Symptom Experiences Among Individuals With Prostate Cancer and Their Partners: Influence of Sociodemographic and Cancer Characteristics
Objectives: To determine if subgroups of individuals with prostate cancer and their partners could be identified based on their distinct symptom profiles and to identify and characterize subgroups based on sociodemographic and cancer characteristics.
Sample & Setting: 263 individuals with prostate cancer and 263 partners recruited from three academic cancer centers in the Midwest.
Methods & Variables: Latent class analysis was applied to divide individuals into subgroups based on symptom prevalence. Multinomial logistic regression models were used to estimate the prevalence of each symptom, predict subgroup membership, and adjust for direct or indirect effects of covariates on the symptoms.
Results: Three distinct subgroups (low, moderate, and high symptoms) were identified among individuals with prostate cancer and partners, respectively. Education and household income of individuals with prostate cancer were associated with different symptom burdens. Partners’ household income differentiated among the subgroups.
Implications for Nursing: Understanding the influence of sociodemographic and cancer characteristics can inform risk stratification and tailored symptom management interventions.
Jump to a section
Individuals with cancer experience various physical and psychological symptoms, including pain, fatigue, sleep disturbance, depression, and symptoms specific to their cancers and treatments (e.g., urinary and erectile dysfunction) (Miaskowski et al., 2006; Sullivan et al., 2018). Symptoms can occur as a result of the disease, the treatment for it, or interactions among the disease, treatment, and patients’ comorbidities (Maliski et al., 2008; Miaskowski et al., 2015). Unrelieved symptoms can have negative effects on the quality of life (QOL) of individuals with cancer (Dodd et al., 2010; Miaskowski et al., 2006, 2007).
Partners of individuals with cancer play an integral role in helping them manage the effects of treatment while also supporting their physical and emotional needs. The symptoms and related experiences of individuals with cancer affect their partners’ health, causing partners to experience symptoms such as anxiety, sleep disturbance, fatigue, and pain (Carney et al., 2011; El-Jawahri et al., 2017; Fletcher et al., 2008, 2009; Jadalla et al., 2020). These symptoms of partners—coupled with their existing health problems, comorbidities, competing demands, and life stresses—may lead to deterioration in the partners’ QOL (Ellis et al., 2021; Lapid et al., 2016).
Symptom cluster research has provided a scientific basis to understand co-occurring symptoms and the symptom profiles of individuals with cancer. Within this broad area of research, two major approaches have been adopted—that is, a symptom-centered approach to identify symptom clusters of co-occurring symptoms and a person-centered approach, which the authors used in this study, to characterize subgroups of individuals based on their experiences with specific symptoms (Miaskowski et al., 2007, 2017). The person-centered approach enables the identification of individual subgroups with distinct symptom profiles (Miaskowski et al., 2007, 2017). Analytical methods including latent class analysis (LCA), hierarchical cluster analysis, and machine learning techniques such as K-modes have been applied to group individuals with similar symptom profiles (Kim et al., 2012; Miaskowski et al., 2014, 2015; Papachristou et al., 2018; Reese et al., 2015). Using this approach, previous studies on individuals with cancer have identified different subgroups among them, with low/all low and high/all high symptoms as two of the most common subgroups (Astrup et al., 2017; Doong et al., 2015; Ferreira et al., 2008; Gwede et al., 2008; Kim et al., 2012; Lin et al., 2021; Miaskowski et al., 2014; Papachristou et al., 2018; Reese et al., 2015; Snyder et al., 2009). Depending on whether symptom occurrence or symptom severity was analyzed, the low/high labeling of the subgroups represents the probability of symptom occurrence or severity of symptoms (Astrup et al., 2017; Doong et al., 2015; Miaskowski et al., 2014). Different granularities and naming schemes have been used when examining and describing symptom characteristics for individuals within each subgroup. For instance, in addition to the all low and all high subgroups, some studies also found an all moderate subgroup in which individuals’ symptoms were neither all high nor all low (Lin et al., 2021; Miaskowski et al., 2014; Reese et al., 2015). Other researchers have clustered individuals with cancer based on prevalence and combinations of physical and psychological symptoms, including high psychological and low psychological (Astrup et al., 2017); moderate physical and lower psychological, and moderate physical and higher psychological (Miaskowski et al., 2015; Papachristou et al., 2018); low pain and high fatigue (Doong et al., 2015; Kim et al., 2012); and high depressed mood and cognitive disturbance, and high fatigue and insomnia (Kim et al., 2012).
However, little research has viewed the latent variable behind the subgroups as a part of this holistic model that consisted of sociodemographic and cancer characteristics and examined the direct and indirect roles of these characteristics on the symptoms (Miaskowski et al., 2015). The clustering process has often been based solely on the symptoms without considering the effects of individual characteristics on the latent classes and the symptoms. However, symptom-related theories (e.g., Symptom Management Model, Theory of Unpleasant Symptoms) contend that individual and situational factors are critical factors that need to be better understood because they combine with the symptoms to create a multidimensional symptom experience for individuals with illness (Dodd et al., 2001; Larson et al., 1994; Lenz et al., 1997). In addition, although symptom cluster research has been increasingly adopted to study symptom experiences of individuals with cancer, their partners’ symptoms remain understudied. The lack of understanding of variations in partners’ symptom experience leads to inconsistency and uncertainty in appropriate management, despite partners’ critical role in cancer care and the patients’ symptom experiences. Therefore, it is crucial to consider the effects of these sociodemographic and cancer characteristics to gain a comprehensive view and understanding of symptom profiles of individuals with cancer and their partners.
In this study, the authors focused on individuals with prostate cancer and their partners because prostate cancer is the most prevalent type of cancer in men in the United States and globally (excluding skin cancer) (American Cancer Society, 2021b). This population has been understudied, particularly in symptom cluster research. Cancer-specific symptoms (e.g., hot flashes, urinary and erectile dysfunction) may co-occur with general symptoms among individuals with prostate cancer (American Cancer Society, 2021a; Galbraith et al., 2005; Maliski et al., 2008). In addition, prostate cancer is known as a “disease of couples,” which affects not only the individuals with the illness but also the partners. Therefore, this study aimed to examine the symptom experience of individuals with prostate cancer and their partners in the context of their sociodemographic characteristics and the patients’ cancer characteristics. Considering the study is focused on the patient–partner context in which symptom profiles of individuals with prostate cancer and their partners are studied, hereafter, to avoid ambiguity, the authors use “patient” to refer to individuals with prostate cancer and “partner” to refer to their partners when needed.
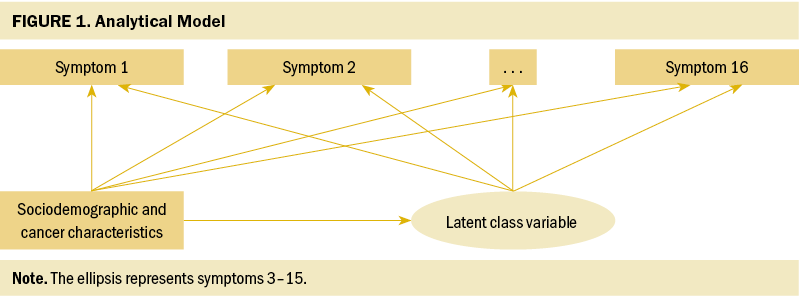
Figure 1 presents the overall conceptualization of the authors’ analytical model. Patients and partners were separately divided into different subgroups (i.e., latent classes) based on an unobservable construct—that is, the latent class variable. According to this model, the sociodemographic and cancer characteristics not only directly affect symptoms but also indirectly affect symptoms via the latent class variable. By controlling for the direct and indirect effects of the sociodemographic and cancer characteristics on the symptoms, the authors used a refined clustering model. Based on this analytical model, this study aimed to determine if subgroups of individuals with prostate cancer and their partners could be identified based on their distinct symptom profiles and to identify and characterize patient and partner subgroups based on select sociodemographic factors and cancer characteristics.
Methods
Study Population
This study is a secondary analysis of baseline data from a randomized clinical trial (NCT00708968) that examined the effects of a couple-based (patient–partner) intervention on the QOL of 263 individuals with prostate cancer and their partners (Northouse et al., 2007). Participants were recruited from three academic cancer centers in the Midwest. The study and its procedure have been published (Northouse et al., 2007, 2013). To be eligible for the clinical trial, patients needed to (a) have completed the primary treatment for localized prostate cancer or have a new diagnosis of recurrent or advanced cancer after completing primary treatment, (b) be at least 30 years old, (c) have a life expectancy of at least 12 months, and (d) have a spouse or partner. The partners had to be 21 years of age or older and identified as the patient’s primary caregiver. Data used in this analysis had been de-identified to adhere to the institutional review board requirements.
Measurements
Symptoms: General symptom distress was measured using the Symptom Scale of the Omega Screening Questionnaire (Mood & Bickes, 1989). Patients and partners separately responded to the questions and reported whether they were experiencing any of the 16 symptoms assessed (i.e., pain, fatigue, weight loss, sleeping problems, skin problems, body sensations, difficulty moving, stomach problems, bowel problems, urinary incontinence, breathing problems, heart problems, sexual problems, mental distress, mental fatigue, and concentration). Their symptoms were categorized as binary indicators (i.e., presence or absence).
Sociodemographic and cancer characteristics: The authors assessed patients’ sociodemographic characteristics (age, race, education, and income) and cancer characteristics (time since diagnosis and type of treatment). Type of treatment, along with phase of illness information, was recategorized into the following groups: (a) newly diagnosed patients who received a prostatectomy, (b) newly diagnosed patients who received radiation therapy, (c) recurrent patients who were under observation or had radiation therapy, and (d) advanced patients who had hormone-naive or hormone-refractory therapy. The authors excluded the stage of cancer variable from the study because of its high correlation (p = 0.97) with the type of treatment variable.
Data Analysis
Statistical analyses were conducted using SAS, version 9.4, and Mplus, version 8.4, with two-sided tests at a 0.05 significance level (Muthén & Muthén, 2018). Descriptive statistics were calculated to describe the demographic and cancer characteristics of patients and their partners.
LCA was applied to examine the latent subgroups based on the observed variables that have similar characteristics (Hagenaars & McCutcheon, 2002; Nylund-Gibson & Masyn, 2016). The participants were assigned to distinct subgroups based on their posterior probabilities (i.e., the probability of that observation being classified in a given class) for class membership. The authors applied LCA models with one to five subgroups to determine the number of subgroups of patients based on the prevalence of symptoms they experienced. The number of latent classes (i.e., subgroups) was determined based on the evaluation of model fit indices Akaike information criterion (AIC) and Bayesian information criterion (BIC) (Collins & Lanza, 2010); meanwhile, the optimal fitting model should make sense conceptually. To examine the influence of patients’ sociodemographic and cancer characteristics on their symptom prevalence–based clustering, the authors performed variable screening by conducting LCA modeling with each covariate (i.e., age, race, education, income, time since diagnosis, and type of treatment) while fixing the number of subgroups. The authors assumed that the covariates had not only indirect effects via the latent class variable on symptoms but also direct effects on symptoms, bypassing latent subgroups (Nylund-Gibson & Masyn, 2016). The multinomial logistic regression model was then fitted to estimate the prevalence of each symptom in the subgroups and predict subgroup membership while adjusting for the significant direct or indirect effects of covariates on the symptoms.
The authors repeated the same procedure for partners to identify the number of subgroups and examine the influence of partners’ sociodemographic characteristics and patients’ cancer characteristics on subgroups of partners based on partners’ symptoms experienced.
Results
Participant Characteristics and Symptom Prevalence
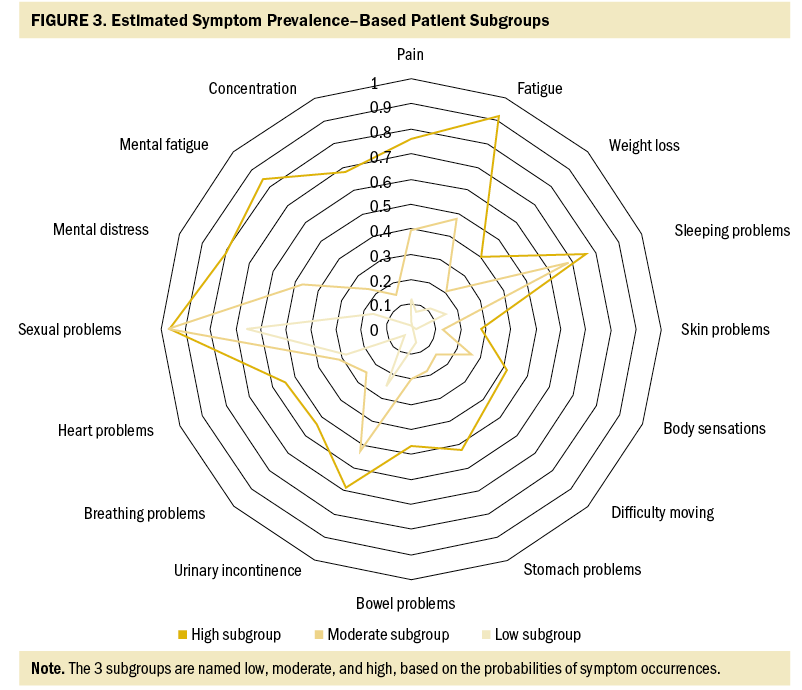
The sociodemographic and cancer characteristics of the 263 patient–partner dyads are presented in Table 1. Patients and partners were mainly White, with an average age of 63.09 and 59.03 years, respectively. On average, patients and partners had 15.7 years and 14.84 years of education, respectively. Most patients were newly diagnosed and received prostatectomy treatment. The average time since diagnosis was 30.01 months.
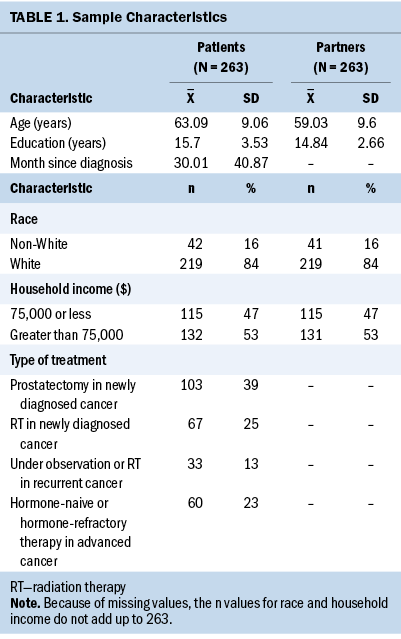
Figure 2 shows the prevalence of general symptoms among patients and their partners. The most common patient symptoms were sexual problems (89%), sleeping problems (54%), and urinary incontinence (49%). For partners, the most common general symptom was sleeping problems (59%), followed by mental distress (57%) and sexual problems (56%).
Symptom Prevalence–Based Patient and Partner Subgroups
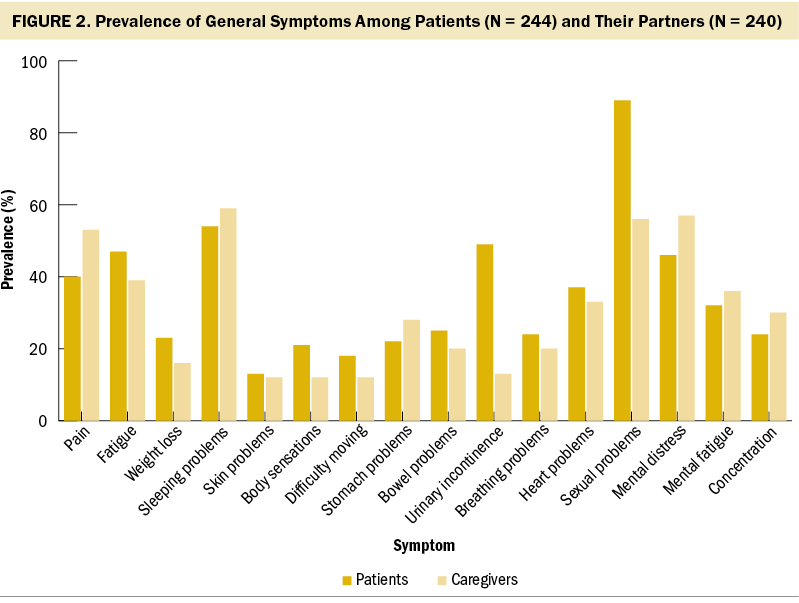
For patients, the latent class model with three subgroups (BIC: 1834.88, AIC: 1656.28) had the lowest BIC score and was selected as the optimal model. The probabilities of patients’ symptom occurrences are visualized in Figure 3. The three subgroups are named low, moderate, and high, based on the probabilities of symptom occurrences. In the low subgroup (n = 78, 32%), sexual problems were likely to occur, but the probabilities of other symptoms occurring were all low (all < 0.3). In the moderate subgroup (n = 100, 41%), all symptoms were more likely to occur to the patients than those in the low subgroup; patients were most likely to experience sexual problems, sleeping problems, and urinary incontinence. The high subgroup (n = 66, 27%) was characterized with high probabilities (greater than 0.7) of more symptoms and more types of symptoms, including sexual problems, fatigue, mental fatigue, mental distress, sleeping problems, and urinary incontinence. The probabilities of 12 of 16 symptoms were higher than 0.5 to occur to patients in the high subgroup.
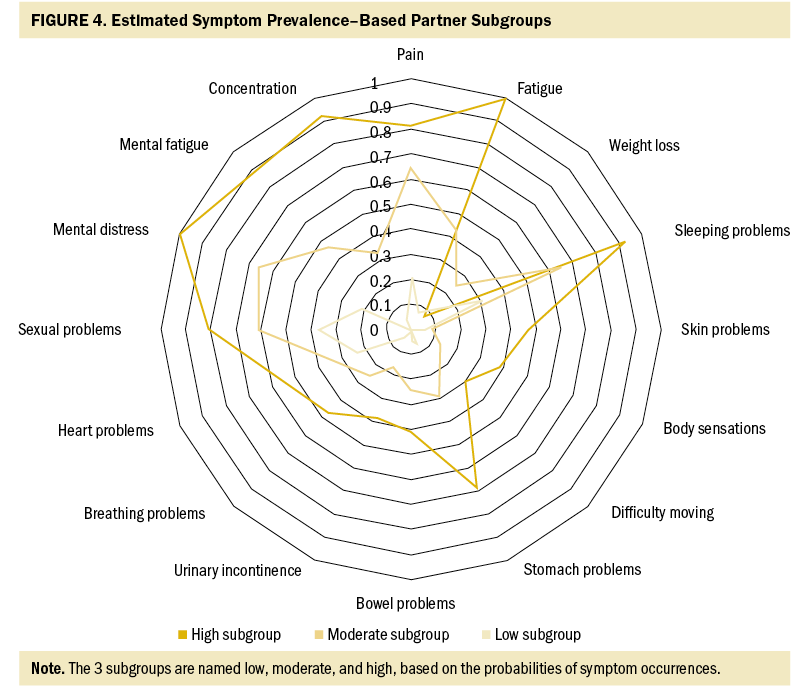
For partners, the three-subgroup model was selected (BIC: 1755.44, AIC: 1576.83). Figure 4 shows the estimated prevalence of partners’ symptoms in each subgroup. The first subgroup of partners (n = 84, 35%) had low probabilities of having any of the symptoms; excluding sleeping and sexual problems, the probabilities for other symptoms to occur were all less than 0.3 among these partners. For those in the moderate subgroup (n = 36, 15%), the probabilities of these partners experiencing mental distress, sleeping problems, sexual problems, and pain were moderate to high (greater than 0.5 and less than 0.7), and they had moderate to low probabilities (all less than 0.5) of experiencing the other symptoms. In the high subgroup (n = 120, 50%), partners had higher probabilities of experiencing all symptoms except for weight loss than those in the low and moderate subgroups. The probabilities of 7 of 16 symptoms were higher than 0.7 to occur to these partners, including pain, fatigue, sleeping problems, sexual problems, mental distress, mental fatigue, and concentration.
Influencing Factors
After adjusting for covariates, patients’ education and household income were associated with the latent class variable (p < 0.05). Patients with higher education levels were more likely to be in the low (odds ratio [OR] = 1.23, 95% confidence interval [CI] [1.05, 1.44]) and moderate (OR = 1.23, 95% CI [1.03, 1.45]) subgroups than the high subgroup. Patients with family incomes greater than $75,000 were less likely to be in the low (OR = 0.33, 95% CI [0.12, 0.93]) and moderate (OR = 0.2, 95% CI [0.07, 0.64]) subgroups than in the high subgroup compared to those with incomes of $75,000 or less.
For partners, family income was associated with the latent class variable (p < 0.05). Partners with household incomes greater than $75,000 were more likely to be in the low subgroup (OR = 3.68, 95% CI [1.28, 10.6]) than in the high subgroup compared to those with family incomes of $75,000 or less.
Discussion
To the authors’ knowledge, this is the first symptom cluster study that focuses on individuals with prostate cancer and their partners and uses a person-centered approach. The authors found that sexual problems were highly likely to occur in all three patient subgroups (probabilities ranging from 1 to 0.68) and in two of the partner subgroups (high and moderate, with probabilities of 0.8 and 0.61, respectively), regardless of their experiences of the other symptoms. Urinary incontinence was also likely to occur in the moderate and high subgroups among patients. Previous symptom cluster research that has included individuals with prostate cancer as part of their samples mainly used the symptom-centered approach to study symptom co-occurrence. Symptom clusters that have been identified in prior research included two to seven symptoms per cluster, with sexual, urinary, and bowel dysfunction being the most prevalent co-occurring symptoms (Capp et al., 2009; Lemanska et al., 2018; Maliski et al., 2008; Thavarajah et al., 2012). Among the few studies solely focused on individuals with prostate cancer, researchers have used a symptom-based approach to cluster the symptoms of patients receiving specific treatment for prostate cancer (e.g., radiation-induced rectal symptoms) (Capp et al., 2009) or a combination of psychosocial and physical symptoms in patients receiving different types of treatments (Lemanska et al., 2018; Maliski et al., 2008). Despite the heterogeneity in research methods, which made it challenging to compare findings across studies, the authors’ person-centered approach generated some similar results.
However, the authors’ person-centered approach, which focuses more on the interindividual variability of the symptom profiles instead of the co-occurrences of symptoms, has added a new perspective to symptom cluster research and filled the gaps in research on symptom clustering among caregivers, particularly among partners of individuals with prostate cancer. For instance, for patients in the moderate subgroup (41% of patients), the three most prevalent symptoms—sexual problems, sleeping problems, and urinary incontinence—had almost the same levels of probabilities of occurrence as in the high subgroup. However, the other symptoms were unlikely to occur among the patients in the moderate subgroup. Potentially, interventions can target one or multiple of these three symptoms (e.g., urinary incontinence) to ameliorate the overall symptom profiles of these patients, which may make it possible for them to transition into the low subgroup. Meanwhile, for patients in the high subgroup, the physical and psychological symptoms (e.g., sleeping problems, fatigue, mental distress, urinary incontinence, sexual problems) were interrelated and had deteriorating influences on each other; more comprehensive interventions are needed to ameliorate these symptoms. These results may also indicate the possibility that, if the symptoms are not addressed and managed appropriately, patients and partners may transition from low or moderate groups into high groups with more symptom burden.
The current study also contributes to a better understanding of the variability of partners’ symptom experiences. Compared to the patients, partners had a relatively higher prevalence of psychoneurologic symptoms (Tometich et al., 2019) including mental distress, mental fatigue, and concentration. This finding is consistent with the high psychological burden reported by partners in previous studies (Girgis et al., 2013; Kim et al., 2008). In addition, sexual problems and sleeping problems among partners were more prevalent than other symptoms in all three subgroups. This corresponds to the previously mentioned similar findings of sexual and sleeping problems among patients and sheds light on the interrelated and interwoven nature of patients’ and partners’ symptom experiences during prostate cancer survivorship. Couple-focused interventions may produce better outcomes if they are offered jointly to the patients and partners and provide partners of patients with more emotional support.
Another contribution of this study is that the authors examined the sociodemographic and cancer characteristics, symptoms, and latent variable of patient and partner subgroups in a holistic and refined model. Because the authors adjusted for the direct effects of these characteristics on symptoms and their indirect effects via the latent class variable, the current models identified and characterized the subgroups of patients and partners more accurately than studies that did not adjust for these effects. Of note, education had a significant effect on patients’ subgroup memberships. Patients with higher education levels were more likely to be in the low and moderate subgroups than the high subgroup, indicating that patients with more years of education may have more knowledge to problem solve and manage their symptoms. In addition, family income significantly affected patients’ and their partners’ subgroup memberships. Partners with family incomes greater than $75,000 were more likely to be in the low versus the high subgroup than those with lower incomes, indicating that partners may have more resources to help them manage the patients’ cancer and related challenges as their family incomes increased. Different from the partners, patients with incomes greater than $75,000 were more likely to belong to the high versus the moderate and low subgroups than those with lower incomes. This is different from the findings of previous studies on patients with other types of cancers, which indicated either no relationship or a positive relationship between higher household income and more positive symptom experiences of patients in different subgroups (Doong et al., 2015; Lin et al., 2021; Miaskowski et al., 2014). Because of the lack of existing studies using a person-centered approach to study symptom experiences of subgroups of individuals with prostate cancer, it is not possible to compare this result. Some explanations for the discrepancies in findings between the current study and prior research may be the fact that the authors adjusted for contextual covariates in the current modeling, used a different symptom scale, and focused only on individuals with prostate cancer, which may have a confounding gender effect. In addition, the authors’ post hoc analysis revealed that patients in the high subgroup had, on average, fewer years of education (14.81) than the sample mean (15.7). Even those with incomes greater than $75,000 had, on average, fewer years of education (15.19) than the sample mean. Given the positive correlation between patients’ education and income (analysis of variance p < 0.05) in the current sample, the low education levels of patients in this subgroup are seemingly contradictory to their income levels. This suggests that income and resources may buffer only a small part of the negative effects of low education on health. Instead, better education seems to provide more important psychosocial and health behaviors benefits, which can synergistically help fight structural vulnerability and lead to better health outcomes (Bourgois et al., 2017; Pampel et al., 2010). In-depth interviews may help to better understand how patients perceive and manage illnesses and symptoms in the context of their sociodemographic backgrounds.
Limitations
The current study has some limitations. First, the Symptom Scale of the Omega Screening Questionnaire was used to assess the occurrence of symptoms, and other person-centered symptom clustering research has mainly used symptom scales that included the Memorial Symptom Assessment Scale (Gwede et al., 2008; Lin et al., 2021; Papachristou et al., 2018), European Organisation for Research and Treatment of Cancer Quality-of-Life Questionnaire–Core 30 (Ferreira et al., 2008; Reese et al., 2015; Snyder et al., 2009), and Supportive Care Needs Survey–Short Form (Ferreira et al., 2008; Reese et al., 2015), or a combination of different scales (Doong et al., 2015). These assessment tools vary in terms of the number of symptoms included, the symptom dimensions assessed, the rating scales, and the recall period of symptom assessment (Kirkova et al., 2006). Coupled with the challenges caused by the lack of existing studies focused on prostate cancer, the heterogeneity in symptom measurements and analytical methods has made it challenging to compare findings across studies. Second, this study examined only symptom prevalence. Previous studies have used symptom occurrence (Miaskowski et al., 2014, 2015), symptom distress (Suwisith et al., 2008), and symptom severity (Dodd et al., 2010; Miaskowski et al., 2006) to cluster patients’ symptom subgroups. Although it is possible to yield richer results if symptom severity or distress data were included, previous research found that using occurrence and severity ratings resulted in very similar symptom clusters (Kim et al., 2009). Third, using secondary data posed limitations on the selection of measurements in the current analysis. If more social determinants of health data were available, a more comprehensive model could be built to create a fuller picture of influencing factors.
Implications for Nursing
Findings from the current study confirm the interindividual variability in the symptom experiences of individuals with prostate cancer and their partners. The current study particularly contributes to a better understanding of the variability of partners’ symptom experiences, suggesting that more emotional support should be provided to the partners regardless of their physical health. For individuals with prostate cancer, clinicians should consider offering couple- or family- focused symptom management interventions.
Identification of the characteristics that place individuals with prostate cancer and their partners at risk for a higher symptom burden can inform risk stratification and tailored symptom management interventions. In practice, it is important for clinicians to have in mind that patients and their partners are facing multidimensional symptom experiences embedded in their unique individual and situational backgrounds.
The current study also suggests that education plays a key role in providing psychosocial and health behaviors benefits. Clinicians should strive to promote patient and caregiver education and engagement through improvement in their health literacy.
Conclusion
In the context of sociodemographic and cancer characteristics, this study has confirmed inter-individual variability of the symptom experiences of individuals with prostate cancer and their partners. Understanding the influence of these characteristics can inform risk stratification and tailored symptom management interventions.
About the Authors
Shenmeng Xu, PhD, is a research scientist in the School of Nursing, Xianming Tan, PhD, is an associate professor in the Gillings School of Global Public Health in the Department of Biostatistics and a research associate professor in the Lineberger Comprehensive Cancer Center, and Peiran Guo, MS, and Chunxuan Ma, MS, are biostatisticians, both in the School of Nursing, all at the University of North Carolina at Chapel Hill; Katrina R. Ellis, PhD, MPH, MSW, is an assistant professor in the School of Social Work at the University of Michigan in Ann Arbor; Angela B. Smith, MD, MS, FACS, is an associate professor in the Department of Urology in the School of Medicine at the University of North Carolina at Chapel Hill; Laurel Northouse, PhD, RN, is a professor emerita in the School of Nursing at the University of Michigan; and Lixin Song, PhD, RN, FAAN, is a professor in the School of Nursing at the University of Texas Health Science Center at San Antonio. This research was supported, in part, by the National Institutes of Health/National Cancer Institute (R01 grant number: CA90739NCI, principal investigator: Northouse), the National Institutes of Health/National Institute of Nursing Research (R01 grant number: NR016990, principal investigator: Song), and the University of North Carolina Lineberger Comprehensive Cancer Center University Cancer Research Fund (principal investigator: Song). Xu, Smith, Northouse, and Song contributed to the conceptualization and design. Song completed the data collection. Tan, Guo, and Song provided statistical support. Xu, Guo, Ma, Smith, and Northouse provided the analysis. Xu, Guo, Ellis, Smith, Northouse, and Song contributed to the manuscript preparation. Xu can be reached at xushenmeng@gmail.com, with copy to ONFEditor@ons.org. (Submitted March 2022. Accepted September 23, 2022.)
References
American Cancer Society. (2021a). Cancer facts and figures, 2021. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-fact…
American Cancer Society. (2021b). Cancer facts for men. https://www.cancer.org/healthy/cancer-facts/cancer-facts-for-men.html
Astrup, G.L., Hofsø, K., Bjordal, K., Guren, M.G., Vistad, I., Cooper, B., . . . Rustøen, T. (2017). Patient factors and quality of life outcomes differ among four subgroups of oncology patients based on symptom occurrence. Acta Oncologica, 56(3), 462–470. https://doi.org/10.1080/0284186X.2016.1273546
Bourgois, P., Holmes, S.M., Sue, K., & Quesada, J. (2017). Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Academic Medicine, 92(3), 299–307. https://doi.org/10.1097/ACM.0000000000001294
Capp, A., Inostroza-Ponta, M., Bill, D., Moscato, P., Lai, C., Christie, D., . . . Denham, J.W. (2009). Is there more than one proctitis syndrome? A revisitation using data from the TROG 96.01 trial. Radiotherapy and Oncology, 90(3), 400–407. https://doi.org/10.1016/j.radonc.2008.09.019
Carney, S., Koetters, T., Cho, M., West, C., Paul, S.M., Dunn, L., . . . Miaskowski, C. (2011). Differences in sleep disturbance parameters between oncology outpatients and their family caregivers. Journal of Clinical Oncology, 29(8), 1001–1006.
Collins, L.M., & Lanza, S.T. (2010). Latent class and latent transition analysis: With applications in the social behavioral, and health sciences. Wiley.
Dodd, M.J., Cho, M.H., Cooper, B.A., & Miaskowski, C. (2010). The effect of symptom clusters on functional status and quality of life in women with breast cancer. European Journal of Oncology Nursing, 14(2), 101–110.
Dodd, M., Janson, S., Facione, N., Faucett, J., Froelicher, E.S., Humphreys, J., . . . Taylor, D. (2001). Advancing the science of symptom management. Journal of Advanced Nursing, 33(5), 668–676. https://doi.org/10.1046/j.1365-2648.2001.01697.x
Doong, S.-H., Dhruva, A., Dunn, L.B., West, C., Paul, S.M., Cooper, B.A., . . . Miaskowski, C. (2015). Associations between cytokine genes and a symptom cluster of pain, fatigue, sleep disturbance, and depression in patients prior to breast cancer surgery. Biological Research for Nursing, 17(3), 237–247. https://doi.org/10.1177/1099800414550394
El-Jawahri, A., Greer, J.A., Pirl, W.F., Park, E.R., Jackson, V.A., Back, A.L., . . . Temel, J.S. (2017). Effects of early integrated palliative care on caregivers of patients with lung and gastrointestinal cancer: A randomized clinical trial. Oncologist, 22(12), 1528–1534. https://doi.org/10.1634/theoncologist.2017-0227
Ellis, K.R., Oh, S., Hecht, H.K., & Northouse, L. (2021). Symptom distress and quality of life among Black Americans with cancer and their family caregivers. Psycho-Oncology, 30(8), 1356–1365. https://doi.org/10.1002/pon.5691
Ferreira, K.A.S.L., Kimura, M., Teixeira, M.J., Mendoza, T.R., da Nóbrega, J.C.M., Graziani, S.R., & Takagaki, T.Y. (2008). Impact of cancer-related symptom synergisms on health-related quality of life and performance status. Journal of Pain and Symptom Management, 35(6), 604–616. https://doi.org/10.1016/j.jpainsymman.2007.07.010
Fletcher, B.A.S., Schumacher, K.L., Dodd, M., Paul, S.M., Cooper, B.A., Lee, K., . . . Miaskowski, C. (2009). Trajectories of fatigue in family caregivers of patients undergoing radiation therapy for prostate cancer. Research in Nursing and Health, 32(2), 125–139. https://doi.org/10.1002/nur.20312
Fletcher, B.S., Paul, S.M., Dodd, M.J., Schumacher, K., West, C., Cooper, B., . . . Miaskowski, C.A. (2008). Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. Journal of Clinical Oncology, 26(4), 599–605. https://doi.org/10.1200/JCO.2007.12.2838
Galbraith, M.E., Arechiga, A., Ramirez, J., & Pedro, L.W. (2005). Prostate cancer survivors’ and partners’ self-reports of health-related quality of life, treatment symptoms, and marital satisfaction 2.5–5.5 years after treatment. Oncology Nursing Forum, 32(2), E30–E41. https://doi.org/10.1188/05.onf.e30-e41
Girgis, A., Lambert, S., Johnson, C., Waller, A., & Currow, D. (2013). Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. Journal of Oncology Practice, 9(4), 197–202. https://doi.org/10.1200/JOP.2012.000690
Gwede, C.K., Small, B.J., Munster, P.N., Andrykowski, M.A., & Jacobsen, P.B. (2008). Exploring the differential experience of breast cancer treatment-related symptoms: A cluster analytic approach. Supportive Care in Cancer, 16(8), 925–933. https://doi.org/10.1007/s00520-007-0364-2
Hagenaars, J.A., & McCutcheon, A.L. (2002). Applied latent class analysis. Cambridge University Press. https://doi.org/10.1017/CBO9780511499531
Jadalla, A., Ginex, P., Coleman, M., Vrabel, M., & Bevans, M. (2020). Family caregiver strain and burden: A systematic review of evidence-based interventions when caring for patients with cancer. Clinical Journal of Oncology Nursing, 24(1), 31–50. https://doi.org/10.1188/20.CJON.31-50
Kim, E., Jahan, T., Aouizerat, B.E., Dodd, M.J., Cooper, B.A., Paul, S.M., . . . Miaskowski, C. (2009). Differences in symptom clusters identified using occurrence rates versus symptom severity ratings in patients at the end of radiation therapy. Cancer Nursing, 32(6), 429–436. https://doi.org/10.1097/NCC.0b013e3181b046ad
Kim, H.-J., Barsevick, A.M., Beck, S.L., & Dudley, W. (2012). Clinical subgroups of a psychoneurologic symptom cluster in women receiving treatment for breast cancer: A secondary analysis. Oncology Nursing Forum, 39(1), E20–E30. https://doi.org/10.1188/12.onf.e20-e30
Kim, Y., Kashy, D.A., Wellisch, D.K., Spillers, R.L., Kaw, C.K., & Smith, T.G. (2008). Quality of life of couples dealing with cancer: Dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Annals of Behavioral Medicine, 35(2), 230–238. https://doi.org/10.1007/s12160-008-9026-y
Kirkova, J., Davis, M.P., Walsh, D., Tiernan, E., O’Leary, N., LeGrand, S.B., . . . Russell, K.M. (2006). Cancer symptom assessment instruments: A systematic review. Journal of Clinical Oncology, 24(9), 1459–1473. https://doi.org/10.1200/JCO.2005.02.8332
Lapid, M.I., Atherton, P.J., Kung, S., Sloan, J.A., Shahi, V., Clark, M.M., & Rummans, T.A. (2016). Cancer caregiver quality of life: Need for targeted intervention. Psycho-Oncology, 25(12), 1400–1407. https://doi.org/10.1002/pon.3960
Larson, P.J., Carrieri-Kohlman, V., Dodd, M.J., Douglas, M., Faucett, J., Froelicher, E.S., . . . Underwood, P.R. (1994). A model for symptom management. Journal of Nursing Scholarship, 26(4), 272–276. https://doi.org/10.1111/j.1547-5069.1994.tb00333.x
Lemanska, A., Dearnaley, D.P., Jena, R., Sydes, M.R., & Faithfull, S. (2018). Older age, early symptoms and physical function are associated with the severity of late symptom clusters for men undergoing radiotherapy for prostate cancer. Clinical Oncology, 30(6), 334–345. https://doi.org/10.1016/j.clon.2018.01.016
Lenz, E.R., Pugh, L.C., Milligan, R.A., Gift, A., & Suppe, F. (1997). The middle-range theory of unpleasant symptoms: An update. Advances in Nursing Science, 19(3), 14–27.
Lin, Y., Bailey, D.E., Jr., Docherty, S.L., Porter, L.S., Cooper, B.A., Paul, S.M., . . . Miaskowski, C. (2021). Distinct profiles of multiple co-occurring symptoms in patients with gastrointestinal cancers receiving chemotherapy. Supportive Care in Cancer, 29(8), 4461–4471. https://doi.org/10.1007/s00520-020-05946-4
Maliski, S.L., Kwan, L., Elashoff, D., & Litwin, M.S. (2008). Symptom clusters related to treatment for prostate cancer. Oncology Nursing Forum, 35(5), 786–793. https://doi.org/10.1188/08.ONF.786-793
Miaskowski, C., Aouizerat, B.E., Dodd, M., & Cooper, B. (2007). Conceptual issues in symptom clusters research and their implications for quality-of-life assessment in patients with cancer. Journal of the National Cancer Institute. Monographs, (37), 39–46. https://doi.org/10.1093/jncimonographs/lgm003
Miaskowski, C., Barsevick, A., Berger, A., Casagrande, R., Grady, P.A., Jacobsen, P., . . . Marden, S. (2017). Advancing symptom science through symptom cluster research: Expert panel proceedings and recommendations. Journal of the National Cancer Institute, 109(4), djw253. https://doi.org/10.1093/jnci/djw253
Miaskowski, C., Cooper, B.A., Melisko, M., Chen, L.-M., Mastick, J., West, C., . . . Aouizerat, B.E. (2014). Disease and treatment characteristics do not predict symptom occurrence profiles in oncology outpatients receiving chemotherapy. Cancer, 120(15), 2371–2378. https://doi.org/10.1002/cncr.28699
Miaskowski, C., Cooper, B.A., Paul, S.M., Dodd, M., Lee, K., Aouizerat, B.E., . . . Bank, A. (2006). Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: A cluster analysis. Oncology Nursing Forum, 33(5), E79–E89. https://doi.org/10.1188/06.ONF.e79-e89
Miaskowski, C., Dunn, L., Ritchie, C., Paul, S.M., Cooper, B., Aouizerat, B.E., . . . Yates, P. (2015). Latent class analysis reveals distinct subgroups of patients based on symptom occurrence and demographic and clinical characteristics. Journal of Pain and Symptom Management, 50(1), 28–37. https://doi.org/10.1016/j.jpainsymman.2014.12.011
Mood, D., & Bickes, J. (1989). Strategies to enhance self-care in radiation therapy. Oncology Nursing Forum, 16(Suppl.), 143.
Muthén, B., & Muthén, L. (2018). Mplus. In W.J. van der Linden (Ed.), Handbook of item response theory, volume three: Applications. CRC Press.
Northouse, L.L., Mood, D.W., Montie, J.E., Sandler, H.M., Forman, J.D., Hussain, M., . . . Kershaw, T. (2007). Living with prostate cancer: Patients’ and spouses’ psychosocial status and quality of life. Journal of Clinical Oncology, 25(27), 4171–4177.
Northouse, L.L., Mood, D.W., Schafenacker, A., Kalemkerian, G., Zalupski, M., LoRusso, P., . . . Kershaw, T. (2013). Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncology, 22(3), 555–563. https://doi.org/10.1002/pon.3036
Nylund-Gibson, K., & Masyn, K.E. (2016). Covariates and mixture modeling: Results of a simulation study exploring the impact of misspecified effects on class enumeration. Structural Equation Modeling, 23(6), 782–797. https://doi.org/10.1080/10705511.2016.1221313
Pampel, F.C., Krueger, P.M., & Denney, J.T. (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349–370. https://doi.org/10.1146/annurev.soc.012809.102529
Papachristou, N., Barnaghi, P., Cooper, B.A., Hu, X., Maguire, R., Apostolidis, K., . . . Miaskowski, C. (2018). Congruence between latent class and k-modes analyses in the identification of oncology patients with distinct symptom experiences. Journal of Pain and Symptom Management, 55(2), 318–333.e4. https://doi.org/10.1016/j.jpainsymman.2017.08.020
Reese, J.B., Blackford, A., Sussman, J., Okuyama, T., Akechi, T., Bainbridge, D., . . . Snyder, C.F. (2015). Cancer patients’ function, symptoms and supportive care needs: A latent class analysis across cultures. Quality of Life Research, 24(1), 135–146. https://doi.org/10.1007/s11136-014-0629-4
Snyder, C.F., Garrett-Mayer, E., Blackford, A.L., Brahmer, J.R., Carducci, M.A., Pili, R., . . . Wu, A.W. (2009). Concordance of cancer patients’ function, symptoms, and supportive care needs. Quality of Life Research, 18(8), 991–998. https://doi.org/10.1007/s11136-009-9519-6
Sullivan, C.W., Leutwyler, H., Dunn, L.B., & Miaskowski, C. (2018). A review of the literature on symptom clusters in studies that included oncology patients receiving primary or adjuvant chemotherapy. Journal of Clinical Nursing, 27(3-4), 516–545. https://doi.org/10.1111/jocn.14057
Suwisith, N., Hanucharurnkul, S., Dodd, M., Vorapongsathorn, T., Pongthavorakamol, K., & Asavametha, N. (2008). Symptom clusters and functional status of women with breast cancer. Pacific Rim International Journal of Nursing Research, 12(3), 153–165. https://he02.tci-thaijo.org/index.php/PRIJNR/article/view/5869
Thavarajah, N., Chen, E., Bedard, G., Lauzon, N., Zhou, M., Chu, D., & Chow, E. (2012). Symptom clusters in patients with prostate cancer: A literature review. Journal of Pain Management, 5(4), 303–310. https://doi.org/10.1586/erp.12.41
Tometich, D.B., Small, B.J., Carroll, J.E., Zhai, W., Luta, G., Zhou, X., . . . Mandelblatt, J.S. (2019). Pretreatment psychoneurological symptoms and their association with longitudinal cognitive function and quality of life in older breast cancer survivors. Journal of Pain and Symptom Management, 57(3), 596–606.


