Interprofessional Oncology Providers’ Experiences and Knowledge of Opioid Use Disorders in Patients With Cancer
Objectives: To determine oncology providers’ experiences and knowledge of opioid use disorders (OUDs) in patients with cancer.
Sample & Setting: The final sample of 773 participants included 42 physicians, 213 advanced practice providers (APPs), and 518 nurses at a large comprehensive cancer center.
Methods & Variables: This study used a cross-sectional descriptive survey to describe providers’ experiences and knowledge of OUDs.
Results: Nurses and APPs reported personal experiences with addiction and encountering issues with OUDs in patients more often compared to physicians. Knowledge deficits were identified regarding addiction, including evidence-based treatment for OUDs. Overall, OUDs are a topic of concern that the majority of oncology providers are interested in learning more about.
Implications for Nursing: The opioid epidemic presents an opportunity to improve the knowledge of interprofessional oncology providers addressing OUDs. Nurses and APPs are ideally positioned for the prevention and early recognition of patients with an OUD and cancer.
Jump to a section
The opioid epidemic is a public health crisis, devastating families and communities in the United States in lives lost and economic expenditures. In 2019, 10.1 million Americans aged 12 years or older reported opioid misuse, with 92.1% involving only prescription medications, 3.4% using only heroin, and 4% using prescription medications and heroin (Substance Abuse and Mental Health Services Administration, 2020a). Opioid use disorders (OUDs), a subtype of substance use disorders (SUDs), are complex, caused by underlying changes in the brain circuitry, resulting in a pathologic pattern of behaviors (American Psychiatric Association, 2013). An OUD is considered a medical illness, although misconceptions exist, with the belief by some that addiction is a weakness, lifestyle choice, and moral failing (Adams et al., 2021). These misbeliefs drive barriers to receiving high-quality care and may result in dismal outcomes, such as disease progression from treatment delays related to nonadherence or complications, increased symptoms, and ultimately death (Yusufov et al., 2019).
Severe pain is a feared consequence associated with a cancer diagnosis. A meta-analysis by van den Beuken-van Everdingen et al. in 2016 reported the prevalence of pain as 55% during curative treatment and nearly 40% following, with 38% of all patients rating pain as moderate to severe. Opioid exposure to treat cancer-related pain may increase the likelihood of individuals relapsing or developing an OUD (Amaram-Davila et al., 2020; Dowell et al., 2016; Pinkerton & Hardy, 2017). There is an increased awareness of the risks of opioid addiction and misuse among individuals with cancer (Sager & Childers, 2019). Understandably, the prevalence of OUDs in this population is unclear. A systematic review identified seven studies examining opioid use in patients with cancer, with the median opioid misuse rate being 18% (range = 2%–43%); only one study included heroin, with no patients reporting heroin use (Yusufov et al., 2019). Challenges included different terminology between the studies, as well as the various methods to measure substance use (Yusufov et al., 2019). More recently, a prospective study found 19.2% (n = 299) of patients reported one nonmedical opioid use behavior or more. The total sample included 1,554 patients with cancer receiving opioids for cancer-related pain (Yennurajalingam et al., 2021). A systematic review of the adult chronic noncancer pain literature reported the estimated prevalence of problematic use of opioids as 36.3% (95% confidence interval [27.4%, 45.2%]) (Jantarada et al., 2021).
Little is known about the experiences and knowledge of oncology providers related to OUDs in patients with cancer. Often, OUDs are discussed in the context of providing palliative care and pain management. Results from one retrospective, matched case-control analysis of patients hospitalized with cancer-related pain suggested patients with OUDs received lower quality of pain management (Singh et al., 2021). Proposed clinician-specific barriers included limited knowledge and training, as well as bias and discrimination (Singh et al., 2021). A qualitative study explored the problems and needs of healthcare professionals and volunteers providing palliative care to patients with SUDs. Areas for improvement included the lack of formal knowledge, stigma, and insufficient resources (Ebenau et al., 2020).
The Ohio State University Comprehensive Cancer Center–Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (The James) in Columbus, Ohio, serves central and southern Ohio and northern West Virginia, which are areas hit hard by the opioid epidemic (MacKinnon & Privitera, 2020). Identifying knowledge gaps is the first step to tailor future education strategies for oncology providers. A hospitalwide survey was conducted with the primary objective to determine oncology providers’ experiences and knowledge of OUDs in patients with cancer. Secondary objectives were evaluating future learning interest and learning preferences for increasing provider awareness and knowledge related to OUDs.
Methods
Sample and Setting
Healthcare providers employed at the institution (N = about 2,580) were invited to participate in the research study, including full-time, part-time, and contingent staff as follows: physicians (n = about 900), advanced practice providers (APPs) (advance practice nurses, physician assistants, and pharmacists) (n = about 480), and nurses (n = about 1,200). Other provider types, such as physical or occupational therapists, patient care associates, and unit clerks, were excluded. Because all healthcare providers described were invited to participate, a sample size estimation was not conducted prior to beginning the study.
Design and Data Collection
This study was a cross-sectional, descriptive survey of interprofessional healthcare providers at The James, including the satellite ambulatory sites. Following hospital administration and institutional review board review, all potential participants received an invitation email with a link to participate in an online survey anytime during a four-week period in January and February 2020. Potential participants received weekly reminder emails. The consent and administration of the survey used REDCap (Harris et al., 2009, 2019). Once informed consent was obtained, interested participants could proceed with the survey. Participation was voluntary, and identifiers (email address) were removed from the data set to de-identify respondents. At survey completion, the participants had the option to voluntarily include an email address to receive a $5 gift card to the hospital coffee shop. Data were collected using REDCap and analyzed using SAS, version 9.4.
Measures
Participants were asked to complete a 29-question survey mainly exploring the experiences with and knowledge related to OUDs. Participant demographic and clinical practice information was also collected. The survey was created by the authors, based on their clinical experience, and took less than 10 minutes to complete. Feedback and face and content validity were provided by three physicians working in addiction medicine and a public health professor. This article focuses on questions related to baseline experiences, including personal and clinical encounters and knowledge of OUDs. Future interest in learning more about OUDs and preferred methods to receive this information are reviewed.
Data Analysis
Survey responses were summarized using appropriate descriptive statistics (mean and standard deviation [for continuous and symmetric data], median and interquartile range [for skewed data], or counts [for categorical variables]). The responses were compared across different oncology healthcare provider groups (physicians, APPs, and nurses) using chi-square or Fisher exact tests for categorical data and one-way analysis of variance or Kruskal–Wallis tests for continuous data, with a significance level of 0.05. For significant results, additional pairwise comparisons were made among the three healthcare provider groups using the appropriate method (t tests, chi-square tests, Fisher exact tests), with a Bonferroni corrected significance level of 0.017.
Results
Sample Characteristics
Of the approximate 2,580 potential participants, 847 (33%) completed the survey. Seventy-four participants were excluded because provider type could not be determined (unclear or ineligible provider type, such as social worker), for a final sample of 773. This included 42 physicians, 213 APPs (180 advanced practice nurses or physician assistants and 33 pharmacists), and 518 nurses. The response rates were 5% for physicians, 50% for advanced practice nurses and physician assistants, 28% for pharmacists, and 43% for nurses. The majority of the participants were female (n = 676, 87%) and White (n = 692, 90%), with an overall mean age of 38.8 years (SD = 11). A greater percentage of physicians were male (n = 23, 55%) and non-White (n = 14, 33%). Fewer nurses had at least a master’s degree (n = 69, 13%), compared to all physicians (n = 42, 100%) and nearly all APPs (n = 205, 96%) (p < 0.001). More than half of the sample had worked in oncology for six years or longer (n = 406, 53%). A greater percentage of nurses only worked inpatient (n = 273, 53%), compared to physicians (n = 3, 7%) and APPs (n = 85, 40%) (p < 0.001). Participant characteristics are summarized in Table 1.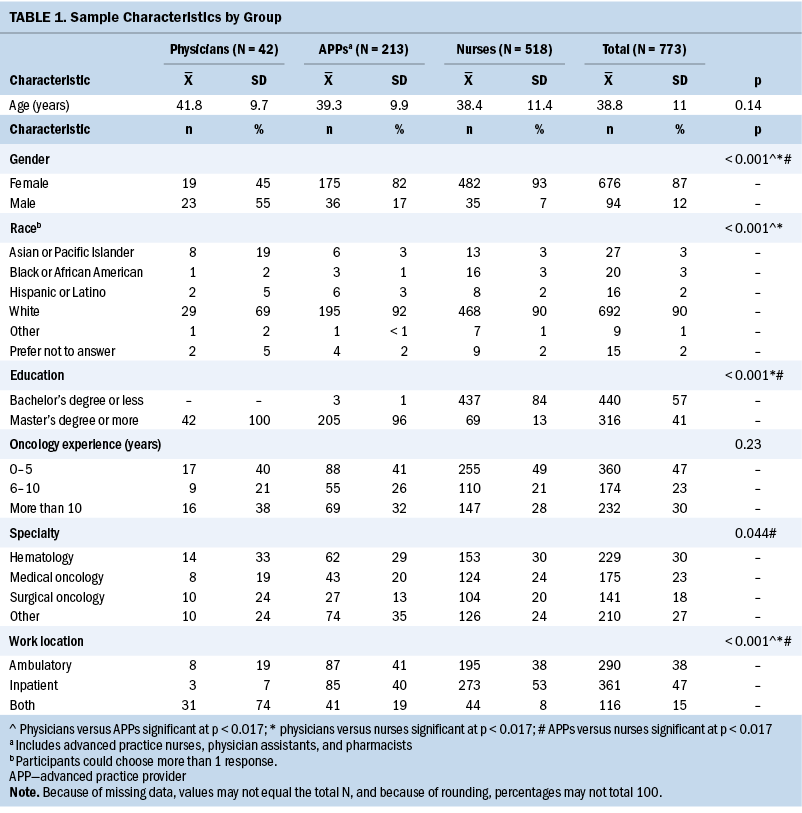
Primary Objective: To Determine Oncology Providers’ Experiences and Knowledge of OUDs
Personal experience was defined as either self or knowing a close associate (family, friend, or coworker) affected by a SUD. About half (n = 405, 52%) of all participants acknowledged personal experience with SUDs; however, this differed by provider type, with only 29% of physicians (n = 12) reporting such experience, compared to 55% of APPs (n = 117) and 53% of nurses (n = 276) (p = 0.003). Clinical experience questions asked about the frequency they encountered issues related to OUDs. Participants reported rarely or occasionally experiencing these issues with their patient population (n = 527, 68%), although this differed by group. For example, more APPs reported this as often (n = 72, 34%). No training or education related to OUDs was reported by 23% of nurses (n = 120), compared to 17% of APPs (n = 37) and 7% of physicians (n = 3) (p = 0.013). Nurses reported more often that they did not have confidence addressing OUDs (n = 205, 40%), although this was not significantly different from other providers (p = 0.16).
Several statements evaluated participants’ knowledge related to OUDs. Most participants recognized the statement, “Pain protects people from addiction to opioids,” as false (n = 592, 77%). “People with OUDs can control their addiction and use” was correctly acknowledged as false by many participants (n = 503, 65%). Only 40% of nurses (n = 207), compared to 60% of physicians (n = 25) and 57% of APPs (n = 121), discerned the statement, “Medication-assisted therapy replaces one addiction with another,” as false (p < 0.001). Eighty-five percent of nurses (n = 440) agreed with the statement, “I am certain I treat all people the same, regardless of current or past OUDs,” in contrast to 64% of physicians (n = 27) and 76% of APPs (n = 162) (p < 0.001). Of note, almost half of the sample (n = 346, 45%) correctly disagreed or strongly disagreed with the statement, “I am certain that stereotypes or bias do not affect the quality of care patients receive.” More nurses agreed with this statement (n = 265, 51%) compared to physicians (n = 18, 43%) or APPs (n = 90, 42%). Complete results for experience and knowledge questions are provided in Table 2. 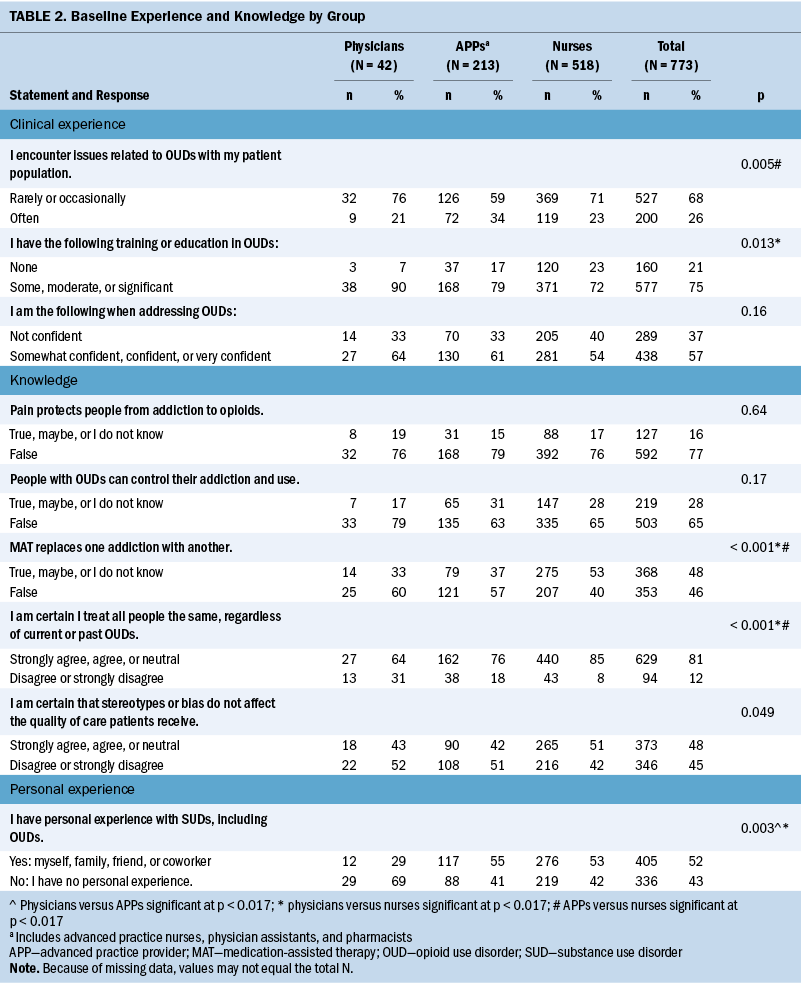
Secondary Objectives: Future Interest in Learning More About OUDs and Preferred Methods to Receive This Information
OUD was a topic of concern for the majority of providers (n = 573, 74%). This concern was shared consistently across all provider types (p = 0.29). OUDs are a subject of universal interest, with 90% of all respondents (n = 694) indicating at least some level of interest in learning more about OUDs (p = 0.55). Refer to Table 3 for complete results. 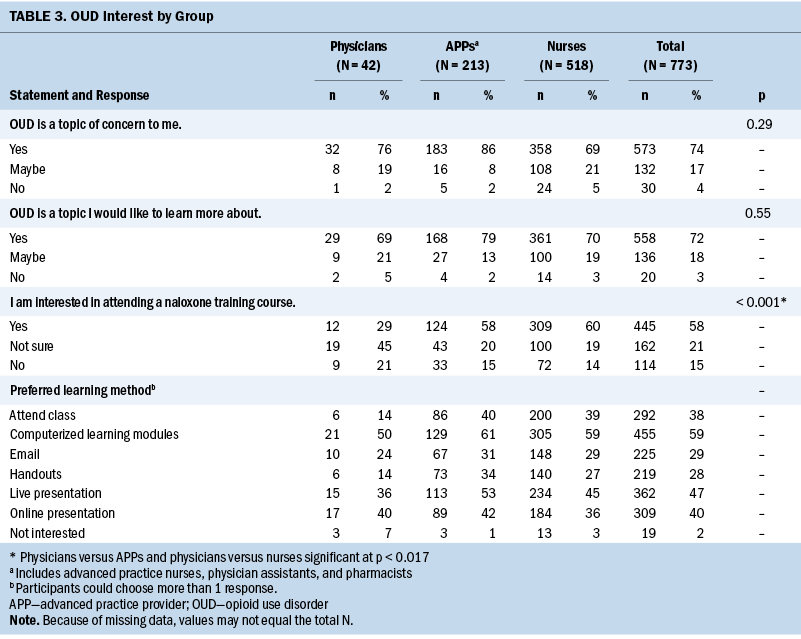
The most popular preferred learning methods were computerized learning modules (n = 455, 59%), followed by presentations, both live (n = 362, 47%) and online (n = 309, 40%). The least desirable approaches were handouts (n = 219, 28%) and email (n = 225, 29%). Interest in attending a naloxone training course varied among providers; 12 physicians (29%) expressed interest, compared to 309 nurses (60%).
Discussion
Opioids are used to treat cancer-related pain, and the opioid epidemic does not exclude oncology. However, providers may be less aware that opioid misuse risk exists among patients with cancer; this contributes to the under-recognition of risk and the implementation of mitigation strategies. To the authors’ knowledge, this is the first study exploring interprofessional oncology providers’ experiences and knowledge of OUDs. Results will inform future instruction methods. Nurses and APPs reported personal experiences with OUDs, as well as encountering OUD issues with patients more often, compared to physicians. Despite this increased exposure, a greater percentage of both reported having no training or education specific to OUDs, compared to physicians. Because less formal education is required, there may be fewer opportunities for OUD content. Regardless of training, almost 40% (n = 289) of providers lacked confidence in addressing OUDs. Conversations with patients regarding opioid use are challenging and difficult for providers. Key communication strategies include validating pain and suffering, such as by simply acknowledging, “I know you have pain.” Cultivating and maintaining a therapeutic alliance while minimizing stigma allows providers to address opioid use and nonmedical consumption. Providers should ask directly regarding opioid use or misuse and express concerns regarding harms (Sager & Childers, 2019).
SUDs are not uncommon in the general population. Addiction can be a highly misunderstood and stigmatized chronic illness and may be encountered while providing routine medical care, including cancer screenings, treatment, and survivorship care. Knowledge deficits promote the development of misconceptions, which may contribute to the development of healthcare stigma (Compton & Blacher, 2020). For example, nearly 20% (n = 127) of providers believed or were not sure if pain protects people from addiction to opioids. Almost one-third of providers (n = 219) answered true, maybe, or do not know to the statement “People with OUDs can control their addiction and use.” Both of these statements are false (Tyson et al., 2021). Another example is the number of participants agreeing that medication-assisted therapy may replace one addiction with another. Medication for OUD provides evidence-based treatment for OUDs (Substance Abuse and Mental Health Services Administration, 2020b).
The current results suggest that OUDs are a topic of concern providers are interested in learning about. There is a distinctive opportunity for the dissemination of current knowledge regarding the science, treatment, and management of OUDs. Oncology providers may not self-identify their role as assisting with substance use. Clear communication of the importance of providing holistic care is imperative for all providers, particularly APPs and nurses (Russell et al., 2017). Approaches for prevention and risk mitigation can also be discussed. Instruction focusing on substance use increases confidence and competence while decreasing stigma (Compton & Blacher, 2020).
Limitations
Several limitations of this study need to be considered. Generalizability is limited from this single-center study, which was conducted at an urban, comprehensive cancer center, where there may have been more exposure to OUD resources. Results may have been different in community-based and rural oncology practices. A large proportion of the study participants were White (90%) and female (87%), although this was less true for physicians. Even so, more diverse participants likely would have similar results. Future studies should include different settings with more diverse participants to increase generalizability.
Threats to internal validity include selection bias. Addiction may be a highly sensitive topic for those with personal experience with addiction, and they may have opted not to participate. SUDs are highly stigmatized; although surveys were anonymous, participants may have been dishonest regarding personal experiences or may have felt pressured to submit socially desirable answers to items. Likewise, providers with an interest in OUDs, as well as those with a perceived deficiency in knowledge, may have been more likely to participate in the survey. Maturation may also play a role because participants may have been exposed to information or education on OUDs from the media and other outside forces. Survey respondents could not be compared to nonrespondents because of the anonymity of the study. The survey was created by the authors and was not formally tested for validity and reliability, although face and content validity were established before distribution.
Lastly, the survey was administered prior to the COVID-19 pandemic. Many of the educational options have since been modified. Personal comfort level and capability have improved with technology, expanding opportunities for the delivery of information.
Implications for Nursing and Research
Oncology providers should be prepared to treat patients with cancer from a variety of backgrounds with an assortment of comorbid conditions. A cancer diagnosis may provide the ideal opportunity to prevent and prompt recognition of OUDs, allowing for the implementation of mitigation strategies. These are opportunities to coordinate care, such as referral for parallel treatment and management of coexisting OUDs, thereby simplifying workloads for patients and families. Cultivation of personalized techniques to treat adverse symptoms and complications, including from concurrent addiction, across diverse populations will improve symptom science. Oncology nurses have a strong foundation and are in ideal roles to lead teams implementing innovative ways to address addiction in patients with cancer using a broad public health approach.
Further research is needed to fully understand oncology providers’ interest in OUDs. Findings support the development and implementation of innovative training modules within a harm reduction toolkit; this would combine instruction on knowledge gaps, such as addiction biology and treatment, and increase awareness of OUDs as a chronic disease. This includes the appropriate terminology providers should use to communicate with others. Language may encourage judgment and directly affect the attitudes and practices of interprofessional colleagues and students, extending into communities and affecting patients and loved ones affected by OUDs. Content from the harm reduction toolkit could be piloted in a variety of practice settings, with multiple delivery tactics, encompassing many specialties and provider roles. Knowledge and attitudes could be examined after completion. Patient outcome data could also be captured, such as recognition, referral, healthcare utilization, adherence to cancer treatment, and appointments.
Conclusion
Interprofessional oncology providers, particularly nurses, have personal and clinical experiences with addiction. Providers are concerned regarding OUDs and have a great interest in learning more about this topic. Treatment for OUDs is ongoing and lifelong. Nurses and APPs have close contact with patients during their cancer journey and are important in the prevention and early identification of patients with OUDs. Providing patient-centered care allows for the implementation of strategies to facilitate adherence and reduce harmful complications, subsequently improving outcomes. Innovative approaches to address provider knowledge gaps will enhance compassion and understanding, ultimately removing barriers to high-quality care.
The authors gratefully acknowledge Kris Kipp, MSN, RN, and The James for their continuous support to positively affect the opioid epidemic, as well as Julie Teater, MD, Margaret “Peggy” Williams, MD, Emily Kaufman, DO, MPH, and Pam Salsberry, PhD, RN, FAAN, for providing face and content validity for the questionnaire. The authors also gratefully acknowledge Carlton Brown, RN, PhD, AOCN®, FAAN, for proofreading and providing constructive feedback of this article.
About the Author(s)
Gretchen A. McNally, PhD, ANP-BC, AOCNP®, is a hematology nurse practitioner and nurse scientist at the Ohio State University Comprehensive Cancer Center–Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (The James), Eric M. McLaughlin, MS, is a biostatistician 1 in the Center for Biostatistics, Robin Rosselet, DNP, APRN-CNP/CNS, AOCN®, is the director of advanced practice providers, research, and evidence-based practice at The James and an assistant professor of practice in the College of Nursing, and Robert Baiocchi, MD, PhD, is a professor of internal medicine in the Division of Hematology in the College of Medicine, all at the Ohio State University in Columbus. This research was supported by the Ohio State University Center for Clinical and Translational Science grant support (National Center for Advancing Translational Sciences, Grant UL1TR002733). Baiocchi has served on the advisory boards for Viracta Therapeutics and Prelude Therapeutics and participated in the American Society of Hematology Minority Recruitment Initiative. McNally and Rosselet contributed to the conceptualization and design. McNally completed the data collection. McNally and McLaughlin provided statistical support. McNally, McLaughlin, and Baiocchi provided the analysis. McNally, McLaughlin, and Rosselet contributed to the manuscript preparation. McNally can be reached at gretchen.mcnally@osumc.edu, with copy to ONFEditor@ons.org. (Submitted April 2021. Accepted October 22, 2021.)

