Personality and Spirituality as Predictors of Mental Health and Salivary Alpha-Amylase Activity in Breast Cancer Survivors
Objectives: To determine the relative predictive validity of personality and spirituality for mental health and salivary alpha-amylase (sAA) in breast cancer (BC) survivors.
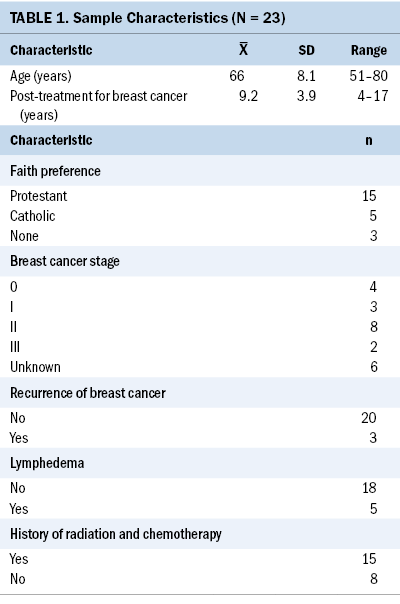
Sample & Setting: 23 BC survivors participated in a single-group, cross-sectional study.
Methods & Variables: Predictor variables included personality and spiritual variables. Outcome variables included subjective physical and mental health outcomes and sAA, a neuroimmune biomarker.
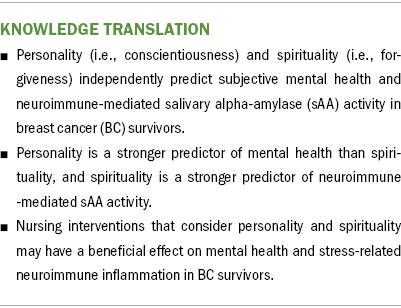
Results: Hierarchical regressions indicated that (a) conscientiousness and forgiveness independently predict 38% and 11% of variance in mental health scores, respectively; and (b) conscientiousness and forgiveness independently predict 15% and 24% of the variance in sAA, respectively. Consistent with psychoneuroimmunology theory, personality and spiritual variables independently influence subjective mental health and neuroimmune activity in BC survivors.
Implications for Nursing: Nurses should be aware of BC survivors’ personality characteristics and spiritual dispositions so that distinct interventions can be offered to promote mental health and reduce stress-related neuroimmune inflammation.
Jump to a section
Breast cancer (BC) survivors experience chronic stress and poorer mental and physical health because of ongoing psychosocial and physical symptom burdens associated with BC treatment (Eaton et al., 2020; Harrington et al., 2010). Chronic psychosocial stress in BC survivors is associated with neuroimmune inflammation, BC recurrence, and mortality (Dai et al., 2020; Mundy-Bosse et al., 2011; Witek-Janusek et al., 2007). Data suggest that BC survivors are at a 15% risk of BC recurrence in the first two years after initial diagnosis (Colleoni et al., 2016). As a result, researchers are interested in interventions that reduce stress and buffer the inflammatory neuroimmune changes that are associated with poor BC survivorship (Lengacher et al., 2019; Witek-Janusek et al., 2019).
Stress reduction is associated with better mental health in BC survivors; however, the effect of stress reduction interventions on physiologic health (e.g., neuroimmune inflammation) remains unclear (Carlson et al., 2017; Greenlee et al., 2017). Furthermore, the influence of spiritual factors (e.g., spiritual beliefs) on neuroimmune biomarkers is also unclear (Hulett & Armer, 2016). Understanding personality and spiritual variables may help explain diverse responses to stress among individuals (Soliemanifar et al., 2018).
Psychoneuroimmunology Theory
Psychoneuroimmunology theorists posit that the brain’s perception of stress is filtered through behavioral and psychosocial-spiritual variables (e.g., personality, spirituality) and communicated to the immune system via neuroimmune pathways, which results in a state of well-being or disease (Ader & Cohen, 1975; Lutgendorf & Costanzo, 2003). In short, during acute stress, the sympathetic-adrenal-medullary axis activates the sympathetic nervous system to release norepinephrine, which induces the fight-or-flight response. Following sympathetic nervous system activation, the hypothalamic-pituitary-adrenocortical axis releases endocrine-based hormones, including cortisol, which activate inflammatory protein cellular messengers (i.e., cytokines) (McEwen, 1998). The prolonged cortisol release that occurs with chronic stress is associated with dysregulation of immune cytokines such as interleukin-6, which is linked to greater susceptibility to disease and mortality (Kiecolt-Glaser et al., 2003).
Spirituality and Neuroimmune Activity
Spiritual variables refer to an individual’s emotional connection to a divine or higher power (e.g., beliefs in a loving higher power) (Johnstone, Franklin, et al., 2008). Differentiating religious and spiritual constructs is challenging because of overlapping definitions (e.g., searching for the divine). Discussions regarding the distinctions between religious versus spiritual constructs are well described in the extant literature and are beyond the scope of this article.
Spiritual variables (e.g., positive spiritual beliefs) are associated with better perceptions of general health and adjustment to illness in individuals with chronic disease (Campbell et al., 2008; Cohen et al., 2009). Jones et al. (2015) reported that positive spiritual beliefs were associated with better mental health in 199 individuals with heterogeneous health conditions (e.g., cancer, stroke, traumatic brain injury). In addition, Jones et al. (2015) noted that those who held any degree of negative spiritual beliefs (i.e., beliefs in a punishing higher power) reported poorer physical and mental health.
In a feasibility study with 41 breast cancer survivors, on which the current study is based, Hulett et al. (2018, 2021) reported that spiritual variables were associated with neuroimmune activity and self-reported mental and physical health. Specifically, salivary cortisol (i.e., the cortisol awakening response) was moderately and directly associated with positive spiritual experiences (Hulett et al., 2018). Salivary alpha-amylase (sAA) activity was directly associated with spiritual self-rank (i.e., the strength of one’s convictions) and inversely associated with forgiveness and mental and physical health (Hulett et al., 2021). Interleukin-6 was inversely associated with spiritual self-rank but directly associated with positive congregational support and mental health measures of social function and vitality (Hulett et al., 2021). These findings suggested that positive spiritual beliefs, positive support from one’s religious community, and strength of one’s convictions are associated with stronger neuroimmune activity and better mental health outcomes in BC survivors (Hulett et al., 2021).
Personality and Neuroimmune Activity
Personality is described by the Five-Factor model (also called the Big Five model), which features five dimensions: (a) neuroticism, tendency toward worries and negative affect, (b) extraversion, preference for social engagement, (c) openness, receptivity to new experiences, (d) agreeableness, sympathy toward others, and (e) conscientiousness, tendency to be responsible (McCrae & Costa, 2010). Previous data suggest that personality traits are primary predictors of health outcomes and that behavioral patterns and worldviews influence overall health (Vollrath, 2006).
In a systematic review, Soliemanifar et al. (2018) examined 26 studies, reporting mixed findings on the associations between five-factor personality traits and stress biomarkers in heterogeneous samples. The majority (19 studies) examined associations between personality and cortisol (blood, plasma, salivary, urine, or hair), but only two studies examined sAA. Inukai et al. (2010) found that sAA was positively associated with neuroticism and inversely associated with agreeableness, extraversion, and openness in healthy adults. Afrisham et al. (2015) reported that sAA was positively associated with neuroticism and agreeableness in medical students.
Few studies have examined the association between personality and psychoneuroimmunologic variables in BC survivors. In their feasibility study, Hulett et al. (2018) determined that BC survivors were not burdened by the addition of an exploratory aim to evaluate the hypothesis that personality and spirituality are associated with better mental health, physical health, and neuroimmune activity. Therefore, participants who enrolled during the latter half of the rolling recruitment period (n = 23) were invited to complete a personality inventory. This article reports the associations among personality traits, spiritual variables, mental and physical health outcomes, and neuroimmune biomarkers in the sample subset of 23 BC survivors.
Methods
Sample and Setting
The sample (N = 23) is based on a previous feasibility study (single-group, cross-sectional design) (Hulett et al., 2018). The study was approved by the University of Missouri Institutional Research Board and conducted by the Sinclair School of Nursing in collaboration with Ellis Fischel Cancer Center. Participants provided informed consent. Given the rural, Midwestern demographic, participants were offered a mail-back option for completing self-report measures to minimize travel burden. Salivary specimens were self-collected in participants’ home settings. To reduce the risk of confounding influences of treatment-related neuroimmune changes, adult women at least three months post-BC treatment were included in the study. Exclusion criteria included acute illness, steroid medication use, nicotine use, recreational drug misuse, and oral inflammation. Complete details from the parent study are reported in Hulett et al. (2018).
Variables
Self-reported measures included demographics, personality traits, spiritual variables, and mental and physical health outcomes. BC treatment histories were self-reported.
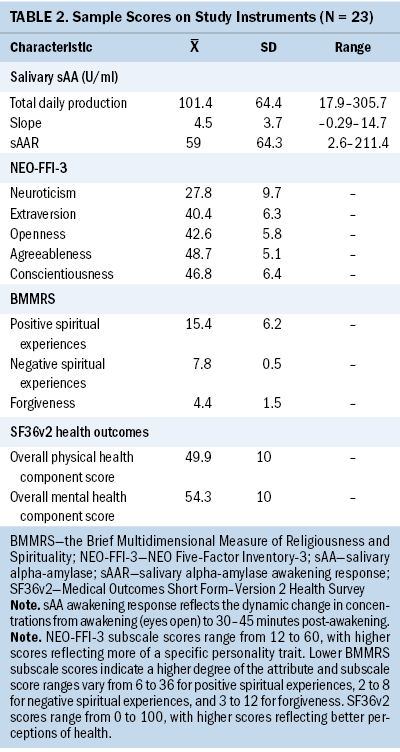
Personality: The NEO Five-Factor Inventory-3 is a 60-item measure of the five domains of personality: neuroticism, extraversion, openness, agreeableness, and conscientiousness (McCrae & Costa, 2010). For the five personality domains, Cronbach’s alpha ranges from 0.79 to 0.91 (Johnstone et al., 2012). A higher score for any given personality characteristic indicates a higher level of that characteristic.
Spirituality: Spiritual variables were measured using the Brief Multidimensional Measure of Religiousness and Spirituality (BMMRS) (Fetzer Institute & National Institute on Aging Working Group, 1999). This study used general indices of spirituality identified in a previous factor analysis of the BMMRS, including positive spirituality (i.e., belief in a loving higher power), negative spirituality (i.e., belief in a punishing higher power), and forgiveness (Johnstone, Yoon, et al., 2008). Cronbach’s alpha for the BMMRS spirituality subscales ranges from 0.72 to 0.85 (Johnstone et al., 2012). In this study, lower mean scores indicate a higher degree of the given attribute.
Health survey: The Medical Outcomes Short Form–Version 2 Health Survey is a 36-item general physical and mental health measure. Its internal consistency ranges from 0.83 to 0.95 (Ware et al., 2007). Scores were calculated using Quality Metrics scoring software and compared to 2009 general population normative data (Saris-Baglama et al., 2010; Ware et al., 2007). Physical health and mental health composite scores were used as the primary outcome measures, with higher scores equaling better health.
sAA: This protein enzyme is released by salivary glands during sympathetic nervous system responses to acute stress and correlates with plasma norepinephrine (r = 0.64) (Nater & Rohleder, 2009). SAA is an established biomarker of autonomic nervous system activity in behavioral medicine and stress research (Nater et al., 2013). Reference ranges for sAA in BC survivors have not been established (Hulett et al., 2021). Data suggest that higher levels of sAA and blunted diurnal sAA slopes indicate autonomic nervous system dysregulation in BC survivors (Wan et al., 2016).
Data Collection and Procedures
Participants were given verbal and written instructions for the self-collection of passive drool salivary specimens. Specimens were collected three times per day for two consecutive days at the three diurnal timepoints of awakening, 30–45 minutes after awakening, and evening (bedtime). The collection protocol instructed on oral intake, oral hygiene, physical activity two hours before collection, and cold storage and transport to the laboratory. BC survivors were provided with commercial sAA enzymatic kits and protocol from Salimetrics for testing sAA. Details of the enzyme immunoassay procedures and sAA parameter reporting can be found in Hulett et al. (2020).
Statistical Analyses
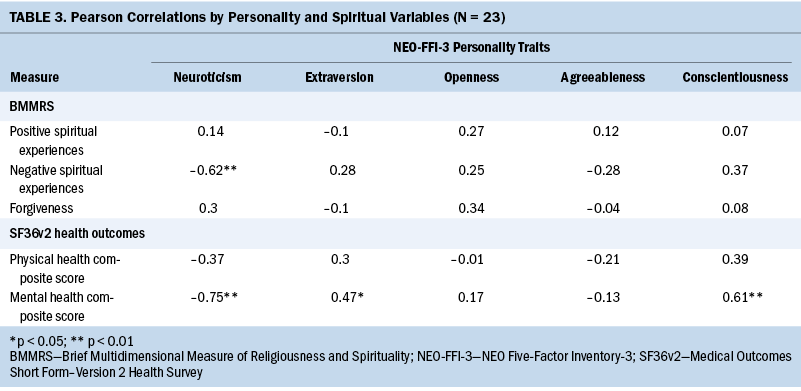
Concentrations of sAA demonstrated positive skewness on a histogram and Shapiro-Wilk testing (p < 0.01); therefore, sAA values were logarithmically transformed for statistical analyses. IBM Statistics SPSS software version 26 was used to perform statistical analyses, including descriptive statistics and correlations. Hierarchical regressions were conducted to explore associations between personality, spiritual variables, SF-36v2® health variables, and sAA. Statistical significance for all analyses was set at < 0.05. Because of the small sample size, statistical analyses were limited to one personality predictor (i.e., conscientiousness) and one spirituality predictor (i.e., forgiveness), based on Pearson’s correlation findings and data from previous studies that showed both conscientiousness and forgiveness are associated with health outcomes (Hulett et al., 2021; Johnstone et al., 2012). The neuroimmune biomarker sAA, was selected for hierarchical regression analysis based on previous findings that the association between sAA and forgiveness is statistically significant (Hulett et al., 2021).
Results
Descriptive statistics are presented in Tables 1 and 2. Pearson correlations between personality traits and demographics, spiritual variables, and physical and mental health are presented in Table 3. Spearman’s rho correlations between personality traits and sAA were not statistically significant; however, a near statistical significance was observed between neuroticism and sAA (rs = –0.34, p = 0.11) and between conscientiousness and sAA (rs = 0.37, p = 0.09).
Hierarchical Regressions
For each hierarchical regression, the first regression examined the degree to which the personality trait (i.e., conscientiousness) predicted a given outcome (i.e., mental health, sAA). The second regression determined the degree to which the spiritual variable (i.e., forgiveness) significantly predicted the given outcome after considering personality. The normal assumptions of multicollinearity, normal probability plots, and residual statistics were met.
Personality and spiritual variables as predictors of general mental health: In the first model, conscientiousness accounted for 38% of the variation in general mental health (p < 0.01). In the second model, forgiveness explained an additional 11% of the variation in general mental health after the consideration of the variance predicted by conscientiousness (p = 0.001). The total model explained 49% of the variance in general mental health (R² = 0.49, F[2, 20] = 9.57, p = 0.001) with conscientiousness (β = 0.64, p < 0.001) offering a greater contribution than forgiveness (β = –0.34, p < 0.05).
In the first model, conscientiousness accounted for 15% of the variance (p = 0.07). In the second model, forgiveness explained 24% of the variation in sAA after the consideration of conscientiousness (p < 0.05). The overall regression was significant (R² = 0.39, F[2, 20] = 6.47, p < 0.05). The total model explained 39% of the variation in sAA activity with forgiveness (β = –0.49, p < 0.05), predicting a greater contribution than conscientiousness (β = 0.43, p < 0.05).
Discussion
The results from this pilot study indicate that personality (i.e., conscientiousness) and spirituality (i.e., forgiveness) independently predict subjective and objective health (i.e., mental health and sAA) in BC survivors, providing important information regarding the psychoneuroimmunologic variables that influence BC survivorship. Personality is a stronger predictor of mental health than spirituality, a finding that supports earlier studies (Johnstone et al., 2012; Lockenhoff et al., 2009). Specifically, less neuroticism, greater extraversion, and greater conscientiousness are the personality traits most strongly associated with mental health scores. The current study’s findings are similar to those from Lai et al. (2019), who reported that neuroticism and conscientiousness predicted mental health and quality of life in BC survivors (N = 207).
Previous research has found that, in individuals treated for cancer, those who report greater expression of positive spiritual variables (i.e., forgiveness) are less likely to experience adverse psychological symptoms (e.g., depression) (Vespa et al., 2011). The current study’s findings that forgiveness independently predicts subjective mental health support those of Smith et al. (2021), who reported that positive spiritual variables, including forgiveness, are associated with mental health but not with self-reported physical health. A scoping review demonstrated that few studies had reported the relationships between forgiveness and physiologic health (Kim et al., 2020). Consequently, the finding that forgiveness predicts an objective measure of neuroimmune (i.e., sAA) activity beyond that predicted by personality is novel. Positive correlations indicate that increased spiritual scores are associated with better mental and physical health. In short, individuals who are more likely to forgive others are more likely to have better mental health and stronger neuroimmune activity, which suggests that lower stress and less resentment are associated with better mental health.
This study’s findings suggest that personality and spirituality are distinct constructs (Piedmont, 1999) that should be identified for treatment by behavioral health specialists, including nurses, and by spiritual advisors, including chaplains or clergy, for behavioral and spiritual issues, respectively. In BC survivors, positive spiritual beliefs aid in the self-management of stress and symptoms occurring during the recovery from BC treatment, which suggests that spiritual interventions may benefit BC survivors (Hulett, 2015; Sterba et al., 2014).
Few studies have investigated the association between personality, spirituality, and sAA biomarker activity. The findings of this study extend previous spirituality research by offering new empirical evidence supporting relationships between personality, spiritual variables, mental health, and sAA. Although more evidence is required, the study’s data suggest that interventions designed with consideration of personality and spirituality may have a beneficial effect on mental health and stress-related neuroimmune activity in BC survivors.
Limitations
These findings are exploratory and based on an underpowered sample. A full-scale study is necessary to better establish these associations.
Implications for Nursing and Conclusion
Personality and spirituality are theoretically and statistically distinct constructs, and they should be treated independently as such. The results of this study suggest the need for nursing clinicians to be aware of the personality characteristics and spiritual dispositions of their clients with BC so that distinct behavioral and spiritual interventions can be offered. Nurse-led behavioral interventions that consider personality and spirituality may have a beneficial effect on mental health and stress-related neuroimmune inflammation in BC survivors.
About the Authors
Jennifer M. Hulett, PhD, APRN, FNP-BC, is an assistant professor in the Sinclair School of Nursing at the University of Missouri in Columbia, MO; Brick Johnstone, PhD, is the director of acquired brain injury research at the Shepherd Center in Atlanta, GA; Rami J. Millspaugh, BS, was, at the time of data collection and analysis, a senior research specialist at the University of Missouri in Columbia, MO; and Joshua J. Millspaugh, PhD, is the Boone and Crockett professor of wildlife conservation in the Wildlife Biology Program at the University of Montana in Missoula. No financial relationships to disclose. Hulett and Johnstone contributed to the conceptualization and design. R.J. Millspaugh and J.J. Millspaugh conducted the enzyme immunoassay procedures. Hulett, R.J. Millspaugh, and J.J. Millspaugh completed the data collection. Hulett provided statistical support and the analysis. All authors contributed to the manuscript preparation. Hulett can be reached at hulettjm@missouri.edu, with copy to ONFEditor@ons.org. (Submitted August 2021. Accepted December 20, 2021.)
References
Ader, R., & Cohen, N. (1975). Behaviorally conditioned immunosuppression. Psychosomsatic Medicine, 37(4), 333–340. https://doi .org/10.1097/00006842-197507000-00007
Afrisham, R.S.-N., Solimanifar, S., Abromand, O., Kooti, M., Najjar-Asi, W., & Khaneh-Keshi, S.A. (2015). Evaluating the salivary alpha-amylase level under psychological stress and its relationship with rumination and the five personality traits. Journal of Mazandaran University of Medical Sciences, 25(126), 22–33.
Campbell, J.D., Yoon, D.-P., & Johnstone, B. (2008). Determining relationships between physical health and spiritual experience, religious practices, and congregational support in a heterogeneous medical sample. Journal of Religion and Health, 49(1), 3–17. https://doi.org/10.1007/s10943-008-9227-5
Carlson, L.E., Zelinski, E., Toivonen, K., Flynn, M., Qureshi, M., Piedalue, K.A., & Grant, R. (2017). Mind-body therapies in cancer: What is the latest evidence? Current Oncology Reports, 19(10), 67.
Cohen, D., Yoon, D.P., & Johnstone, B. (2009). Differentiating the impact of spiritual experiences, religious practices, and congregational support on the mental health of individuals with heterogeneous medical disorders. International Journal for the Psychology of Religion, 19(2), 121–138.
Colleoni, M., Sun, Z.X., Price, K.N., Karlsson, P., Forbes, J.F., Thurlimann, B., . . . Goldhirsch, A. (2016). Annual hazard rates of recurrence for breast cancer during 24 years of follow-up: Results from the International Breast Cancer Study Group Trials I to V. Journal of Clinical Oncology, 34(9), 927–935. https://doi.org/10.1200/JCO.2015.62.3504
Dai, S.R., Mo, Y.Z., Wang, Y.M., Xiang, B., Liao, Q.J., Zhou, M., . . . Zeng, Z.Y. (2020). Chronic Stress Promotes Cancer Development. Frontiers in Oncology, 10, 1492. https://doi.org/10.3389/fonc.2020.01492
Eaton, L.H., Narkthong, N., & Hulett, J.M. (2020). Psychosocial issues associated with breast cancer-related lymphedema: A literature review. Current Breast Cancer Reports, 12(4), 1–9. https://doi.org/10.1007/s12609-020-00376-x
Fetzer Institute & National Institute on Aging Working Group. (1999). Multidimensional measurement of religiousness/spirituality for use in health research: A report of the Fetzer Institute/National Institute on Aging Working Group. Fetzer Institute. https://fetzer .org/resources/multidimensional-measurement-religiousnessspirituality-use-health-research
Greenlee, H., DuPont-Reyes, M.J., Balneaves, L.G., Carlson, L.E., Cohen, M.R., Deng, G., . . . Tripathy, D. (2017). Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: A Cancer Journal for Clinicians, 67(3), 194–232. https://doi.org/ 10.3322/caac.21397
Harrington, C.B., Hansen, J.A., Moskowitz, M., Todd, B.L., & Feuerstein, M. (2010). It’s not over when it’s over: Long-term symptoms in cancer survivors—A systematic review. International Journal of Psychiatry in Medicine, 40(2), 163–181. https://doi.org/10.2190/PM.40.2.c
Hulett, J.M., Abshire, D.A., Armer, J.M., Millspaugh, R., & Millspaugh, J. (2020). Rural-urban differences in neuroimmune biomarkers and health status among women living with breast cancer. Cancer Nursing, 44(4), 323–332. https://doi.org/10.1097/NCC.0000000000000802
Hulett, J.M., & Armer, J.M. (2016). A systematic review of spiritually-based interventions and psychoneuroimmunological outcomes in breast cancer survivorship. Integrative Cancer Therapies, 15(4), 405–423. https://doi.org/ 10.1177/1534735416636222
Hulett, J.M., Armer, J.M., Leary, E., Stewart, B.R., McDaniel, R., Smith, K., . . . Millspaugh, J. (2018). Religiousness, spirituality, and salivary cortisol in breast cancer survivorship: A pilot study. Cancer Nursing, 41(2), 166–175. https://doi.org/10.1097/ncc.0000000000000471
Hulett, J.M., Armer, J.M., Stewart, B.R., & Wanchai, A. (2015). Perspectives of the breast cancer survivorship continuum: Diagnosis through 30 months post-treatment. Journal of Personalized Medicine, 5(2), 174–190.
Hulett, J.M., Johnstone, B., Armer, J.M., Deroche, C., Millspaugh, R., & Millspaugh, J. (2021). Associations between religious and spiritual variables and neuroimmune activity in survivors of breast cancer: A feasibility study. Supportive Care in Cancer, 29(11), 6421–6429. https://doi.org/10.1007/s0052 0-021-06224-7
Inukai, K., Shinada, M., Tanida, S., Takahashi, C., Mifune, N., Takagishi, H., . . . Takahashi, T. (2010). Salivary alpha-amylase levels and big five personality factors in adults. Neuroendocrinology Letters, 31(6), 771–774.
Johnstone, B., Franklin, K.L., Yoon, D.P., Burris, J., & Shigaki, C. (2008). Relationships among religiousness, spirituality, and health for individuals with stroke. Journal of Clinical Psychology in Medical Settings, 15(4), 308–313. https://doi.org/10.1007/s10880-008-9128-5
Johnstone, B., Yoon, D.P., Cohen, D., Schopp, L.H., McCormack, G., Campbell, J., & Smith, M. (2012). Relationships among spirituality, religious practices, personality factors, and health for five different faith traditions. Journal of Religion and Health, 51(4), 1017–1041. https://doi.org/10.1007/s10943-012-9615-8
Johnstone, B., Yoon, D.P., Franklin, K.L., Schopp, L., & Hinkebein, J. (2008). Re-conceptualizing the factor structure of the brief multidimensional measure of religiousness/spirituality. Journal of Religion and Health, 48(2), 146–163. https://doi.org/10.1007/s10943-008-9179-9
Jones, A., Cohen, D., Johnstone, B., Yoon, D.P., Schopp, L.H., McCormack, G., & Campbell, J. (2015). Relationships between negative spiritual beliefs and health outcomes for individuals with heterogeneous medical conditions. Journal of Spirituality in Mental Health, 17(2), 135–152. https://doi.org/10.1080/19349637.2015.1023679
Kiecolt-Glaser, J.K., Preacher, K.J., MacCallum, R.C., Atkinson, C., Malarkey, W.B., & Glaser, R. (2003). Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences of the United States of America, 100(15), 9090–9095.
Kim, J.S., Hulett, J.M., & Heiney, S.P. (2020). Forgiveness and health outcomes in cancer survivorship: A scoping review. Cancer Nursing, 44(4), e181–e192. https://doi.org/ 10.1097/NCC.0000000000000809
Lai, H.L., Chen, C.I., Lu, C.Y., Yao, Y.C., & Huang, C.Y. (2019). Relationships among personality, coping, and concurrent health-related quality of life in women with breast cancer. Breast Cancer, 26(5), 544–551. https://doi.org/10.1007/s12282-019-00954-7
Lengacher, C.A., Reich, R.R., Paterson, C.L., Shelton, M., Shivers, S., Ramesar, S., . . . Park, J.Y. (2019). A large randomized trial: Effects of mindfulness-based stress reduction (MBSR) for breast cancer (BC) survivors on salivary cortisol and IL-6. Biological Research for Nursing, 21(1), 39–49. https://doi.org/ 10.1177/1099800418789777
Lockenhoff, C.E., Ironson, G.H., O’Cleirigh, C., & Costa, P.T., Jr. (2009). Five-factor model personality traits, spirituality/religiousness, and mental health among people living with HIV. Journal of Personality, 77(5), 1411–1436.
Lutgendorf, S.K., & Costanzo, E.S. (2003). Psychoneuroimmunology and health psychology: An integrative model. Brain, Behavior, and Immunity, 17(4), 225–232. https://doi.org/10.1016/s0889-1591(03)00033-3
McCrae, R., & Costa, P., Jr. (2010). Professional manual for the NEO inventories: NEO-PI-3, NEO-PI-R, and NEO-FFI-3. Psychological Assessment Resources.
McEwen, B.S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338(3), 171–179. https://doi.org/10.1056/NEJM199801153380307
Mundy-Bosse, B.L., Thornton, L.M., Yang, H.C., Andersen, B.L., & Carson, W.E. (2011). Psychological stress is associated with altered levels of myeloid-derived suppressor cells in breast cancer patients. Cellular Immunology, 270(1), 80–87. https://doi.org/10.1016/j.cellimm.2011.04.003
Nater, U.M., & Rohleder, N. (2009). Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology, 34(4), 486–496. https://doi.org/10.1016/j.psyneuen.2009.01.014
Nater, U.M., Skoluda, N., & Strahler, J. (2013). Biomarkers of stress in behavioural medicine. Current Opinion in Psychiatry, 26(5), 440–445. https://doi.org/10.1097/YCO.0b013e328363b4ed
Piedmont, R.L. (1999). Does spirituality represent the sixth factor of personality? Spiritual transcendence and the Five-Factor Model. Journal of Personality, 67(6), 985–1013. https://doi.org/ 10.1111/1467-6494.00080
Saris-Baglama, R.N., Dewey, C.J., Chisholm, G.B., Plumb, E., King, J., Rasicot, P., . . . Ware, J.E., Jr. (2010) QualityMetric Health Outcomes™ scoring software 4.0 User’s guide. QualityMetric, Inc.
Smith, E.I., Yoon, D.P., Bruininks, P., Witvliet, C.V.O., Cohen, D., Edman, L.R.O., . . . Johnstone, B. (2021). Relationships between psychometrically distinct Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS) factors and mental health among U.S. college students. Mental Health, Religion, and Culture, 24(2), 211–225. https://doi.org/10.1080/13674676 .2021.1871596
Soliemanifar, O., Soleymanifar, A., & Afrisham, R. (2018). Relationship between personality and biological reactivity to stress: A review. Psychiatry Investigation, 15(12), 1100–1114. https://doi.org/10.30773/pi.2018.10.14.2
Sterba, K.R., Burris, J.L., Heiney, S.P., Ruppel, M.B., Ford, M.E., & Zapka, J. (2014). “We both just trusted and leaned on the Lord:” A qualitative study of religiousness and spirituality among African American breast cancer survivors and their caregivers. Quality of Life Research, 23(7), 1909–1920. https://doi.org/10.1007/s11136-014-0654-3
Vespa, A., Jacobsen, P.B., Spazzafumo, L., & Balducci, L. (2011). Evaluation of intrapsychic factors, coping styles, and spirituality of patients affected by tumors. Psycho-Oncology, 20(1), 5–11. https://doi.org/10.1002/pon.1719
Vollrath, M.E. (2006). Handbook of personality and health. John Wiley & Sons. https://doi.org/10.1002/9780470713860
Wan, C., Couture-Lalande, M., Narain, T.A., Lebel, S., & Bielajew, C. (2016). Salivary alpha-amylase reactivity in breast cancer survivors. International Journal of Environmental Research and Public Health, 13(4), 353. https://doi.org/10.3390/ijerph13040353
Ware, J., Kosinski, M., Bjorner, J., Turner-Bowker, D., Gandek, B., & Maruish, M. (2007). User’s guide for the SF-36v2 Health Survey (2nd ed.). QualityMetric Inc.
Witek-Janusek, L., Gabram, S., & Mathews, H.L. (2007). Psychologic stress, reduced NK cell activity, and cytokine dysregulation in women experiencing diagnostic breast biopsy. Psychoneuroendocrinology, 32(1), 22–35. https://doi.org/ 10.1016/j.psyneuen.2006.09.011
Witek-Janusek, L., Tell, D., & Mathews, H.L. (2019). Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: A randomized trial with active control. Brain, Behavior, and Immunity, 80, 358–373. https://doi.org/10.1016/j.bbi.2019.04.012