Critical Event Debriefing: Impacts on Clinical Practice and Implications for Oncology Nurses
Background: The complexity of caring for patients with cancer has a direct impact on oncology nurses. When a patient with cancer experiences a critical health event, oncology nurses may have concerns about their ability to provide high-quality care for patients in the current healthcare environment. These concerns can negatively affect nurses’ emotional well-being and lead to compassion fatigue and burnout.
Objectives: This article aims to examine critical event debriefing and identify ways oncology nurses can implement a critical event debriefing framework into their clinical practice.
Methods: A literature search was conducted in CINAHL® and PubMed® databases for articles related to critical event debriefing and compassion fatigue and burnout among oncology nurses. A case study demonstrates the use of critical event debriefing on an oncology unit.
Findings: Critical event debriefing frameworks can enhance teamwork, help initiate process improvements, and offer psychological support to improve emotional well-being. Additional research is needed about the use of critical event debriefing as a solution to compassion fatigue and burnout among oncology nurses.
Jump to a section
Earn free contact hours: Click here to connect to the evaluation. Certified nurses can claim no more than 1 total ILNA point for this program. Up to 1 ILNA point may be applied to Professional Practice/Performance. See www.oncc.org for complete details on certification.
Oncology care is increasing in complexity because of a multitude of factors. Patients with cancer are being offered a wider range of treatments with higher levels of intensity, often at older ages when multiple comorbidities are present and at later stages of disease (Ferreyro & Munshi, 2019). However, this treatment model has led to new and more severe complications (Ferreyro & Munshi, 2019; Schellongowski et al., 2016). Patients experiencing complications related to cancer account for about four million emergency department visits per year in the United States. Of those visits, about one-third lead to a hospital admission (Hsu et al., 2018). Patients with cancer also use more time and resources in the emergency department because of their higher acuity levels on presentation (Hsu et al., 2018). Patients with hematologic malignancies or solid tumors frequently require intensive care to manage complications from the disease or its treatment, such as organ failure from an infiltrating tumor or organ toxicity from a cancer drug (Schellongowski et al., 2016). In the current healthcare system, the emergency department is pressured to limit overcrowding by efficiently transferring patients to inpatient units (Hammer et al., 2022), and the intensive care unit must carefully evaluate potential admissions before accepting them from inpatient units (Ferreyro & Munshi, 2019; Schellongowski et al., 2016). This can lead to oncology units being filled with high-acuity patients.
Oncology nurses, like all healthcare providers, face a great deal of stress. Data show that healthcare providers who specialize in oncology face even greater degrees of stress than those who work in other specialties, which may increase their risk of burnout (Gribben & Semple, 2021). Burnout occurs when an individual experiences low energy, low personal accomplishment, and negative feelings about their job (World Health Organization, 2019). When work-related stress becomes so constant that nurses start to experience undesirable consequences, such as burnout, fear, or insomnia, it can lead to compassion fatigue (Algamdi, 2022). While experiencing compassion fatigue and burnout, oncology nurses are no longer getting pleasure out of being a service provider, which has a negative impact on their emotional well-being (Algamdi, 2022).
The heightened level of stress in oncology can be largely attributed to the widespread nursing shortage and the many challenges nurses manage with their workload when caring for complex, high-acuity patients (Gribben & Semple, 2021). Oncology nurses also assist with the emotional challenges faced by patients, including fear of the unknown, bad news about a diagnosis, and the ever-present need to make complicated decisions (Gribben & Semple, 2021). In addition, because of the nature of oncology as a rapidly evolving field, oncology nurses continuously educate themselves to keep abreast of clinical updates (Gribben & Semple, 2021). They do this while also providing compassionate, holistic care to patients who are experiencing a great deal of pain and can be at high risk for experiencing a critical or traumatic event. To cope with these heavy and numerous burdens, oncology nurses require evidence-based approaches. One approach is to routinely conduct debriefing sessions after critical events.
Clinical debriefing is a way for the healthcare team to review and process a critical event that just occurred (Toews et al., 2021). Common critical events in patients with cancer are most often related to adverse effects of cancer therapies, new symptoms of a previously undiagnosed malignancy, progression of a known disease, or disease recurrence (Gould Rothberg et al., 2022). The critical events that occur because of patient complications are usually acute respiratory failure, sepsis requiring vasopressor support, or cardiac arrest (Bruckel et al., 2017; Schellongowski et al., 2016). Of note, about 14% of all in-hospital cardiac arrests occur in patients with advanced cancer (Bruckel et al., 2017). The American Heart Association Guidelines for CPR and Emergency Cardiovascular Care recommend critical event debriefing for healthcare providers involved in a resuscitation attempt to provide support, review team performance, and discover areas for improvement (Berg et al., 2020; Panchal et al., 2020).
Purpose
The purpose of this article is to summarize the literature about the role of clinical debriefing after critical events and outline a framework for oncology nurses to implement critical event debriefing into their clinical practice. In addition, a case study illustrates the use of debriefing on an oncology unit.
Methods
A review of the literature was performed using CINAHL® and PubMed® databases. The following key search terms were used: debriefing, critical event, oncology, nursing, compassion fatigue, and burnout. Studies published in English from 2012 to 2022 were included. Because clinical debriefing can occur in all areas of the hospital, the settings and populations considered for inclusion were any hospital department serving any patient population. Studies focusing on clinical debriefing that occurred outside of the hospital, such as with EMTs or paramedics, were excluded.
Findings
In total, 16 studies were identified that focused on the impacts of debriefing after critical events, and 5 of these studies described specific debriefing frameworks. Four studies focused on compassion fatigue and burnout among oncology nurses. No studies were found that focused on debriefing after critical events to prevent compassion fatigue or burnout in oncology nurses. The details of the included studies are presented in Table 1.
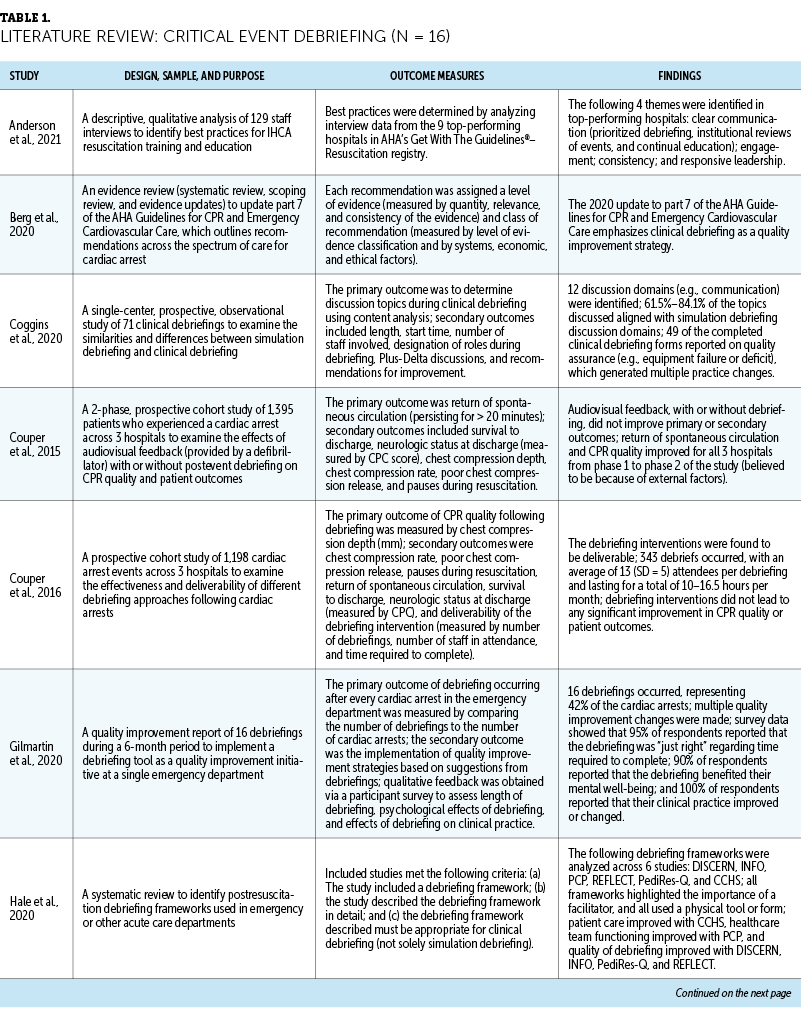
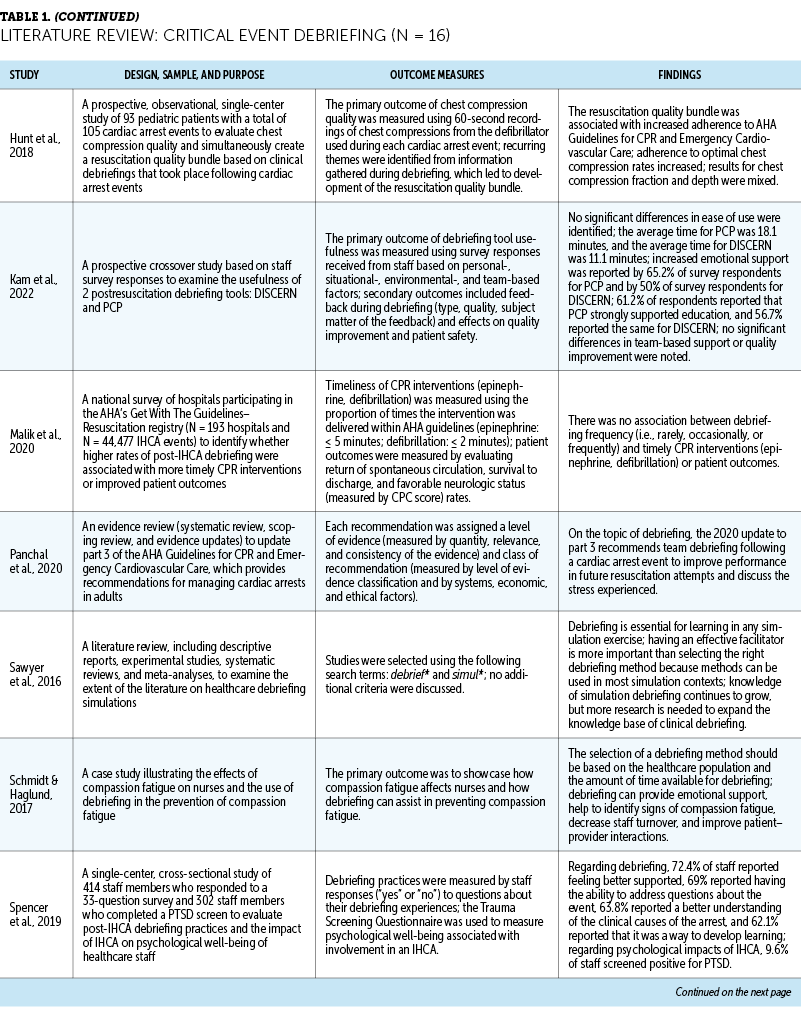
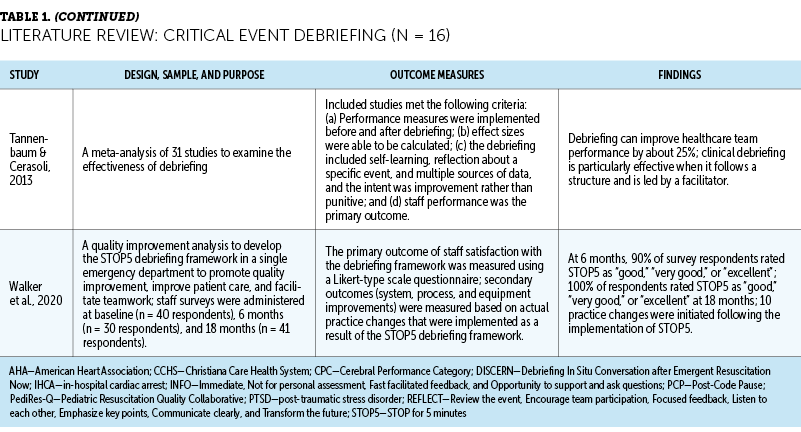
Many researchers who study the process of debriefing after critical events focus specifically on in-hospital cardiac arrest and how debriefing after the event affects patient outcomes (e.g., return of spontaneous circulation, patient survival), as well as the quality of future resuscitation attempts (e.g., efficiency of interventions, chest compression quality) (Anderson et al., 2021; Couper et al., 2015, 2016; Malik et al., 2020). Other potential effects of debriefing that are often studied include adherence to American Heart Association guidelines, awareness of the need to update or change established protocols or equipment, and emotional support for staff (Coggins et al., 2020; Gilmartin et al., 2020; Hunt et al., 2018; Kam et al., 2022; Spencer et al., 2019).
Debriefing Frameworks
Critical event debriefing frameworks are usually multistep processes, with a leader who guides the discussion similar to a team leader during a code. Establishing a leader to facilitate the conversation and providing them with a script or visual aids were reported as the most effective approaches to critical event debriefing (Hale et al., 2020; Sawyer et al., 2016; Tannenbaum & Cerasoli, 2013). When led by a facilitator and approached using a well-developed structure, debriefing can improve healthcare team performance by about 25% (Tannenbaum & Cerasoli, 2013).
Although there is an abundance of literature on the use of debriefing frameworks in simulation, research on such frameworks in the clinical setting is less common (Coggins et al., 2020; Sawyer et al., 2016). This may be because clinical debriefing has to be tailored to the healthcare providers involved, the event itself, and the amount of time available to conduct a debriefing (Schmidt & Haglund, 2017), which can make some institutions hesitant to investigate the use of debriefing.
A few debriefing frameworks have been developed specifically for real-world situations and can be widely used. STOP5 is a debriefing framework that enables healthcare workers to have a structured dialogue immediately following a critical event (Walker et al., 2020) (see Figure 1). This framework is highly rated by its users and has been shown to help initiate practice changes to improve quality (Walker et al., 2020). In addition, the STOP5 framework is a mnemonic, which makes it easy for anyone to use and does not require specialized training for use. It calls on staff involved in the event to stop for five minutes to summarize what happened, discuss things that went well and opportunities for improvement, and point to future actions that will help ensure those improvements can be attained (Walker et al., 2020). Gilmartin et al. (2020) studied a similar debriefing framework called the hot debriefing tool, which was effective in helping staff feel a sense of psychological well-being following a critical event and identify areas for improvement in their handling of critical events. All users of the hot debriefing tool reported that their clinical practice had improved after participating in a hot debrief, which is a debriefing that occurs immediately following a critical event (Gilmartin et al., 2020). Another debriefing model, the Post-Code Pause, was found to be effective at identifying areas for improvement and addressing stress or psychological trauma that can result from being involved in a critical health event (Hale et al., 2020; Kam et al., 2022).

Debriefing After Critical Events
Although published literature evaluating the impact of debriefing on patient outcomes or CPR quality is limited (Couper et al., 2015, 2016; Malik et al., 2020), there is quite a bit of evidence to support the practice of critical event debriefing to enhance staff satisfaction, performance, and well-being. Staff who are involved in a debriefing feel more supported by their colleagues, appreciate having the opportunity to address questions that come up after an incident, and think of debriefing as a meaningful learning experience that enables them to better understand the clinical picture (Spencer et al., 2019). In addition to providing needed emotional support, debriefing also allows for the identification of gaps in care or deficiencies in standard operating procedures and highlights areas for quality improvement at the individual, group, and system levels (Coggins et al., 2020; Gilmartin et al., 2020; Kam et al., 2022). Debriefings that are led by a facilitator, include all staff members involved in the critical event, and focus on personal challenges experienced by staff during the event have been found to increase adherence to established CPR guidelines from the American Heart Association (Hunt et al., 2018).
Of note, debriefing sessions are easy to implement, are relatively inexpensive, and do not take much time to complete, with the average session lasting 5–18 minutes (Couper et al., 2016; Kam et al., 2022; Tannenbaum & Cerasoli, 2013). In addition, among hospitals with the best resuscitation performance records, healthcare staff acknowledge that critical event debriefing is a top priority (Anderson et al., 2021). Anderson et al. (2021) also acknowledged a general preference for a coordinated, interprofessional approach to the debriefing process instead of the asynchronous, departmentally stratified approach that is often used and believed to be less effective in improving teamwork. In the latter approach, each discipline debriefs separately, and they infrequently debrief immediately after a critical event because of other clinical responsibilities (Anderson et al., 2021).
Debriefing Applications for Clinical Oncology Critical Events
The number of patients with cancer with critical illness has increased because novel cancer treatments are being selected for a greater number of patients, including older adult patients and patients with poor functional status (Ferreyro & Munshi, 2019). Because of the rapid advances in treatment options, caring for patients who are critically ill is rarely straightforward and requires providers to have an expansive knowledge base and be prepared for adverse outcomes, such as respiratory failure and cardiac arrest (Bruckel et al., 2017; Ferreyro & Munshi, 2019). Adverse outcomes among patients in the oncologic and hematologic populations can be particularly challenging for healthcare providers because survival rates for these patients are lower than those for the general patient population (Bruckel et al., 2017; Ferreyro & Munshi, 2019). With formal debriefing, staff can gain a better understanding of the situation, evaluate and respond to the varied emotions they may be experiencing, and have better support as they return to patient care (American Association of Nurse Anesthesiology, 2014).
There is a substantial lack of research on the topic of critical event debriefing in oncology settings. However, there is a growing body of evidence focusing on the high prevalence of compassion fatigue and burnout among oncology nurses (Algamdi, 2022; Ortega-Campos et al., 2020). Nurses who care for patients with cancer are continually exposed to emotionally challenging situations, which can lead to the development of compassion fatigue and burnout (Ortega-Campos et al., 2020). Oncology nurses report experiencing compassion fatigue more often than compassion satisfaction (Algamdi, 2022). An exceptionally heavy workload, staffing shortages, continual exposure to profound distress, and high patient acuity all contribute to oncology nurse burnout (Gribben & Semple, 2021).
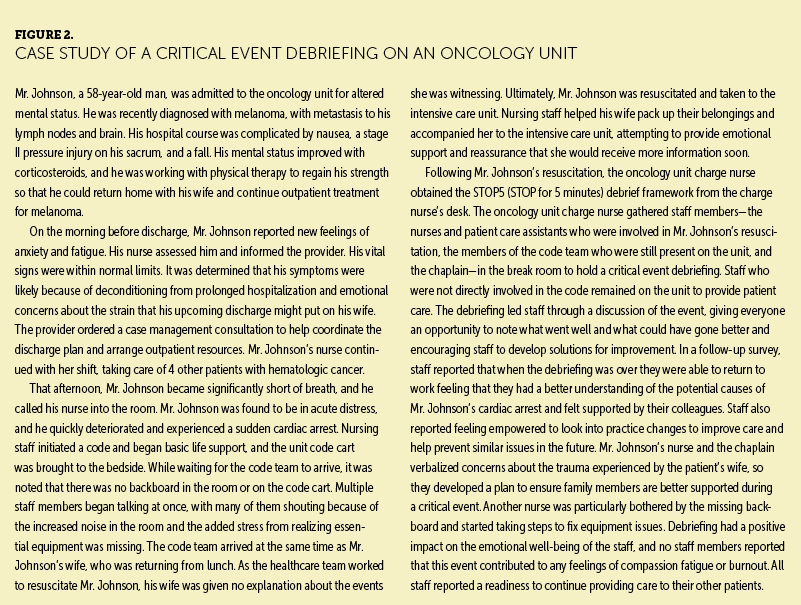
When a critical event such as a cardiac arrest takes place, nurses have expressed that there is a need for reassurance, validation, and education about the event to establish a shared understanding of what happened (Clark & McLean, 2018). This can be accomplished through formal debriefing. When nurses debrief following an emotionally challenging critical event, a significantly distressing experience can turn into a positive learning experience (Clark & McLean, 2018). Compassion fatigue and burnout can be reduced when nurses have the opportunity to gain a sense of clarity regarding their thoughts and emotions (Ortega-Campos et al., 2020), and critical event debriefing can provide such an opportunity. Figure 2 presents a case study to demonstrate the challenges faced by oncology nurses and how the use of clinical debriefing after critical events can help to mitigate the negative effects of those challenges.
Discussion
Although data on debriefing in oncology practice are limited, the strong foundation for debriefing in health care can be readily applied to clinical oncology. Clinical oncology settings, some of the most complex settings in any healthcare institution, need ways to reduce nurse burnout and promote psychological and emotional wellness to retain nursing staff (Gribben & Semple, 2021). Emotional well-being is frequently cited as a positive outcome of critical event debriefing (Gilmartin et al., 2020; Kam et al., 2022; Schmidt & Haglund, 2017).
Oncology nurses are responsible for safely managing the unique needs of their patients while also closely and continuously monitoring for signs of deterioration. Therefore, when a critical event involving a patient with cancer occurs, critical event debriefing is needed to examine all the moving pieces and make sense of what happened. Debriefing provides opportunities to ask questions and learn from the experience (Spencer et al., 2019). The knowledge gained from critical event debriefing can be used during future high-intensity situations (Schmidt & Haglund, 2017). Critical event debriefing also offers an opportunity to create meaningful practice changes that can improve clinical practice (Gilmartin et al., 2020). In addition, debriefing provides oncology nurses with tools to build personal resilience and a more stable workforce—two key components for combating burnout (Gribben & Semple, 2021).
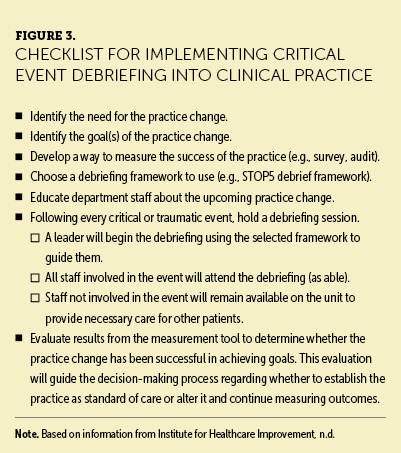
Institutions can implement a formal debriefing framework to use following critical or traumatic events for minimal cost, time, and education. Important components to include when debriefing are as follows: Each debriefing has a leader, such as the unit charge nurse; participants in the debriefing include any staff member involved in the event; and the debriefing is structured. Debriefing can last from 5 to 20 minutes. This practice change can be approached using the Model for Improvement, a quality improvement framework used by many healthcare institutions because of its simplicity and high utility (Institute for Healthcare Improvement, n.d.). This framework helps to establish goals for a quality improvement project and determine ways to measure whether the practice change has been successful in achieving those goals (Institute for Healthcare Improvement, n.d.). The nursing team implementing the change decides on a goal (e.g., improving emotional well-being), develops a way to measure whether this goal was achieved (e.g., a postimplementation staff survey to assess improvements in emotional well-being after three months of regular use of the critical event debriefing tool), and begins using the selected clinical debriefing tool after any critical event occurs (see Figure 3). Using the information obtained from postimplementation surveys, the nursing team can decide whether the debriefing tool has been successful in achieving the predetermined goals or whether it needs to be adjusted.
Implications for Practice and Research
The positive effects of clinical debriefing on emotional well-being, teamwork, and process enhancement indicate that it plays an important role in oncology nursing to improve clinical practice. More research is needed about critical event debriefing in oncology settings to evaluate how debriefing can most effectively improve emotional well-being and reduce problems such as compassion fatigue and burnout. Critical event debriefing frameworks have been shown to be effective and easy to implement, but their use has not been studied on hematology or oncology units specifically. Future studies are needed on compassion fatigue and burnout among oncology nurses that focus on clinical debriefing as a means to reduce these potential adverse effects and keep oncology nurses engaged in the care of patients with cancer.
Conclusion
As the treatment landscape evolves and patients live longer with cancer, oncology nursing will continue to be a challenging specialty. Meeting these challenges with adequate protective measures can ensure that oncology nurses feel supported to perform their jobs at a high level and maintain their emotional well-being by preventing adverse outcomes such as compassion fatigue or burnout. Debriefing after a patient experiences a critical or traumatic event offers many protective measures for nurses, such as better emotional support, enhanced teamwork, and continual opportunities to improve their practice environment.
About the Authors
Molly Joyce, MSN, APRN, OCN®, is an instructor in nursing in the School of Nursing at Vanderbilt University in Nashville, TN; and Joanne Itano, RN, PhD, is a retired associate professor in the School of Nursing at the University of Hawaii at Manoa in Honolulu. The authors take full responsibility for this content. The authors were participants in the Clinical Journal of Oncology Nursing Writing Mentorship Program. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Joyce can be reached at tuckerme50@gmail.com, with copy to CJONEditor@ons.org. (Submitted March 2023. Accepted September 12, 2023.)
References
Algamdi, M. (2022). Prevalence of oncology nurses’ compassion satisfaction and compassion fatigue: Systematic review and meta-analysis. Nursing Open, 9(1), 44–56. https://doi.org/10.1002/nop2.1070
American Association of Nurse Anesthesiology. (2014). Guidelines for critical incident stress management. https://issuu.com/aanapublishing/docs/3_-_guidelines_for_critical_incid…
Anderson, T.M., Secrest, K., Krein, S.L., Schildhouse, R., Guetterman, T.C., Harrod, M., . . . Nallamothu, B.K. (2021). Best practices for education and training of resuscitation teams for in-hospital cardiac arrest. Circulation: Cardiovascular Quality and Outcomes, 14(12), e008587. https://doi.org/10.1161/CIRCOUTCOMES.121.008587
Berg, K.M., Cheng, A., Panchal, A.R., Topjian, A.A., Aziz, K., Bhanji, F., . . . Lavonas, E.J. (2020). Part 7: Systems of care: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(16, Suppl. 2), S580–S604. https://doi.org/10.1161/CIR.0000000000000899
Bruckel, J.T., Wong, S.L., Chan, P.S., Bradley, S.M., & Nallamothu, B.K. (2017). Patterns of resuscitation care and survival after in-hospital cardiac arrest in patients with advanced cancer. Journal of Oncology Practice, 13(10), e821–e830. https://10.1200/JOP.2016.020404
Clark, R., & McLean, C. (2018). The professional and personal debriefing needs of ward based nurses after involvement in a cardiac arrest: An explorative qualitative pilot study. Intensive and Critical Care Nursing, 47, 78–84. https://doi.org/10.1016/j.iccn.2018.03.009
Coggins, A., De Los Santos, A., Zaklama, R., & Murphy, M. (2020). Interdisciplinary clinical debriefing in the emergency department: An observational study of learning topics and outcomes. BMC Emergency Medicine, 20(1), 79. https://doi.org/10.1186/s12873-020-00370-7
Couper, K., Kimani, P.K., Abella, B.S., Chilwan, M., Cooke, M.W., Davies, R.P., . . . Perkins, G.D. (2015). The system-wide effect of real-time audiovisual feedback and postevent debriefing for in-hospital cardiac arrest: The cardiopulmonary resuscitation quality improvement initiative. Critical Care Medicine, 43(11), 2321–2331. https://10.1097/CCM.0000000000001202
Couper, K., Kimani, P.K., Davies, R.P., Baker, A., Davies, M., Husselbee, N., . . . Perkins, G.D. (2016). An evaluation of three methods of in-hospital cardiac arrest educational debriefing: The cardiopulmonary resuscitation debriefing study. Resuscitation, 105, 130–137. https://doi.org/10.1016/j.resuscitation.2016.05.005
Ferreyro, B.L., & Munshi, L. (2019). Acute respiratory failure in the oncologic patient: New era, new issues. In J.-L. Vincent (Ed.), Annual update in intensive care and emergency medicine 2019 (pp. 31–45). Springer. https://doi.org/10.1007/978-3-030-06067-1_3
Gilmartin, S., Martin, L., Kenny, S., Callanan, I., & Salter, N. (2020). Promoting hot debriefing in an emergency department. BMJ Open Quality, 9(3), e000913. https://10.1136/bmjoq-2020-000913
Gould Rothberg, B.E., Quest, T.E., Yeung, S.-C.J., Pelosof, L.C., Gerber, D.E., Seltzer, J.A., . . . Kyriacou, D.N. (2022). Oncologic emergencies and urgencies: A comprehensive review. CA: A Cancer Journal for Clinicians, 72(6), 570–593. https://doi.org/10.3322/caac.21727
Gribben, L., & Semple, C.J. (2021). Factors contributing to burnout and work–life balance in adult oncology nursing: An integrative review. European Journal of Oncology Nursing, 50, 101887. https://doi.org/10.1016/j.ejon.2020.101887
Hale, S.J., Parker, M.J., Cupido, C., & Kam, A.J. (2020). Applications of postresuscitation debriefing frameworks in emergency settings: A systematic review. Academic Emergency Medicine Education and Training, 4(3), 223–230. https://10.1002/aet2.10444
Hammer, C., DePrez, B., White, J., Lewis, L., Straughen, S., & Buchheit, R. (2022). Enhancing hospital-wide patient flow to reduce emergency department crowding and boarding. Journal of Emergency Nursing, 48(5), 603–609. https://doi.org/10.1016/j.jen.2022.06.002
Hsu, J., Donnelly, J.P., Moore, J.X., Meneses, K., Williams, G., & Wang, H.E. (2018). National characteristics of emergency department visits by patients with cancer in the United States. American Journal of Emergency Medicine, 36(11), 2038–2043. https://doi.org/10.1016/j.ajem.2018.03.025
Hunt, E.A., Jeffers, J., McNamara, L., Newton, H., Ford, K., Bernier, M., . . . Duval-Arnould, J. (2018). Improved cardiopulmonary resuscitation performance with CODE ACES2: A resuscitation quality bundle. Journal of the American Heart Association, 7(24), e009860. https://doi.org/10.1161/JAHA.118.009860
Institute for Healthcare Improvement. (n.d.). How to improve: Model for improvement. https://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
Kam, A.J., Gonsalves, C.L., Nordlund, S.V., Hale, S.J., Twiss, J., Cupido, C., . . . Parker, M.J. (2022). Implementation and facilitation of post-resuscitation debriefing: A comparative crossover study of two post-resuscitation debriefing frameworks. BMC Emergency Medicine, 22(1), 152. https://doi.org/10.1186/s12873-022-00707-4
Malik, A.O., Nallamothu, B.K., Trumpower, B., Kennedy, M., Krein, S.L., Chinnakondepalli, K.M., . . . Chan, P.S. (2020). Association between hospital debriefing practices with adherence to resuscitation process measures and outcomes for in-hospital cardiac arrest. Circulation: Cardiovascular Quality and Outcomes, 13(11), e006695. https://10.1161/CIRCOUTCOMES.120.006695
Ortega-Campos, E., Vargas-Román, K., Velando-Soriano, A., Suleiman-Martos, N., Cañadas-de la Fuente, G.A., Albendín-García, L., & Gómez-Urquiza, J.L. (2020). Compassion fatigue, compassion satisfaction, and burnout in oncology nurses: A systematic review and meta-analysis. Sustainability, 12(1), 72. https://doi.org/10.3390/su12010072
Panchal, A.R., Bartos, J.A., Cabañas, J.G., Donnino, M.W., Drennan, I.R., Hirsch, K.G., . . . Berg, K.M. (2020). Part 3: Adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(16, Suppl. 2), S366–S468. https://doi.org/10.1161/CIR.0000000000000916
Sawyer, T., Eppich, W., Brett-Fleegler, M., Grant, V., & Cheng, A. (2016). More than one way to debrief: A critical review of healthcare simulation debriefing methods. Simulation in Healthcare, 11(3), 209–217. https://doi.org/10.1097/sih.0000000000000148
Schellongowski, P., Sperr, W.R., Wohlfarth, P., Knoebl, P., Rabitsch, W., Watzke, H.H., Staudinger, T. (2016). Critically ill patients with cancer: Chances and limitations of intensive care medicine—A narrative review. European Society for Medical Oncology Open, 1(5), e000018. https://doi.org/10.1136/esmoopen-2015-000018
Schmidt, M., & Haglund, K. (2017). Debrief in emergency departments to improve compassion fatigue and promote resiliency. Journal of Trauma Nursing, 24(5), 317–322. https://10.1097/JTN.0000000000000315
Spencer, S.A., Nolan, J.P., Osborn, M., & Georgiou, A. (2019). The presence of psychological trauma symptoms in resuscitation providers and an exploration of debriefing practices. Resuscitation, 142, 175–181. https://doi.org/10.1016/j.resuscitation.2019.06.280
Tannenbaum, S.I., & Cerasoli, C.P. (2013). Do team and individual debriefs enhance performance? A meta-analysis. Human Factors, 55(1), 231–245. https://doi.org/10.1177/0018720812448394
Toews, A.J., Martin, D.E., & Chernomas, W.M. (2021). Clinical debriefing: A concept analysis. Journal of Clinical Nursing, 30(11–12), 1491–1501. https://doi.org/10.1111/jocn.15636
Walker, C.A., McGregor, L., Taylor, C., & Robinson, S. (2020). STOP5: A hot debrief model for resuscitation cases in the emergency department. Clinical and Experimental Emergency Medicine, 7(4), 259–266. https://doi.org/10.15441/ceem.19.086
World Health Organization. (2019). QD85 burnout. In International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/12918…

