The Formation of Stigma and Its Social Consequences on Chinese People Living With Lung Cancer: A Qualitative Study
Purpose: To explore the formation of stigma toward lung cancer and its social consequences for Chinese patients living with this diagnosis.
Participants & Setting: A purposive sample of 19 patients with lung cancer were recruited in the outpatient clinic of a tertiary cancer center in southern China.
Methodologic Approach: This is a descriptive qualitative study. Semistructured interviews were conducted to explore the formation of stigma toward lung cancer and its social consequences. Audio recordings were transcribed verbatim and coded by the thematic analysis approach.
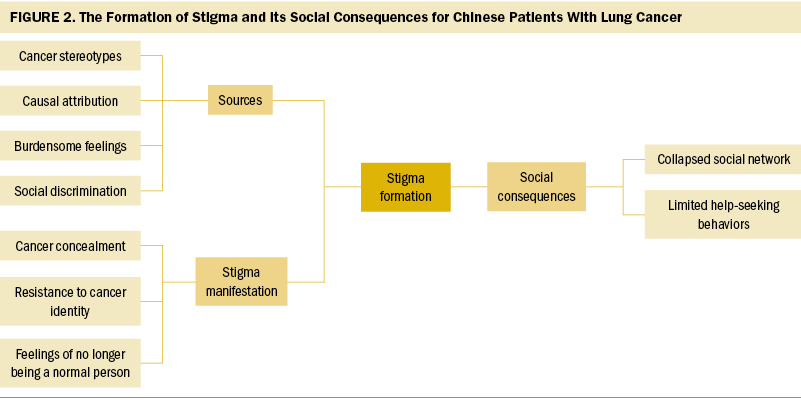
Findings: The following three themes emerged from interviews: (a) sources of stigma, (b) stigma manifestations, and (c) social consequences of stigma.
Implications for Nursing: Considering that the formation of lung cancer stigma is socioculturally specific, existing stereotypes and prejudice in Chinese society should be the focus of antistigma interventions at the population level. At the individual level, cancer concealment, resistance to cancer identity, and feelings of no longer being a normal person were three common manifestations that may be indicators for stigma screening among people with lung cancer. In addition, stigmas profoundly affected patients’ social lives and their help-seeking behaviors, and medical staff should use effective strategies to alleviate stigma toward lung cancer and its effects.
Jump to a section
Lung cancer is among the most common and aggressive cancers worldwide (Siegel et al., 2022). In 2020, it was estimated that 2.09 million new cases of lung cancer occurred, with about 1.76 million lung cancer deaths globally (Ferlay et al., 2020). With the implementation of effective tobacco control and health education, lung cancer incidence has decreased in some countries, like the United States (Siegel et al., 2022). However, lung cancer incidence in China is still increasing and high and is seen as a great threat to public health, with around 733,300 new cases diagnosed in China in 2015 (Yang et al., 2020). Patients with lung cancer often experience high levels of symptom burden (e.g., fatigue, shortness of breath, cough) and psychological distress (Morrison et al., 2017).
Goffman (1986) defined stigma as “an undesirable stereotype leading people to reduce the bearer from a whole and usual person to a tainted, discounted one” (pp. 2–3). It is well known that cancer is a highly stigmatized condition because of its association with death (Mosher & Danoff-Berg, 2007), negative body image (e.g., alopecia, weakness) (Rosman, 2004), and internal causal attribution (Ferrucci et al., 2011). Evidence has shown that lung cancer stigma is associated with self-blame and feelings of shame, and can even negatively affect patients’ help-seeking behaviors (Webb et al., 2019). Prior studies in Western countries have highlighted that lung cancer stigma stemmed from smoking denormalization. With the implementation of tobacco control campaigns, smoking has become an unethical behavior (Stuber et al., 2008). An investigation among 266 people with lung cancer in the United States showed that patients who had a smoking history reported significantly higher stigma compared to those who never smoked (Williamson et al., 2020). A previous study in the United Kingdom demonstrated that lung cancer attracted more public stigma than other cancer types because of its close association with smoking (Marlow et al., 2015). In addition, patients with lung cancer also reported blaming themselves and feeling deeply depressed because they often attributed their lung cancer diagnosis to their own faults (Ostroff et al., 2019; Weiss et al., 2017). To some extent, this may provide an explanation for the high level of psychological distress among patients with lung cancer. Experiencing stigma toward lung cancer is a burden for patients with this diagnosis, particularly in the Chinese culture, but limited studies demonstrate how the stigmatization came about in this culture. To date, China is the largest producer and consumer of tobacco in the world (Zhang et al., 2022). Contrary to smoking denormalization in other countries (Peretti-Watel et al., 2014; Rozin & Singh, 1999), cigarette smoking and gifting is still pervasive social etiquette in Chinese culture (Pan, 2004; Rich & Xiao, 2012). Despite that, previous research has indicated that the general Chinese population has a stronger public stigma toward lung cancer than individuals in the United Kingdom, particularly in the perception of severity and avoidance (Liu et al., 2018). Patients with lung cancer in China also reported a higher level of perceived stigma than patients with lung cancer in other countries (Liu et al., 2020). Based on the study of stigma theory by Yang and Kleinman (2008), the meanings, practices, and outcomes of stigma differ across cultures. Previous studies focused on the experience of lung cancer stigma and its associated effects on health, including a patient’s negative emotions, delayed behaviors related to seeking medical help, and altered patient–clinician relationships (Webb et al., 2019). However, limited existing evidence is available to give deep insight, particularly about the formation of stigma and its social consequences among Chinese patients living with lung cancer.
To date, it is well known that lung cancer stigma has a negative effect on patients’ psychological well-being (Chambers et al., 2012). However, there is a lack of research discussing stigma within a local cultural context. Therefore, this study aims to explore the formation of lung cancer stigma in China and its social consequences, which might provide theoretical evidence that will further interventional studies.
Methods
Study Design
This was a qualitative descriptive exploratory study based on phenomenology (Munhall, 2012) to explore the individual experience of Chinese patients with lung cancer regarding the stigma toward their disease through semistructured interviews. This approach recognized that the stigma experienced by patients with lung cancer embraces the interaction between individuals and their sociocultural contexts. Thematic analysis was used to generate results (Braun & Clarke, 2008). The Consolidated Criteria for Reporting Qualitative Research Checklist was used as a guideline for reporting qualitative research (Tong et al., 2007).
Participants and Setting
A purposive sample of 19 patients with lung cancer were recruited in the outpatient clinic at Sun Yat-sen University Cancer Center in Guangzhou, China, from June 2018 to January 2019. The inclusion criteria included the following: aged 18 years or older, had a primary lung cancer confirmed by pathology, received anticancer treatment, was fully aware of the diagnosis, understood the purpose of the study, and agreed to participate. Individuals with chronic infectious disease, mental illness, or cognitive impairment were excluded. To ensure the representation of the sample, the authors purposively selected participants for a variation of genders, smoking history, cancer stage, types of treatment, and time since diagnosis.
Data Collection
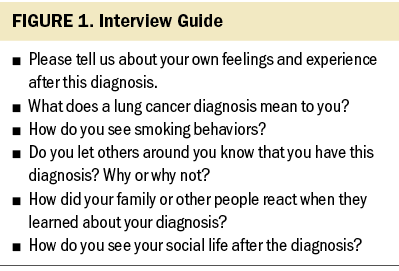
Participants who met the criteria were recommended by the clinical nurses to receive a brief introduction about this study. After obtaining informed consent, the eligible participants were invited into a quiet separate room for interviews. All semistructured interviews were conducted by the first author (X.L.), who had received formal qualitative interview training. To make the interview questions clear and easily understood, the interview guide was tested in a pilot study (see Figure 1). In addition, reflective journals were used throughout the research process; they were written by the researchers themselves to enhance the transparency of the research process and included their experiences, thoughts, and feelings. The interviews lasted between 30 and 45 minutes. The sample size was determined by data saturation, which meant no more new information was identified.
Data Analysis
All interviews were anonymized, audio recorded, and transcribed verbatim in Chinese. The transcripts were coded using the thematic analysis approach (Braun & Clarke, 2008). The following six phases were included: (a) data familiarization, (b) generating initial codes, (c) searching for themes, (d) reviewing themes, (e) defining and naming themes, and (f) producing the report. Initially, the researchers (X.L. and J.R.) listened to audio recordings repeatedly to familiarize themselves with the data and to check the transcripts for accuracy. The transcripts were then coded independently by X.L. and J.R. to generate initial codes, and axial coding was extracted and used to identify themes within the data. The data coded discordantly were discussed with the corresponding author (J.-E.Zh.) until a consensus was reached.
Ethical Consideration
Approval for this study was obtained from the ethics committee of Sun Yat-sen University Hospital. Before interviews, participants received oral and written information about the study’s aim and process. Potential participants were screened for eligibility and gave informed consent. Participants were guaranteed that all interviews were recorded anonymously, and they had the right to withdraw from the study at any time.
Rigor
To ensure credibility, the audio recordings were transcribed in a timely manner by X.L. and verified by the other researcher (J.R.), who was also responsible for recording and taking notes during interviews. Respondent validation techniques were applied to ensure the credibility of results. The generated themes were returned to three informative participants to check for consistency and resonance with their experience. To improve transferability, participants were selected purposively by various demographic and disease characteristics, and open-ended questions were used in all in-depth interviews. To ensure dependability, transcripts were read separately by X.L. and J.R. at least twice, and they were coded systematically to ensure that the core meanings of participants were conveyed accurately. Any disagreements were discussed with the corresponding author (J.-E.Zh.) to reach a final consensus. To achieve confirmability, the researchers followed the thematic analysis procedure rigorously without any prejudice.
Findings
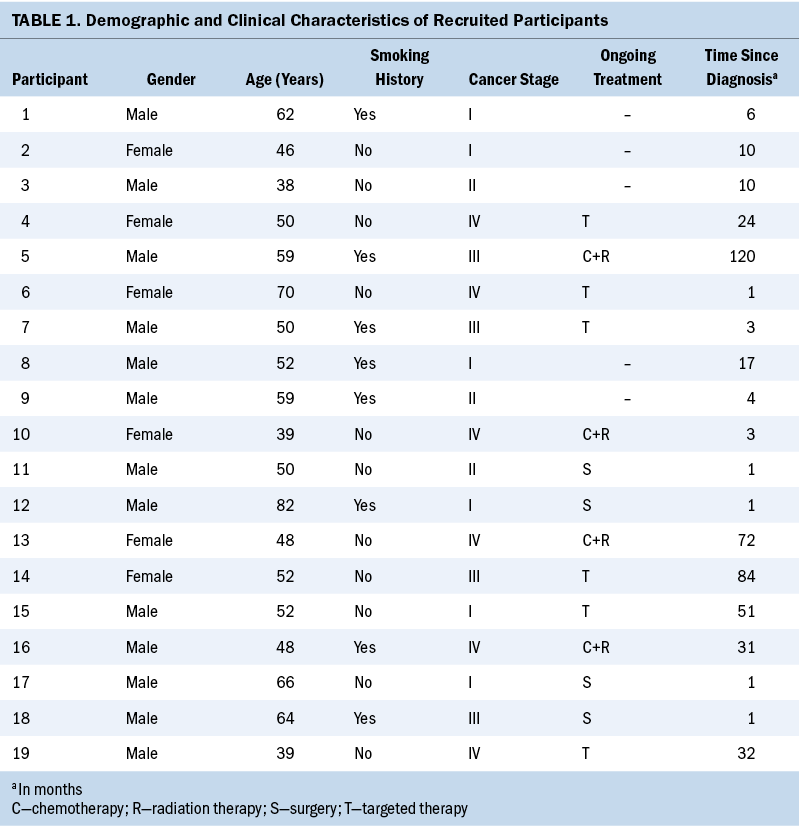
Twenty-one potential participants were approached. One declined to participate because of refusal to discuss any disease-related issues, and another declined by citing a lack of time. The final sample consisted of 19 patients with lung cancer (13 men and 6 women) with a median age of 52 years, ranging from 38 to 82 years. Eight participants had a smoking history, and the others were nonsmokers. The cancer stage, treatment status, and time since diagnosis were diverse to increase the representativeness of samples (see Table 1).
Three themes and nine subthemes were generated from interviews: (a) sources of stigma (subthemes were cancer stereotypes, causal attribution, burdensome feelings, and social discrimination); (b) stigma manifestations (subthemes were cancer concealment, resistance to cancer identity, and feelings of no longer being a normal person); and (c) social consequences of stigma (subthemes were collapsed social network and limited help-seeking behaviors) (see Figure 2).
Sources of Stigma
In Chinese society, lung cancer is commonly regarded as a death sentence and a contagion, rather than a self-inflicted illness (i.e., caused by smoking), because smoking is not seen as an unhealthy behavior. In addition, the negative feelings linked to a lung cancer diagnosis, such as guilt, self-blame, and feeling burdensome and discriminated against, are sources of stigma that patients with lung cancer feel about their disease.
Cancer stereotypes: “Death” and “contagion” were the most common terms participants used when mentioning lung cancer in the current study, reflecting stereotypes in China. Most participants stated that they felt their death was imminent when they were first diagnosed with lung cancer. Participant 8 said, “Lung cancer means a death sentence. I think my life is over.” Some participants believed that lung cancer was an infectious disease. Participant 6 said, “Since getting my diagnosis, I have never cooked for my grandchildren because of the infectivity of this illness. I also don’t share food with [other family and friends] now.”
Causal attribution: After their diagnosis, participants often wonder why they have this disease. In this study, most individuals attributed their disease to uncontrollable factors (e.g., air pollution, bad luck) or personality traits. Participant 9 said, “This is my fate, [it] is karma, and I deserve this.” Participant 15 said, “I think it is because I have some unspeakable things suppressed in my heart.” Of note, patients who had a smoking history may have attributed their illness to smoking; however, they still tended to rationalize their smoking behavior as a way of minimizing their stress. Participant 7 said, “My daily life habits are unhealthy. I used to smoke about a pack and a half per day. However, smoking is the only way for me to relax from heavy workloads and stress. It’s not my fault.” Some participants disputed the link between smoking behavior and lung cancer. Participant 9 said, “Is it because of smoking? My colleagues are also smokers, but they don’t [have] it.”
Burdensome feelings: Since their lung cancer diagnosis, patients’ and their family members’ daily lives and work were disrupted or suspended. Their previously busy lives suddenly stopped, and life transitioned to focus on cancer treatment, which led to heavy financial and caregiving burdens on their family members. Participant 13 said, “Now I am in the hospital and unable to work, which increased the burdens and pressure for my family. I often ask myself why I got this illness, and I feel guilty and [blame myself].” In addition, some participants mentioned that they felt burdensome because people in their lives had to move where they usually smoke to a different area because of their diagnosis. These life changes made patients feel useless, guilty, and shameful. Participant 1 said, “When other people want to smoke, they try to avoid me. I feel that I bring trouble and inconvenience to them.”
Social discrimination: People around the patients with lung cancer, such as their family members, relatives, friends, and colleagues, may have implicit discrimination, which can manifest as verbal slander, treating the patient differently, and avoidance. Participant 6 said, “All [the] people around me said the cancer was a death sentence, and people getting cancer would become skinny and pale and not like a normal person. No one says a good word.” Participant 8 said, “Now my colleagues avoid me and look at me differently. For example, if I open the food packaging bag and give the food to others, they will not take it.” Participant 13 said, “When I dined out with my friends, a friend put all the [desired food from the shared] dishes in her bowl first, and then she never touched the dishes again once I sat [at] the table.”
Stigma Manifestation
In China, when patients are facing a stigma, they might not address the stigma or directly express their feelings about it. However, they may internalize the stigma against their lung cancer, which may manifest as cancer concealment, resistance to cancer identity, and feelings of no longer being a normal person.
Cancer concealment: Keeping one’s standing in society is a prevalent concept in Chinese culture. This concept is roughly translated to saving or maintaining face and is incredibly important. When one’s standing in society changes for the worse, it is considered losing face (diūliăn in Chinese) and can negatively affect one’s mental health and social relationships. Participants stated that the lung cancer diagnosis was a bad thing that made them lose face; therefore, they tended to conceal their diagnosis from others, which, in turn, made them uneasy and anxious. Participant 7 said,
I used to be an excellent student in my class. I [did not] want my previous classmates to know bad things [like my lung cancer diagnosis] about me that might make me lose face. When I go to the hospital, I keep up my appearance and hide my medical report in a black bag, in case my neighbors or friends find out my secret.
Participant 1 said,
When my friends asked me why I didn’t show up for such a long time, the only thing I could tell them was that I was too busy. I felt extremely stressed when I talked with them because I was worried they might find out something.
Resistance to cancer identity: Patients’ identities were threatened by their lung cancer diagnosis, which altered their self-perception from a normal person to a stigmatized one. Participant 14 said, “I don’t want to be reminded that I am a person with cancer.” Participants also expressed their resistance to their new identities as a person with lung cancer. Participant 17 said, “I would feel depressed and [despaired] suddenly when people around me mentioned cancer, which is extremely hard to accept.”
Feelings of no longer being a normal person: Many participants mentioned that they felt they were no longer a normal person after their lung cancer diagnosis, which made them have a low self-value. Participant 19 said, “Everyone who has this disease would feel different from others. This disease has become a trait mark on me as a special one.” In addition, they became more sensitive to others’ caring behaviors, which made them feel they were being treated differently. Participant 7 said, “I wish my friend never gave money to me [for my cancer care]. Because this behavior made me feel I was pathetic and not a normal person anymore.”
Social Consequences of Stigma
In the Chinese sociocultural context, social consequences of stigma were categorized into two domains: collapsed social network and limited help-seeking behaviors.
Collapsed social network: Most participants mentioned that they found it difficult to return to their former social life, and instead tended to stay away from their former social networks because they anticipated awkward and burdensome feelings in social interactions, particularly in the context of the Chinese tobacco and alcohol culture. Participant 15 said,
I only stayed at home and seldom dined out with friends for a dinner. I can’t drink alcohol when they toast to me, and it would be awkward if I refused to drink or asked others [not to] smoke in the room.
In addition, Chinese patients with lung cancer were unwilling to establish new social connections with other patients via a cancer support group. Participant 14 said, “I don’t want to join in peer support activity. After all, they are unhealthy people. Their bad mood will affect me negatively.”
Limited help-seeking behaviors: Because of the effects of the stigma toward lung cancer, participants had a low inclination to seek help for social support and to receive anticancer treatment. In this study, participants stated they were unwilling to seek support from others, including psychological support and financial aid, even if they needed the help. Participant 9 said, “I am so [depressed]. I want to find someone to [whom I can] pour out all of my sufferings. But I don’t want my friends to know my disease.” Participant 18 said, “Even though my company would subsidize people who suffered from serious illness, I still chose to [forgo] this financial aid. I don’t want my colleagues knowing my diagnosis.”
Participants also mentioned that lung cancer was seen as a fatal disease. They believed the treatment was futile (therapeutic nihilism), which negatively influenced their medical help-seeking behaviors. Participant 6 said, “For this disease, the cure is impossible. The medical treatment for us is futile. I don’t want to waste all my money on this meaningless thing.” Participant 1 said, “I told my wife I would not receive [radiation therapy] and chemotherapy because this treatment is for people who are dying and incurable. I wouldn’t get treatments [even] if I was so ill.”
Discussion
This study revealed that stigma toward lung cancer and its social consequences among Chinese patients with this disease is rooted in factors other than smoking denormalization. These three themes were generated to give the authors a comprehensive view of lung cancer stigma in the context of Chinese culture.
Sources of Stigma
In this study, patients perceived their lung cancer diagnosis as a death sentence or a contagion, which is inconsistent with a prior study conducted in the United States (Webb & McDonnell, 2018). Death and contagion are two common cancer myths (Daher, 2012). With advances in lung cancer treatment since the early 2000s, (e.g., progress in targeted therapy and immunotherapy), mortality rates from lung cancer have decreased sharply (Howlader et al., 2020). Despite that, the results of this study indicated that stereotypes about lung cancer have not changed in China. In Illness as Metaphor by Sontag (1978), the concerns about cancer were caused by the lack of knowledge of its causes and possible cures. Therefore, this finding indicated that educational campaigns about lung cancer may be necessary to optimize patients’ illness perception.
Prior studies in other countries highlighted that a stigma toward lung cancer is often closely linked with smoking denormalization (Chapple et al., 2004; Hamann et al., 2018), although the culture in China finds smoking acceptable. This discrepancy may be explained by the varied underlying meanings of smoking behaviors across different countries. In most Western countries, smoking has been treated as an unethical behavior through the widespread implementation of antismoking approaches, including smoking policies and antitobacco campaigns (Rozin & Singh, 1999; Stuber et al., 2008). However, cigarette smoking in China is still well accepted, and even has a strong social function. For example, it is customary to gift cigarettes and light another person’s cigarettes to show respect for and to reinforce connections with others during social occasions (Rich & Xiao, 2012). In addition, it is regarded as impolite or not giving face (disrespecting) to others when people refuse cigarette offerings (Hu et al., 2012). Considering that, patients reported feeling burdensome and uneasy during social interactions because they lost face and could no longer smoke or drink after their lung cancer diagnosis.
Consistent with the Liu et al. (2016) study, feeling burdensome or discriminated against were also sources of stigma, which reflected the patients’ perceptions about their own disease. In Chinese culture, family is regarded as the most important part of one’s life. Confucianism is a philosophy and belief system from ancient China that has great influence on Chinese culture. With the impact of this culture, Chinese people bear a large obligation to and responsibility for their families (Badanta et al., 2022). However, after receiving a lung cancer diagnosis, patients often lost their ability to work and care for the family. Instead, they had to rely on their families for support (e.g., daily care, emotional and financial support), which was also reported in a previous study (Lee & Bell, 2011). Therefore, patients living with lung cancer were often concerned about the burden the diagnosis placed on their family, which caused the patients to blame themselves for their diagnosis. In addition, cancer is a taboo topic in Chinese culture because it is often associated with death (Dong et al., 2016). Because of this, most people misunderstand cancer and do not know the appropriate way to behave around patients with cancer (e.g., what to say, how to interact, when to help), which is a source of discomfort and tension (Occhipinti et al., 2018). Patients’ families often avoid talking about cancer topics with the patients. This approach suppressed patients’ expressions about their thoughts and feelings toward the diagnosis, which can be harmful when trying to maintain their intimate relationships and patients’ emotional well-being (Senden et al., 2015). These findings imply that public education and communication strategies are needed in Chinese society to address the stigma toward lung cancer.
Stigma Manifestation
In China, lung cancer is stigmatized as a bad thing and is often associated with death and contagion. These beliefs lead to patients losing face. In China, upholding face (miànzi in Chinese) is incredibly important because it affects one’s ability to mobilize social capital to attain essential social status (Yang & Kleinman, 2008). There is an old saying in China that “an individual needs face like a tree needs bark.” Therefore, face culture played a central role in determining stigma in China. This finding was consistent with results from people with schizophrenia and AIDS within Chinese culture (Yang & Kleinman, 2008). To preserve their face, patients often conceal their disease and avoid social occasions where they may openly talk about their disease, as reported in prior studies (Chapple et al., 2004; Yang & Kleinman, 2008).
Most patients resisted their cancer identity, which had a negative influence on them. Lung cancer diagnosis significantly threatened the patient’s identity, which reflected their perception of how others saw them (Knapp et al., 2014). Most patients refused to accept their cancer identity because lung cancer was perceived as an ominous thing that would cause them to lose face. Based on social identity theory, when an individual does not view their group favorably, they can attempt to leave that group (Islam, 2014). In other words, people who solely focus on the bad aspects of their cancer identity are at risk of alienating themselves from peer support. In contrast, emphasizing the positive effects of one’s cancer identity, such as viewing an individual with cancer as a strong and positive person (Harwood & Sparks, 2003), could help patients better accept their new roles and partake in peer-support activities.
In addition, people easily internalize social discrimination into a part of their self-evaluation. Participants in this study no longer viewed themselves as a normal person and had a lower social standing in comparison to the healthy population. This is also called self-stigma (Corrigan & Watson, 2002). People have negative attitudes about their condition, which can lead to patients’ social constraints (Wu et al., 2020), depression, and low quality of life (Maguire et al., 2019). This finding highlighted that healthcare professionals, such as oncology nurses, could provide timely psychoeducational interventions for patients who had difficulties talking about their diagnosis, accepting their cancer identity, and no longer viewing themselves as a normal person.
Social Consequences of Stigma
The current study found that stigma hindered patients with lung cancer from returning to their social life, which was demonstrated in other studies (Stergiou-Kita et al., 2016; van Roij et al., 2019). In Chinese culture, maintaining and saving face is essential for someone to maintain their dignity and normal social life. However, a lung cancer diagnosis was treated as a faceless hindrance. Maintaining face promotes trust and respect, which are important aspects to building connections (guānxì in Chinese) (Yang & Kleinman, 2008). In Chinese society, relationships play an important role in deciding the attainment and allocation of resources (Ai, 2006). Therefore, a loss of face is dreadful for Chinese people, and even leads to distance in social relationships. Consistent with findings from Corrigan et al. (2005), the stigmatized population tended to constrict their social activities. Gradually, patients’ previous social networks were disrupted. In addition, patients also had difficulties accepting their cancer identity and participating in peer support activities, which impeded them from building new social networks. Maintaining a social life is a challenging issue for Chinese patients with lung cancer.
In addition, help-seeking behavior was limited among Chinese patients with lung cancer. Although the benefits of social support in lung cancer care have been reported (Luszczynska et al., 2013), patients expressed they would rather give up the opportunity to obtain support because they felt too stigmatized and ashamed to disclose their disease. One study suggested that social identification could facilitate patients’ willingness to access external support (Klik et al., 2019). However, in this study, patients suffered from accepting their cancer identity, which might hinder their help-seeking behaviors. Although there were existing social supports, stigma impeded patients’ willingness to access new support resources. This finding was supported by Williamson et al. (2018), who found that the fear of disclosure prevented patients from seeking support and increased their emotional distress. In addition, with the effects of cancer fatalism and therapeutic nihilism, individuals often focused on death instead of oncology treatment, which may influence patients’ medical help-seeking behaviors and even clinical outcomes (Carter-Harris et al., 2014; Chambers et al., 2012). Additional support for patients with lung cancer is needed to adopt a patient identity and dispel concerns about seeking help.
Limitations
There were several limitations in this study. Selection bias may exist because the recruited participants all agreed to be interviewed about their feelings and experiences, and were less likely to feel stigma than patients who refused to participate. In addition, family caregivers were not included in this study. In China, family members are very important participants and supporters during a patient’s lung cancer trajectory, and they may provide more comprehensive insights. Future studies may consider exploring stigma toward lung cancer from family members’ perspectives.
Implications for Nursing Practice and Research
The sources of lung cancer stigma are socioculturally specific. Existing stereotypes and prejudice in Chinese society should be the focus of antistigma intervention at the population level. At the individual level, cancer concealment, resistance to cancer identity, and no longer feeling like a normal person were three common manifestations that may be indicators for stigma among patients with lung cancer. In addition, stigma also had a profound effect on patients’ social life and help-seeking behaviors, highlighting the demands of effective strategies to combat lung cancer stigma and its social consequences. To date, there are a limited number of nursing studies that have explored lung cancer stigma, particularly in the Chinese culture. Future studies involving families and healthcare professionals may help provide comprehensive insight into the patients’ lived experiences of lung cancer stigma. Novel approaches, such as individualized counseling programs and anticancer stigma campaigns for people with lung cancer, should be developed and tested in future studies.

Conclusion
This study revealed the formation of stigma and its social consequences among patients with lung cancer in China. The formation of stigma was closely related to the sociocultural meaning of lung cancer, rather than smoking denormalization. Multilevel strategies, including interventions at the population and individual levels, could help to combat lung cancer stigma in China. In addition, psychosocial supports for this vulnerable population are necessary to better adapt to their new social life.
About the Authors
Xiaohang Liu, RN, is a PhD student in the School of Nursing at the University of Hong Kong; Jiudi Zhong, BSN, RN, is the head nurse in the Department of Thoracic Surgery at Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center of Cancer Medicine in Guangzhou; and Jinying Ren, MSN, RN, is a student in the master’s nursing program, and Jun-E Zhang, PhD, RN, is a professor and the associate dean, both in the School of Nursing at Sun Yat-sen University in Guangzhou. This research was funded by the National Social Science Fund of China (Grant/Award No. 16BSH053; principal investigator: Zhang) Liu and Zhang contributed to the conceptualization and design. Liu, Zhong, and Ren completed the data collection. Zhang provided statistical support. Liu, Ren, and Zhang provided the analysis. Liu, Zhong, and Zhang contributed to the manuscript preparation. Zhang can be reached at zhangje@mail.sysu.edu.cn, with copy to ONFEditor@ons.org. (Submitted January 2023. Accepted May 3, 2023.)
References
Ai, J. (2006). Guanxi networks in China: Its importance and future trends. China and World Economy, 14(5), 105–118. https://doi.org/10.1111/j.1749-124X.2006.00034.x
Badanta, B., González-Cano-Caballero, M., Suárez-Reina, P., Lucchetti, G., & de Diego-Cordero, R. (2022). How does Confucianism influence health behaviors, health outcomes and medical decisions? A scoping review. Journal of Religion and Health, 61(4), 2679–2725. https://doi.org/10.1007/s10943-022-01506-8
Braun, V., & Clarke, V. (2008). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Carter-Harris, L., Hermann, C.P., Schreiber, J., Weaver, M.T., & Rawl, S.M. (2014). Lung cancer stigma predicts timing of medical help-seeking behavior. Oncology Nursing Forum, 41(3), E203–E210. https://doi.org/10.1188/14.ONF.E203-E210
Chambers, S.K., Dunn, J., Occhipinti, S., Hughes, S., Baade, P., Sinclair, S., . . . O’Connell, D.L. (2012). A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer, 12, 184. https://doi.org/10.1186/1471-2407-12-184
Chapple, A., Ziebland, S., & McPherson, A. (2004). Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ, 328(7454), 1470.
Corrigan, P.W., Kerr, A., & Knudsen, L. (2005). The stigma of mental illness: Explanatory models and methods for change. Applied and Preventive Psychology, 11(3), 179–190.
Corrigan, P.W., & Watson, A.C. (2002). The paradox of self-stigma and mental illness. Clinical Psychology, 9(1), 35–53.
Daher, M. (2012). Cultural beliefs and values in cancer patients. Annals of Oncology, 23(Suppl. 3), 66–69.
Dong, F., Zheng, R., Chen, X., Wang, Y., Zhou, H., & Sun, R. (2016). Caring for dying cancer patients in the Chinese cultural context: A qualitative study from the perspectives of physicians and nurses. European Journal of Oncology Nursing, 21, 189–196.
Ferlay, J., Ervik, M., Lam, F., Colombet, M., Mery, L., Piñeros, M., . . . Bray, F. (2020). Global cancer observatory: Cancer today. International Agency for Research on Cancer. World Health Organization. https://gco.iarc.fr/today
Ferrucci, L.M., Cartmel, B., Turkman, Y.E., Murphy, M.E., Smith, T., Stein, K.D., & McCorkle, R. (2011). Causal attribution among cancer survivors of the 10 most common cancers. Journal of Psychosocial Oncology, 29(2), 121–140.
Goffman, E. (1986). Stigma: Notes on the management of spoiled identity. Simon and Schuster.
Hamann, H.A., Ver Hoeve, E.S., Carter-Harris, L., Studts, J.L., & Ostroff, J.S. (2018). Multilevel opportunities to address lung cancer stigma across the cancer control continuum. Journal of Thoracic Oncology, 13(8), 1062–1075.
Harwood, J., & Sparks, L. (2003). Social identity and health: An intergroup communication approach to cancer. Health Communication, 15(2), 145–159.
Howlader, N., Forjaz, G., Mooradian, M.J., Meza, R., Kong, C.Y., Cronin, K.A., . . . Feuer, E.J. (2020). The effect of advances in lung-cancer treatment on population mortality. New England Journal of Medicine, 383(7), 640–649.
Hu, M., Rich, Z.C., Luo, D., & Xiao, S. (2012). Cigarette sharing and gifting in rural China: A focus group study. Nicotine and Tobacco Research, 14(3), 361–367. https://doi.org/10.1093/ntr/ntr262
Islam, G. (2014). Social identity theory. In T. Teo (Ed.), Encyclopedia of critical psychology (pp. 1781–1783). Springer. http://doi.org/10.1007/978-1-4614-5583-7_289
Klik, K.A., Williams, S.L., & Reynolds, K.J. (2019). Toward understanding mental illness stigma and help-seeking: A social identity perspective. Social Science and Medicine, 222, 35–43.
Knapp, S., Marziliano, A., & Moyer, A. (2014). Identity threat and stigma in cancer patients. Health Psychology Open, 1(1), 2055102914552281. https://doi.org/10.1177/2055102914552281
Lee, J., & Bell, K. (2011). The impact of cancer on family relationships among Chinese patients. Journal of Transcultural Nursing, 22(3), 225–234.
Liu, H., Yang, Q., Narsavage, G.L., Yang, C., Chen, Y., Xu, G., & Wu, X. (2016). Coping with stigma: The experiences of Chinese patients living with lung cancer. SpringerPlus, 5(1), 1790.
Liu, X.H., Marlow, L.A., Zhong, J., & Zhang, J.E. (2018). Public stigma towards patients with lung cancer and its influencing factors. Journal of Nursing Science, 33(7), 80–84.
Liu, X.H., Zhong, J.D., Zhang, J.E., Cheng, Y., & Bu, X.Q. (2020). Stigma and its correlates in people living with lung cancer: A cross-sectional study from China. Psycho-Oncology, 29(2), 287–293.
Luszczynska, A., Pawlowska, I., Cieslak, R., Knoll, N., & Scholz, U. (2013). Social support and quality of life among lung cancer patients: A systematic review. Psycho-Oncology, 22(10), 2160–2168. https://doi.org/10.1002/pon.3218
Maguire, R., Lewis, L., Kotronoulas, G., McPhelim, J., Milroy, R., & Cataldo, J. (2019). Lung cancer stigma: A concept with consequences for patients. Cancer Reports, 2(5), e1201.
Marlow, L.A.V., Waller, J., & Wardle, J. (2015). Does lung cancer attract greater stigma than other cancer types? Lung Cancer, 88(1), 104–107. https://doi.org/10.1016/j.lungcan.2015.01.024
Morrison, E.J., Novotny, P.J., Sloan, J.A., Yang, P., Patten, C.A., Ruddy, K.J., & Clark, M.M. (2017). Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clinical Lung Cancer, 18(5), 497–503.
Mosher, C.E., & Danoff-Berg, S. (2007). Death anxiety and cancer-related stigma: A terror management analysis. Death Studies, 31(10), 885–907.
Munhall, P.L. (2012). A phenomenological method. In P.L. Munhall (Ed.), Nursing research: A qualitative perspective (5th ed., pp. 113–176). Jones and Bartlett Learning.
Occhipinti, S., Dunn, J., O’Connell, D.L., Garvey, G., Valery, P.C., Ball, D., . . . Chambers, S. (2018). Lung cancer stigma across the social network: Patient and caregiver perspectives. Journal of Thoracic Oncology, 13(10), 1443–1453.
Ostroff, J.S., Riley, K.E., Shen, M.J., Atkinson, T.M., Williamson, T.J., & Hamann, H.A. (2019). Lung cancer stigma and depression: Validation of the lung cancer stigma inventory. Psycho-Oncology, 28(5), 1011–1017. https://doi.org/10.1002/pon.5033
Pan, Z. (2004). Socioeconomic predictors of smoking and smoking frequency in urban China: Evidence of smoking as a social function. Health Promotion International, 19(3), 309–315.
Peretti-Watel, P., Legleye, S., Guignard, R., & Beck, F. (2014). Cigarette smoking as a stigma: Evidence from France. International Journal on Drug Policy, 25(2), 282–290.
Rich, Z.C., & Xiao, S. (2012). Tobacco as a social currency: Cigarette gifting and sharing in China. Nicotine and Tobacco Research, 14(3), 258–263. https://doi.org/10.1093/ntr/ntr156
Rosman, S. (2004). Cancer and stigma: Experience of patients with chemotherapy-induced alopecia. Patient Education and Counseling, 52(3), 333–339. https://doi.org/10.1016/s0738-3991(03)00040-5
Rozin, P., & Singh, L. (1999). The moralization of cigarette smoking in the United States. Journal of Consumer Psychology, 8(3), 321–337.
Senden, C., Vandecasteele, T., Vandenberghe, E., Versluys, K., Piers, R., Grypdonck, M., & Van Den Noortgate, N. (2015). The interaction between lived experiences of older patients and their family caregivers confronted with a cancer diagnosis and treatment: A qualitative study. International Journal of Nursing Studies, 52(1), 197–206.
Siegel, R.L., Miller, K.D., Fuchs, H.E., & Jemal, A. (2022). Cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(1), 7–33.
Sontag, S. (1978). Illness as metaphor. Farrar, Straus and Giroux.
Stergiou-Kita, M., Pritlove, C., & Kirsh, B. (2016). The “Big C”—Stigma, cancer, and workplace discrimination. Journal of Cancer Survivorship, 10(6), 1035–1050.
Stuber, J., Galea, S., & Link, B.G. (2008). Smoking and the emergence of a stigmatized social status. Social Science and Medicine, 67(3), 420–430. https://doi.org/10.1016/j.socscimed.2008.03.010
Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357.
van Roij, J., Brom, L., Youssef-El Soud, M., van de Poll-Franse, L., & Raijmakers, N.J.H. (2019). Social consequences of advanced cancer in patients and their informal caregivers: A qualitative study. Supportive Care in Cancer, 27(4), 1187–1195. https://doi.org/10.1007/s00520-018-4437-1
Webb, L.A., & McDonnell, K.K. (2018). Not a death sentence: Perspectives of African American women living with lung cancer. Oncology Nursing Forum, 45(1), 46–54. https://doi.org/10.1188/18.ONF.46-54
Webb, L.A., McDonnell, K.K., Adams, S.A., Davis, R.E., & Felder, T.M. (2019). Exploring stigma among lung cancer survivors: A scoping literature review. Oncology Nursing Forum, 46(4), 402–418. https://doi.org/10.1188/19.ONF.402-418
Weiss, J., Yang, H., Weiss, S., Rigney, M., Copeland, A., King, J.C., & Deal, A.M. (2017). Stigma, self-blame, and satisfaction with care among patients with lung cancer. Journal of Psychosocial Oncology, 35(2), 166–179. https://doi.org/10.1080/07347332.2016.1228095
Williamson, T.J., Choi, A.K., Kim, J.C., Garon, E.B., Shapiro, J.R., Irwin, M.R., . . . Stanton, A.L. (2018). A longitudinal investigation of internalized stigma, constrained disclosure, and quality of life across 12 weeks in lung cancer patients on active oncologic treatment. Journal of Thoracic Oncology, 13(9), 1284–1293.
Williamson, T.J., Kwon, D.M., Riley, K.E., Shen, M.J., Hamann, H.A., & Ostroff, J.S. (2020). Lung cancer stigma: Does smoking history matter? Annals of Behavioral Medicine, 54(7), 535–540.
Wu, I.H.C., Tsai, W., McNeill, L.H., & Lu, Q. (2020). The associations of self-stigma, social constraints, and sleep among Chinese American breast cancer survivors. Supportive Care in Cancer, 28(8), 3935–3944.
Yang, D., Liu, Y., Bai, C., Wang, X., & Powell, C.A. (2020). Epidemiology of lung cancer and lung cancer screening programs in China and the United States. Cancer Letters, 468, 82–87.
Yang, L.H., & Kleinman, A. (2008). ‘Face’ and the embodiment of stigma in China: The cases of schizophrenia and AIDS. Social Science and Medicine, 67(3), 398–408.
Zhang, G., Zhan, J., & Fu, H. (2022). Trends in smoking prevalence and intensity between 2010 and 2018: Implications for tobacco control in China. International Journal of Environmental Research and Public Health, 19(2), 670.

