doi.org/10.1111/ecc.13257
Buchbinder, D., Casillas, J., Krull, K.R., Goodman, P., Leisenring, W., Recklitis, C., . . . Zeltzer, L.K. (2010). Psychological outcomes of siblings of cancer survivors: A report from the Childhood Cancer Survivor Study. Psycho-Oncology, 20(12), 1259–1268. https://doi.org/10.1002/pon.1848
Cantrell, M.A., & Posner, M.A. (2014). Psychological distress between young adult female survivors of childhood cancer and matched female cohorts surveyed in the Adolescent Health Study. Cancer Nursing, 37(4), 271–277. https://doi.org/10.1097/NCC.0000000000000105
Casillas, J.N., Zebrack, B.J., & Zeltzer, L.K. (2006). Health-related quality of life for Latino survivors of childhood cancer. Journal of Psychosocial Oncology, 24(3), 125–145. https://doi.org/10.1300/J077v24n03_06
Centers for Disease Control and Prevention. (2022). Behavioral risk factor surveillance system. U.S. Department of Health and Human Services. Retrieved May 10, 2020, from https://www.cdc.gov/brfss/index.html
Cherepanov, D., Palta, M., & Fryback, D.G. (2010). Underlying dimensions of the five health-related quality-of-life measures used in utility assessment: Evidence from the National Health Measurement Study. Medical Care, 48(8), 718–725. https://doi.org/10.1097/MLR.0b013e3181e35871
Children’s Oncology Group. (2018). Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancer [v.5.0]. http://www.survivorshipguidelines.org/pdf/2018/COG_LTFU_Guidelines_v5.p…
Choi, K.W., Chen, C.Y., Stein, M.B., Klimentidis, Y.C., Wang, M.J., Koenen, K.C., & Smoller, J.W. (2019). Assessment of bidirectional relationships between physical activity and depression among adults: A 2-Sample Mendelian randomization study. JAMA Psychiatry, 76(4), 399–408. https://doi.org/10.1001/jamapsychiatry.2018.4175
CureSearch for Children’s Cancer. (2020, April 15). Childhood cancer statistics. https://curesearch.org/childhood-cancer-statistics
Ernst, M., Brähler, E., Wild, P.S., Jünger, C., Faber, J., Schneider, A., & Beutel, M.E. (2020). Risk factors for suicidal ideation in a large, registry-based sample of adult long-term childhood cancer survivors. Journal of Affective Disorders, 265, 351–356. https://doi.org/10.1016/j.jad.2020.01.080
Ferrans, C.E., Zerwic, J.J., Wilbur, J.E., & Larson, J.L. (2005). Conceptual model of health-related quality of life. Journal of Nursing Scholarship, 37(4), 336–342. https://doi.org/10.1111/j.1547-5069.2005.00058.x
Hayek, S., Gibson, T.M., Leisenring, W.M., Guida, J.L., Gramatges, M.M., Lupo, P.J., . . . Ness, K.K. (2020). Prevalence and predictors of frailty in childhood cancer survivors and siblings: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 38(3), 232–247. https://doi.org/10.1200/JCO.19.01226
Houtzager, B.A., Oort, F.J., Hoekstra-Weebers, J.E.H.M., Caron, H.N., Grootenhuis, M.A., & Last, B.F. (2004). Coping and family functioning predict longitudinal psychological adaptation of siblings of childhood cancer patients. Journal of Pediatric Psychology, 29(8), 591–605. https://doi.org/10.1093/jpepsy/jsh061
Kapp, J.M., Jackson-Thompson, J., Petroski, G.F., & Schootman, M. (2009). Reliability of health-related quality-of-life indicators in cancer survivors from a population-based sample, 2005, BRFSS. Public Health, 123(4), 321–325. https://doi.org/10.1016/j.puhe.2008.10.005
Leisenring, W.M., Mertens, A.C., Armstrong, G.T., Stovall, M.A., Neglia, J.P., Lanctot, J.Q., . . . Yasui, Y. (2009). Pediatric cancer survivorship research: Experience of the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 27(14), 2319–2327. https://doi.org/10.1200/JCO.2008.21.1813
Lie, H.C., Mellblom, A.V., Brekke, M., Finset, A., Fosså, S.D., Kiserud, C.E., . . . Loge, J.J. (2017). Experiences with late effects-related care and preferences for long-term follow-up care among adult survivors of childhood lymphoma. Supportive Care in Cancer, 25(8), 2445–2454. https://doi.org/10.1007/s00520-017-3651-6
Lund, L.W., Schmiegelow, K., Rechnitzer, C., & Johansen C.A. (2010). A systematic review of studies on psychosocial late effects of childhood cancer: Structures of society and methodological pitfalls may challenge the conclusions. Pediatric Blood and Cancer, 56(4), 532–543. https://doi.org/10.1002/pbc.22883
Miller, K.D., Nogueira, L., Mariotto, A.B., Rowland, J.H., Yabroff, K.R., Alfano, C.M., . . . Siegel, R.L. (2019). Cancer treatment and survivorship statistics, 2019. CA: A Cancer Journal for Clinicians, 69(5), 363–385. https://doi.org/10.3322/caac.21565
Ness, K.K., Hudson, M.M., Ginsberg, J.P., Nagarajan, R., Kaste, S.C., Marina, N., . . . Gurney, J.G. (2009). Physical performance limitations in the Childhood Cancer Survivor Study cohort. Journal of Clinical Oncology, 27(14), 2382–2389. https://doi.org/10.1200/JCO.2008.21.1482
Phillips, S.M., Padgett, L.S., Leisenring, W.M., Stratton, K.K., Bishop, K., Krull, K.R., . . . Mariotto, A.B. (2015). Survivors of childhood cancer in the United States: Prevalence and burden of morbidity. Cancer Epidemiology, Biomarkers and Prevention, 24(4), 653–663. https://doi.org/10.1158/1055-9965.EPI-14-1418
Phillips-Salimi, C.R., Lommel, K., & Andrykowski, M.A. (2011). Physical and mental health status and health behaviors of childhood cancer survivors: Findings from the 2009 BRFSS survey. Pediatric Blood and Cancer, 58(6), 964–970. https://doi.org/10.1002/pbc.23359
Recklitis, C.J., Diller, L.R., Li, X., Najita, J., Robison, L.L., & Zeltzer, L. (2010). Suicide ideation in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 28(4), 655–661. https://doi.org/10.1200/JCO.2009.22.8635
Rosales, P., Evangelista, L., Guo, Y., Agbayani, C.J.G., Kain, Z.N., & Fortier, M.A. (2021). Exploring differences in perceived satisfaction, resilience, and achievement between Hispanic and Non-Hispanic White childhood cancer survivors. Journal of Pediatric Health Care, 35(2), 196–204. https://doi.org/10.1016/j.pedhc.2020.10.003
van Erp, L.M.E., Maurice-Stam, H., Kremer, L.C.M., Tissing, W.J.E., van der Pal, H.J.H., de Vries, A.C.H., . . . Grootenhuis, M.A. (2021). Health-related quality of life in Dutch adult survivors of childhood cancer: A nation-wide cohort study. European Journal of Cancer, 152, 204–214. https://doi.org/10.1016/j.ejca.2021.04.033
Vuotto, S.C., Krull, K.R., Li, C., Oeffinger, K.C., Green, D.M., Patel, S.K., . . . Brinkman, T.M. (2017). Impact of chronic disease on emotional distress in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer, 123(3), 521–528. https://doi.org/10.1002/cncr.30348
Ward, E., DeSantis, C., Robbins, A., Kohler, B., & Jemal, A. (2014). Childhood and adolescent cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 64(2), 83–103. https://doi.org/10.3322/caac.21219
Warner, E.L., Nam, G.E., Zhang, Y., McFadden, M., Wright, J., Spraker-Perlman, H., . . . Kirchhoff, A.C. (2016). Health behaviors, quality of life, and psychosocial health among survivors of adolescent and young adult cancers. Journal of Cancer Survivorship, 10(2), 280–290. https://doi.org/10.1007/s11764-015-0474-7
Wilson, C.L., Brinkman, T.M., Cook, C., Huang, S., Hyun, G., Green, D.M., . . . Hudson, M.L. (2020). Clinically ascertained health outcomes, quality of life, and social attainment among adult survivors of neuroblastoma: A report from the St. Jude Lifetime Cohort. Cancer, 126(6), 1330–1338. https://doi.org/10.1002/cncr.32678
Wilson, I.B., & Cleary, P.D. (1995). Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA, 273(1), 59–65. https://doi.org/10.1001/jama.1995.03520250075037
Wu, E., Robison, L.L., Jenney, M.E.M., Rockwood, T.H., Feusner, J., Friedman, D., . . . Bhatia, S. (2007). Assessment of health-related quality of life of adolescent cancer patients using the Minneapolis-Manchester Quality of Life Questionnaire. Pediatric Blood and Cancer, 48(7), 678–686. https://doi.org/10.1002/pbc.20874
Yağc-Küpeli, B., Akyüz, C., Küpeli, S., & Büyükpamukçu, M. (2012). Health-related quality of life in pediatric cancer survivors: A multifactorial assessment including parental factors. Journal of Pediatric Hematology/Oncology, 34(3), 194–199. https://doi.org/10.1097/mph.0b013e3182467f5f
Zebrack, B.J. (2009). Developing a new instrument to assess the impact of cancer in young adult survivors of childhood cancer. Journal of Cancer Survivorship, 3(3), 174–180. doi:10.1007/s11764-009-0087-0
Zeltzer, L.K., Recklitis, C., Buchbinder, D., Zebrack, B., Casillas, J., Tsao, J.C., . . . Krull, K. (2009). Psychological status in childhood cancer survivors: A report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology, 27(14), 2396–2404. https://doi.org/10.1200/JCO.2008.21.1433
Zullig, K.J., Valois, R.F., Huebner, E.S., & Drane, J.W. (2004). Evaluating the performance of the Centers for Disease Control and Prevention core Health-Related Quality of Life Scale with adolescents. Public Health Reports, 119(6), 577–584.


