An Integrative Review of the Role of Nurses in Fertility Preservation for Adolescents and Young Adults With Cancer
Problem Identification: Adolescents and young adults (AYAs) with cancer commonly report future fertility as an important issue in care. Despite long-standing guidelines on fertility counseling and the trusting relationship between nurses and patients, little is known about the nurse’s role in fertility preservation (FP) for AYAs with cancer.
Literature Search: The authors conducted a literature search of articles published through 2020 focused on nursing involvement in FP for AYAs with cancer.
Data Evaluation: 85 studies were identified. In total, 11 articles met inclusion criteria and were critically appraised in the review.
Synthesis: Although well positioned to improve FP care among AYAs with cancer, nurses currently have a minimal role because of provider, institutional, and patient-related barriers.
Implications for Practice: Interventions to enhance nurses’ knowledge about FP, improvements in electronic health record documentation, and facilitation of institutional support are needed to support the nurse’s role in FP for AYAs with cancer.
Jump to a section
In the United States, about 89,500 new cancer diagnoses among adolescents (ages 15–19 years) and young adults (ages 20–39 years) (AYAs) were estimated in 2020 (American Cancer Society [ACS], 2020). Although the incidence rates for AYAs are rising at a rate greater than other age groups, the five-year survival for AYAs ranges from 83% to 86%, compared to 84% for children and 66% for adults (ACS, 2020). There are more than 1.6 million cancer survivors of reproductive age (ACS, 2019). With the growing survival rates among AYAs, patient-centered care that addresses treatment and survivorship care needs is becoming more relevant.
Although AYAs with cancer identify fertility as a top concern of cancer care, many often face infertility as a common treatment side effect (Benedict et al., 2015; Klosky et al., 2014; Su et al., 2018). Fertility concerns remain highly prevalent at diagnosis and throughout survivorship (Su et al., 2018), with AYAs commonly prioritizing their fertility over home ownership and wealth (Klosky et al., 2014). For both sexes, infertility alone often leads to distress and diminished quality of life (QOL), affecting one’s emotional well-being, sexuality, and relationships (Duffy & Allen, 2009). Fertility preservation (FP) is not always prioritized for adolescents because of age-related challenges; adolescents may not possess the maturity level to appreciate future fertility and often defer to parental support (Anazodo, Ataman-Millhouse, et al., 2018). The impact of infertility on QOL is even greater for those who did not receive adequate information prior to treatment initiation (Goossens et al., 2015; Vadaparampil & Quinn, 2013). AYAs affected by infertility are twice as likely to experience depression (Duffy & Allen, 2009). Therefore, it is imperative that clinicians identify patients of reproductive age and incorporate discussions about fertility in the plan of care.
To meet AYA fertility needs, numerous national healthcare organizations, including the American Society of Clinical Oncology (ASCO), American Society for Reproductive Medicine, American College of Obstetricians and Gynecologists, National Comprehensive Cancer Network, and American Academy of Pediatrics have issued FP practice guidelines. In 2018, ASCO issued clinical practice guidelines for healthcare providers to address fertility risks as early as possible and document FP discussions in the electronic health record (Oktay et al., 2018). However, evidence suggests that many providers do not disclose the risks of treatment-related infertility or do so inadequately (Lee et al., 2006; Quinn et al., 2009, 2015; Su et al., 2018). A referral to a reproductive specialist is also recommended by ASCO to facilitate FP procedures, given that many oncology providers report being unaware of or uncomfortable discussing FP with patients (Oktay et al., 2018). Standard FP procedures for males consist of sperm cryopreservation, and standard FP procedures for females include oocyte and embryo cryopreservation (Fernbach et al., 2014; Oktay et al., 2018).
Despite long-standing guidelines on fertility counseling, a significant gap remains in fertility care of AYAs with cancer (Flink et al., 2017). Intervention and implementation studies to improve FP education for AYAs are in their infancy and limited in scope (Johnson & Kroon, 2013; Su et al., 2018). To meet practice guidelines and to improve outcomes for AYAs with cancer, healthcare systems must intentionally improve access to FP throughout cancer treatment. Accordingly, the 2013 ASCO guidelines on FP have incorporated a variety of healthcare providers, including RNs, to their list of those capable of FP education (Loren et al., 2013). RNs have an important role within the oncology care team and are uniquely positioned to provide FP education and counseling (King et al., 2008). They generally have more consistent and prolonged contact with patients during their hospitalizations as compared to physicians (Douw et al., 2015; Romero-Brufau et al., 2019), and nursing has been rated the most trusted profession for the past 19 years (Reinhart, 2020). To successfully implement FP guidelines for AYAs with cancer, there is an urgent need to leverage the role of nurses. To the authors’ knowledge, little is known about the nurse’s role in FP for AYAs with cancer. Therefore, this integrative review sought to summarize and evaluate the existing quality of evidence on oncology nurses’ role in FP for AYAs and to provide recommendations to increase nurses’ involvement to improve AYA FP outcomes.
Methods
The authors conducted the literature search for this integrative review using methodology and analysis criteria relevant to nursing research (Whittemore & Knafl, 2005). To address the problem of identifying the role of nursing in AYA fertility preservation in cancer, a literature search was conducted. The initial database search was conducted in September 2019 and was updated in February 2021. A reference librarian was consulted prior to conducting the literature search to discuss search strategies and identify key terms relevant to the focus of integrating theory and research in nursing practice in AYA FP. A comprehensive search was completed using CINAHL®, PsycINFO®, PsycArticles®, Academic Search Ultimate, and MEDLINE®. Keywords included AYA, adolescent, young adult, YA, teen, cancer, oncology, neoplasm, tumor, tumour, malignancy, fertility, fertility preservation, onco-fertility, education, nurse, nursing, nurse practitioner, advanced practice registered nurse, NP, and APRN. The reference lists of all identified articles were also searched for relevant articles.
Literature Search
In the authors’ initial search, 85 articles were retrieved from the electronic search. Inclusion criteria were as follows: published in English; peer reviewed and published through April 14, 2020; contained key terms including AYA, cancer, and fertility preservation; and related to nursing practice. Exclusion criteria were as follows: systematic reviews or meta-analyses, gray literature, descriptive papers, abstract-only publications, and publicly available theses and dissertations (see Figure 1). 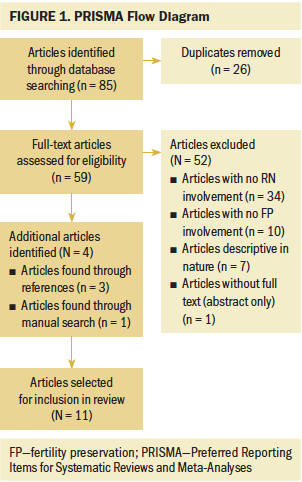
C.C. and L.A. reviewed all titles and abstracts, removing duplicates; thereafter, 59 articles were sent to D.R.A. and T.F.G. to review for inclusion. They identified 11 articles to be included in or excluded from the review. T.F.G. and D.R.A. then switched their article pool to ensure consistency of article inclusion or exclusion. In total, 11 articles met the inclusion criteria, including empirical (e.g., case studies, cross-sectional analyses) and theoretical reports. Most were excluded because they were descriptive in nature, were not specific to AYA FP, or had no review of nursing involvement. Data analysis was completed using the constant comparison method that recommends extracting data into systematic categories to facilitate distinct themes and relationships (Patton, 2002; Whittemore & Knafl, 2005).
Data extraction: To analyze and synthesize the evidence, data from the 11 primary sources were first ordered alphabetically (first author) and then categorized by research type (empirical or theoretical), study sample characteristics (e.g., nurses, physicians), and setting for data collection (e.g., single site, multiple sites) in a preliminary chart.
Data analysis: Data from sources were then indexed to include the study’s primary and secondary findings, recommendations, and key findings relevant to nursing involvement by C.C. and L.A., allowing the entire study team (C.C., L.A., T.F.G., and D.R.A.) to review extracted data thereafter. Through consensus, C.C. and L.A. further stratified the data by categories and themes. All authors reviewed the stratified data, compared findings, and synthesized data into subgroups of barriers and recommendations. Each identified theme was then coded per article, creating a total frequency for each theme (C.C. with team review). The team then compared frequencies and reduced data from this larger matrix to identify primary themes and abstracted findings. Methodologic quality was evaluated during each stage, specifically when coding relevance and frequency of the noted themes. As a final step, the study team synthesized conclusions and summarized interpretations, referencing the synthesized data chart and the larger thematic matrix concurrently. This integrative review did not require an institutional ethics review but was completed in compliance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist. All articles were critically appraised and met standards for methodologic quality.
Results
Synthesis of Literature Search
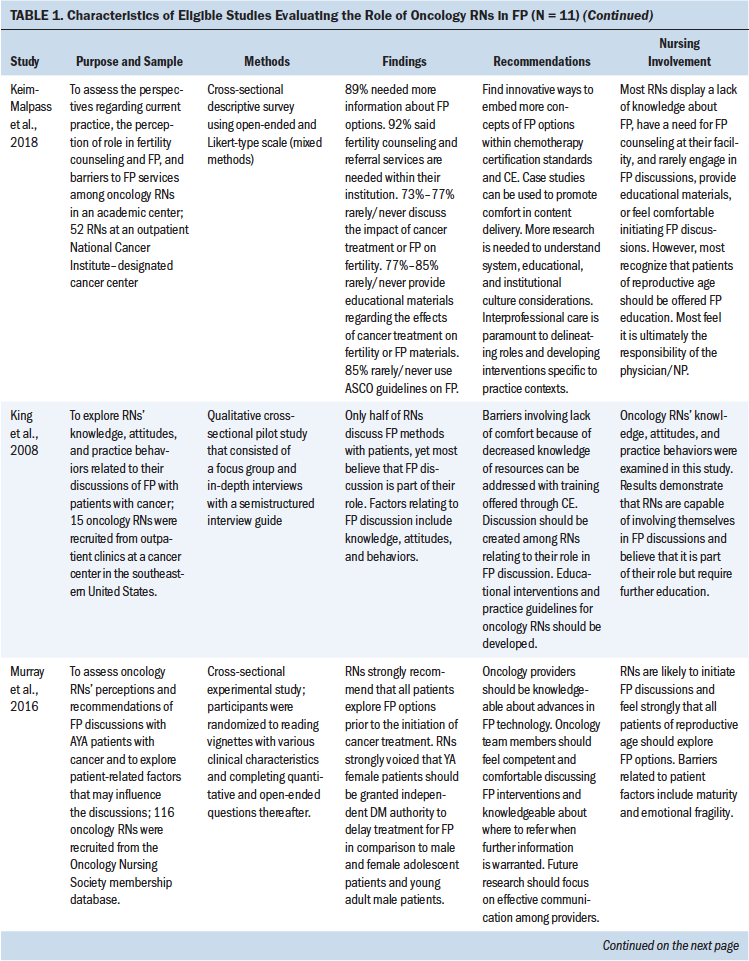
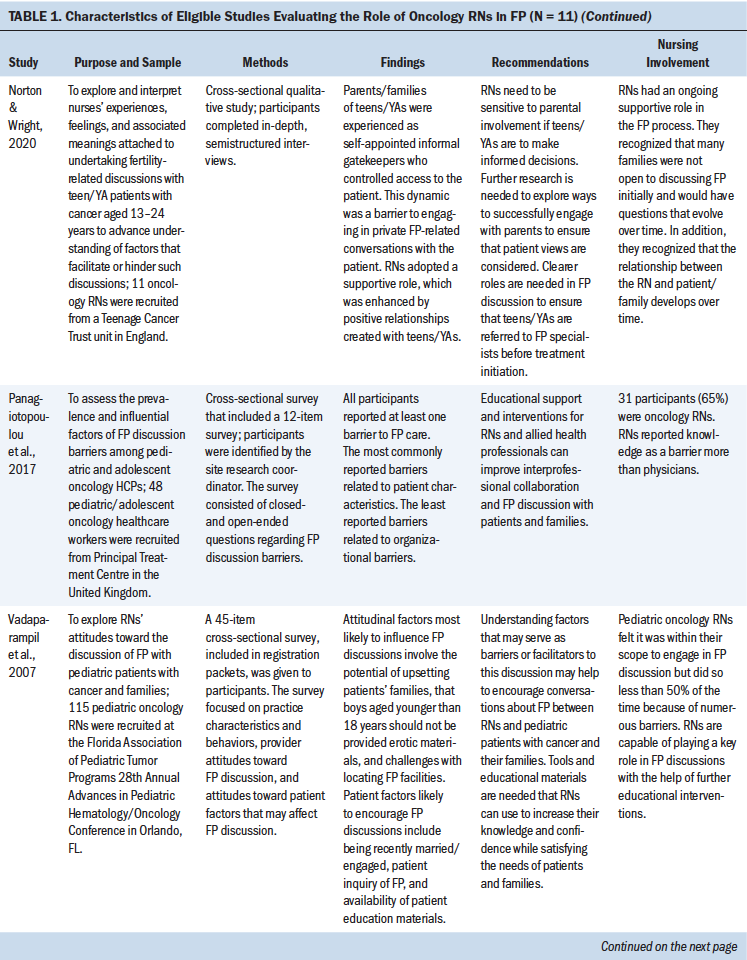
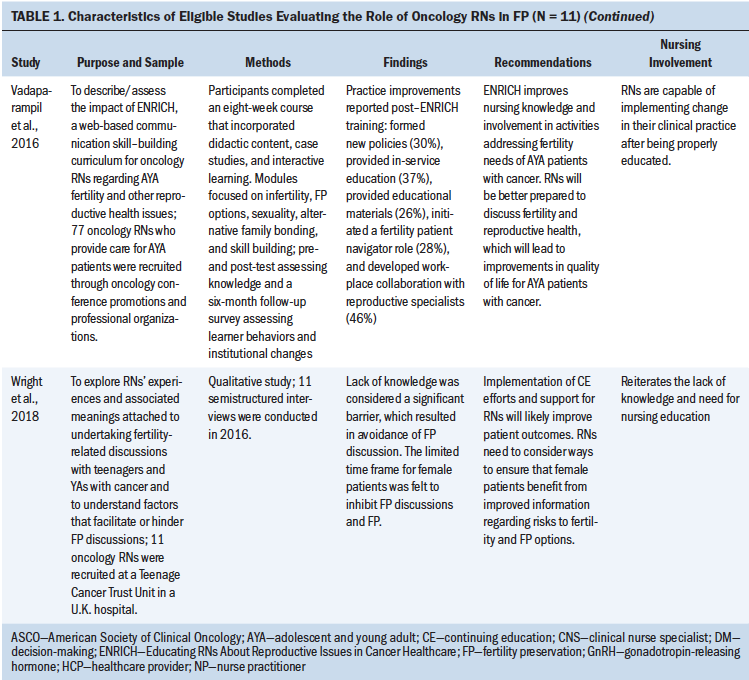
For initial analysis of research design type, a total of four articles used quantitative methods, four used qualitative methods, and three employed a mixed-methods design. Nine studies used cross-sectional surveys and interviews to evaluate perceptions of FP using quantitative (n = 4), qualitative (n = 4), or mixed-methods approaches (n = 1). Regarding sample characteristics, nine studies evaluated RNs only, and the remaining two studies included other types of healthcare providers in addition to RNs (Graham et al., 2017; Panagiotopoulou et al., 2017). Two studies included either an intervention or program implementation approach to evaluate nursing education for FP and evaluate nurse attitudes, perceptions, and levels of engagement with FP. All studies were published within the past 12 years. See Table 1 for study characteristics. 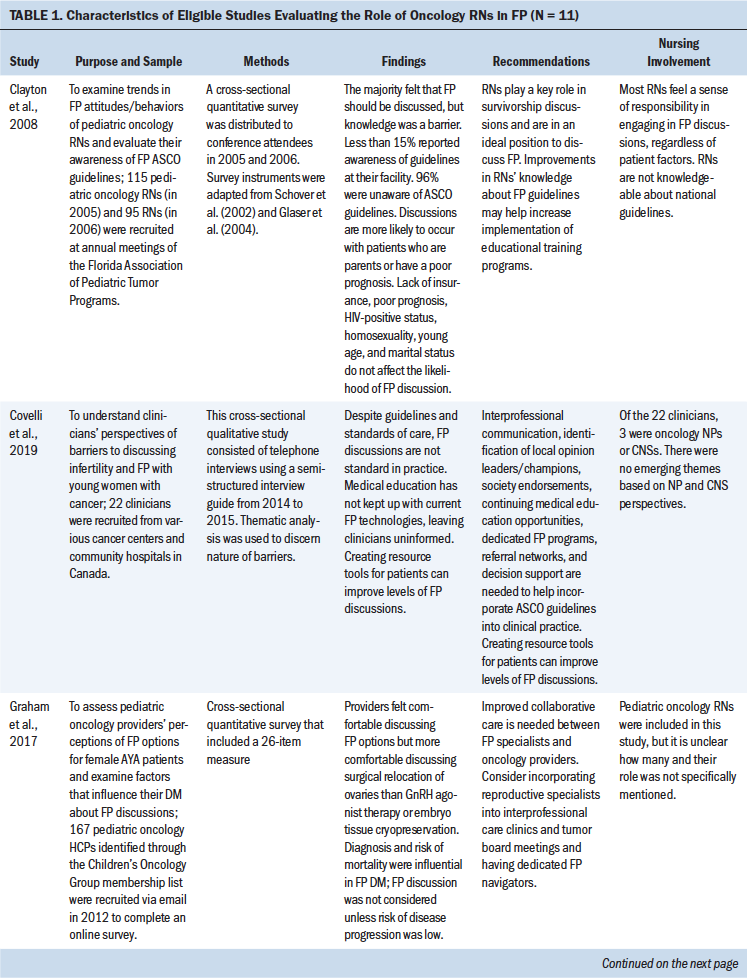
Data Evaluation
The studies relevant to this analysis were limited in quantity and consist of a diverse sample of cross-sectional self-report measures and qualitative analyses and one randomized trial; therefore, a direct comparison of study quality was not suited for this integrative review (Whittemore & Knafl, 2005). Current data are limited by largely observational, cross-sectional studies. Study samples were largely recruited from annual conference attendance and academic hospitals where research was conducted. Although both types of recruitment mechanisms show benefits related to examining nurses’ views about FP in large academic settings, such recruitment methods exclude the perceptions and experiences of RNs in community-based and rural settings. For instance, community nursing perspectives about FP, access to FP centers, and cultural factors for patients and RNs may vary significantly for these community-based and rural cohorts. The majority of the studies used survey-based research methods to assess clinician perspectives, which is highly subject to recall bias. The research could be significantly improved by evaluating electronic health records (EHRs) for evidence of nursing involvement in the FP trajectory of care. Longitudinal research is also needed to capture the effectiveness and optimal timing of FP interventions over time, to monitor changes in fertility concerns throughout the illness trajectory, and to evaluate intervention success throughout survivorship. Although a variety of providers are included in the studies to date, few integrate fertility specialists in their evaluations, which is a necessary disciplinary perspective to address FP needs of AYAs with cancer. With only one intervention study identified, further intervention research that leverages the role of nursing is needed in future work.
Data Synthesis
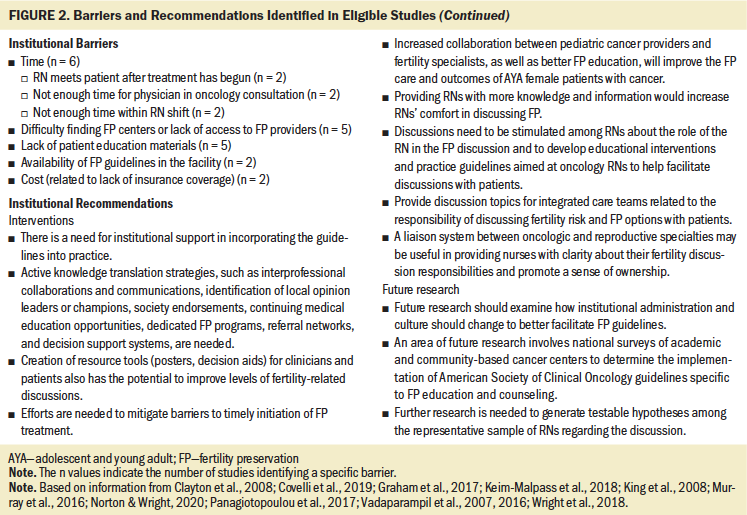
Extracted data were reviewed and indexed by barriers and success for FP nursing and non-nursing involvement, and by recommendations specific to increasing nursing involvement in FP. Relevant themes were categorized by clinician, patient, and systemwide barriers. The frequency of themes per study is noted in Figure 2. All themes were compared and analyzed to identify final barriers and recommendations. 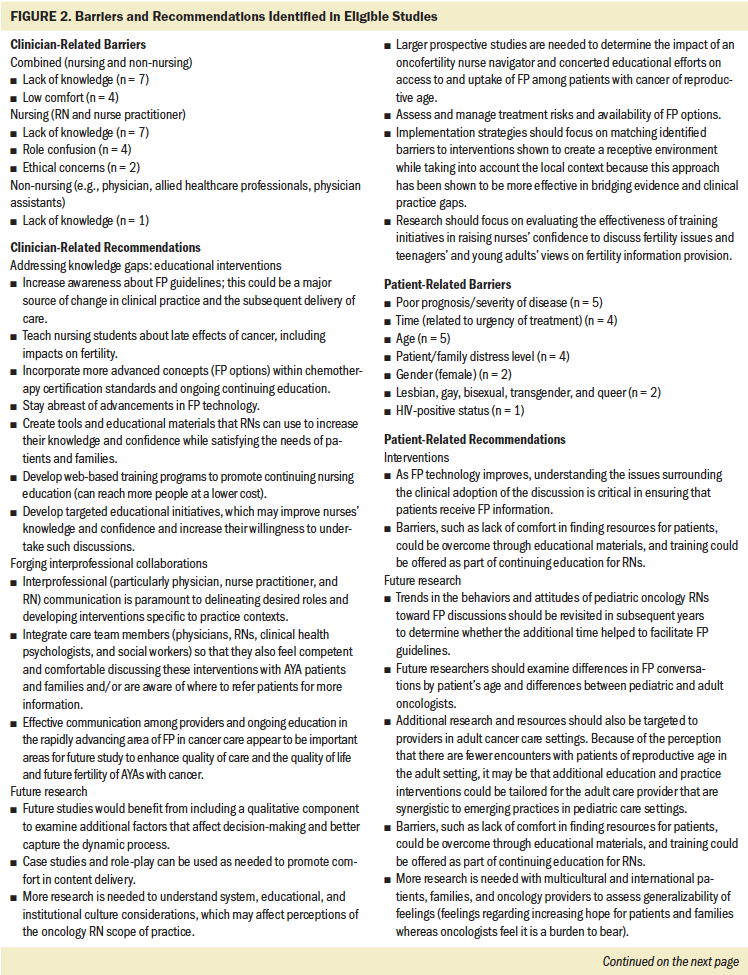
Barriers
Each study revealed several barriers that RNs face in addressing FP with AYAs with cancer. Primary themes included lack of knowledge, low comfort, role confusion, and ethical concerns. Patient-level barriers included patients’ poor prognosis, time limitations, age variability, distress level, gender, and lesbian, gay, bisexual, transgender, and queer (LGBTQ)/HIV factors. Institutional barriers included difficulty accessing FP center, lack of educational materials, and cost. The authors will discuss the role and involvement of each theme related to nursing involvement in FP stratified by clinician, systemwide, and patient factors.
Clinician-Related Barriers
Lack of knowledge regarding national guidelines and institutional policies among RNs and clinicians emerged as the most prominent barrier to FP (Clayton et al., 2008; Covelli et al., 2019, Keim-Malpass et al., 2018; King et al., 2008; Murray et al., 2016; Panagiotopoulou et al., 2017; Wright et al., 2018). Lack of knowledge largely correlated with the comfort level of RNs and was noted in studies by Keim-Malpass et al. (2018), King et al. (2008), Panagiotopoulou et al. (2017), and Wright et al. (2018). RNs emphasized that they would feel more comfortable engaging in FP discussions if they possessed more knowledge (King et al., 2008; Wright et al., 2018) and had clearer roles regarding FP (Keim-Malpass et al., 2018; King et al., 2008; Murray et al., 2016; Wright et al., 2018). In general, RNs reported that oncologists were primarily responsible for initiating FP discussions, but RNs expressed the desire to be involved in the FP process. RNs also endorsed feeling that they should follow up with patients after FP is introduced by the oncologist to ensure patients’ understanding, answer any follow-up questions, and provide access to resources and support (role confusion) (King et al., 2008). This role was exemplified by RNs in Norton and Wright’s (2020) study; however, RNs were not informed whether the patient/family received FP education at the initial physician consultation, causing further role confusion. The final provider barrier was related to ethical concerns of FP for adolescent patients. RNs identified ethical conflicts as a barrier to FP and reported unique concerns when parents of a child of reproductive age ask RNs to withhold FP information (Murray et al., 2016; Norton & Wright, 2020). RNs in Norton and Wright’s (2020) study noted that adolescents’ parents/family often occupy the role of self-appointed gatekeepers to the patient and, thereby, hinder FP conversations. RNs also expressed concerns regarding provision of pornographic material to male adolescent patients aged younger than 18 years (Vadaparampil et al., 2007). In addition, RNs reported concerns and barriers specific to the patient’s age, religiosity, cultural background, and sexual orientation. These findings highlight the unique challenges experienced by pediatric oncology RNs, more so than adult oncology RNs. In addition, four studies in the authors’ review did not specify whether the RNs worked in pediatric or adult settings.
Institutional Barriers
Institutional factors may also serve as barriers to RNs discussing FP with AYA patients with cancer. Time was noted as the most frequently reported institutional barrier (Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008; Panagiotopoulou et al., 2017). Specifically, limited time during busy RN shifts and lengthy clinician oncology consultations were identified as other time-related barriers. Timing, in the context of diagnosis and treatment, for nursing involvement in FP was also stressed as a barrier. For instance, RNs often care for patients with cancer after treatment has begun, which nullifies the opportunity to engage in FP discussions at critical moments of care prior to surgery, chemotherapy, or radiation therapy (Keim-Malpass et al., 2018; King et al., 2008). Their lack of access to patient educational materials also emerged as a significant barrier to providing FP care (Clayton et al., 2008; Covelli et al., 2019, Keim-Malpass et al., 2018; King et al., 2008; Vadaparampil et al., 2007). Lack of access to local fertility centers and knowledge of their location were highlighted as systemic barriers to connecting patients in four U.S. studies and one Canadian study (Clayton et al., 2008; Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008; Vadaparampil et al., 2007). Lastly, high costs associated with FP procedures were noted as an institutional barrier, which is evidence of potential disparities in care. A lack of insurance coverage was noted as a specific barrier in two studies (Covelli et al., 2019; King et al., 2008).
Patient-Related Barriers
Patient-related barriers also constrain RNs from engaging in FP conversations. A patient’s poor prognosis and severity of disease was the most common patient barrier to FP discussions and appeared in five studies (Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008; Panagiotopoulou et al., 2017; Vadaparampil et al., 2007). Timing within their diagnosis and treatment plan was also a factor, where the urgency of a patient’s treatment preceded FP dialogue and intervention (Covelli et al., 2019; Graham et al., 2017; Vadaparampil et al., 2007; Wright et al., 2018). For example, an RN interviewed in Keim-Malpass et al.’s (2018) study described a typical patient scenario with a diagnosis of acute myeloblastic leukemia, which requires immediate initiation of treatment, leaving no time for egg retrieval. Female gender appeared as a barrier in two studies. Nurses in Clayton et al.’s (2008) study reported that guidelines were more available for male patients, and respondents in Covelli et al.’s (2019) study noted that females face different challenges because FP costs associated with necessary female FP procedures are more expensive. Patient age or maturity level was underscored in four studies (Graham et al., 2017; King et al., 2008; Murray et al., 2016; Panagiotopoulou et al., 2017); however, the concept of age was vaguely introduced and younger or older age was not specified. Nurses described challenges in honoring patient autonomy in the presence of parental involvement. For example, in Murray et al. (2016) and Norton and Wright (2020), RNs described encounters where parents specifically requested that fertility not be discussed with the patient. RNs also expressed hesitancy in providing pornographic materials to males aged younger than 18 years (Vadaparampil et al., 2007). Patients’ distress levels were clarified (Covelli et al., 2019; Murray et al., 2016; Vadaparampil et al., 2007) where RNs expressed reluctance to discuss fertility risks because of fear of exacerbating negative emotions and heightening information overload. Of note, a patient’s sexual orientation—LGBTQ status and HIV-positive history—dissuaded RNs from FP discussions (Murray et al., 2016; Vadaparampil et al., 2007).
Facilitators
Despite a multitude of barriers, facilitators were also highlighted. RNs were more likely to engage in FP discussions with adequate access to resources and patient education materials (Vadaparampil et al., 2007). RN FP discussions were also more likely with patients who were married or engaged (Vadaparampil et al., 2007) or who had at least one child (Clayton et al., 2008). Two studies noted that RNs were more likely to discuss FP if the patient initiated the conversation (King et al., 2008; Vadaparampil et al., 2007).
Recommendations
Study recommendations focused on solutions to addressing knowledge gaps, forging interprofessional collaboration, and optimizing the full scope and breadth of the RN role in FP.
Addressing Knowledge Gaps
Recommendations to address RNs’ limited or lack of knowledge were discussed in eight studies (Clayton et al., 2008; Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008; Panagiotopoulou et al., 2017; Vadaparampil et al., 2007, 2016; Wright et al., 2018), with two studies testing interventions to improve RN knowledge gaps (Murray et al., 2016; Vadaparampil et al., 2016). Clayton et al. (2008) stressed the importance of improving RNs’ knowledge gaps regarding national guidelines, and, surprisingly, 96% of the participants were unaware of ASCO FP guidelines. However, Clayton et al. (2008) emphasized that the mere knowledge of guidelines is insufficient to ensure knowledge translation and FP engagement. As a result, Clayton et al. (2008) called upon cancer facilities to provide institutional support that may facilitate the integration of guidelines into clinical practice. Examples of institutional support include advocacy for interprofessional collaboration, identification of institutional and local leaders/champions, society endorsements, continuing education, dedicated FP programs, referral networks, and decision support systems (Clayton et al., 2008). To evaluate the efficacy of institutional education and implementation of FP guidelines, Keim-Malpass et al. (2018) recommended conducting national surveys among academic and community cancer centers to ensure FP engagement. However, national guidelines recommend standardized documentation of FP education, which is presently lacking in the majority of cancer care institutions.
Recommendations related to the use of continuing nursing education programs emerged in five studies (Clayton et al., 2008; Keim-Malpass et al., 2018; Vadaparampil et al., 2007, 2016; Wright et al., 2018). Wright et al. (2018) advised future researchers to evaluate the effectiveness of FP RN training initiatives to confirm their utility. These recommendations set the stage for Vadaparampil et al.’s (2016) ENRICH (Educating RNs About Reproductive Issues in Cancer Healthcare) study, which emphasized RNs’ ability to successfully incorporate FP into clinical practice after undergoing sufficient education.
Forging Interprofessional Collaborations
Improving interprofessional collaboration was highlighted in four studies (Graham et al., 2017; Keim-Malpass et al., 2018; Murray et al., 2016; Wright et al., 2018). For example, Keim-Malpass et al. (2018) and Murray et al. (2016) emphasized the need for targeted collaborations within the interprofessional oncology team, comprised of clinicians, RNs, and nurse practitioners. The studies by Graham et al. (2017) and Wright et al. (2018) emphasized the need for collaboration between FP specialists and the oncology team, such as a liaison system between the two teams that may help clarify RN responsibilities and promote ownership, which is an identified barrier to FP conversations.
Optimizing the Full Scope and Breadth of the RN Role
Although four studies concluded that RNs are ideally suited to discuss FP given their training, expertise, and the unique relationship with the patient (King et al., 2008; Murray et al., 2016; Norton & Wright, 2020; Vadaparampil et al., 2007), further research regarding the nursing role is warranted. King et al. (2008) emphasized the need to explore and clarify RNs’ role, stating that discussions need to take place within nursing groups to develop educational interventions and guidelines specifically for RNs. In addition, Keim-Malpass et al. (2018) encouraged the pursuit of further research to better understand the system, educational, and institutional cultural considerations that affect RN perceptions, as well as the need for larger prospective studies to determine the impact of an oncofertility nurse navigator.
Review of Findings
The majority of the studies in the current review found FP to be an essential aspect of oncologic care in AYAs and reported that patients of all reproductive ages should be offered information about FP prior to treatment. However, evidence suggests that nursing knowledge of FP clinical guidelines remains limited (Clayton et al., 2008; King et al., 2008; Wright et al., 2018). Clayton et al.’s (2008) study revealed that 96% of nurses were unaware of the ASCO guidelines. In addition, RNs are not engaging in FP discussions with their patients (Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008; Vadaparampil et al., 2007), with Keim-Malpass et al. (2018) noting that 77% of RNs rarely or never discuss FP with their patients. Although RNs recognize the importance of FP discussions, they also report a general lack of knowledge, resulting in decreased comfort levels and limited discussions. Of note, patients endorse feeling more comfortable discussing fertility concerns with RNs as opposed to clinicians (King et al., 2008). Therefore, efforts are needed to expand the role and scope of nursing with regard to FP by equipping RNs with the knowledge, confidence, and competence to initiate FP discussions with AYAs with cancer and their families.
Discussion
This integrative review summarized and evaluated the existing quality of evidence on oncology nurses’ role in FP for AYAs and provides recommendations to improve AYA FP outcomes. Study findings indicate that RNs have a minimal role in FP because of numerous provider, institutional, and patient-related barriers, even though they are well positioned to improve FP care in AYAs with cancer. Despite long-standing ASCO guidelines, research suggests that many providers do not disclose the risks or do so inadequately (Lee et al., 2006). Less than 60% of oncologists discuss fertility risk, and less than 40% of oncologists refer patients with fertility risk to reproductive specialists (Quinn et al., 2015). Although oncologists are incredibly skilled in treating disease and are capable of FP, they are often burdened by institutional barriers and may benefit from delegating FP tasks through a collaborative approach.
Implications for Practice
Oncology nurses must be integrated into AYA FP management as a way for healthcare systems to properly adhere to practice guidelines. This review underscores the importance of using interprofessional approaches to meet FP needs of AYA populations. Interventions to enhance nurses’ knowledge about FP, improve EHR documentation, and facilitate institutional support are needed to address barriers and support the nursing role in FP for AYAs with cancer.
Recommendations to Address Clinician-Related Barriers
Lack of knowledge, low comfort, ethical concerns, and role confusion were consistently identified as primary barriers to RN involvement in FP discussions with AYAs with cancer. Although lack of knowledge was the most prominent barrier, evidence shows that RNs are successful in knowledge translation through FP educational interventions. As an example, Vadaparampil et al.’s (2016) program implementation study found that after completing the ENRICH program, more than 70% of RNs met with providers to discuss reproductive health issues, nearly half reviewed practice guidelines, and many formed FP committees, created patient education materials, contributed to in-service education, and assisted in creating collaborative relationships with FP specialists. Educational interventions, such as ENRICH, can improve FP implementation and increase RN comfort level in engaging in FP discussions. Recognizing that no single group of healthcare professionals possesses all the knowledge and skills necessary to adequately address all FP issues (Barbour et al., 2013), there is an urgency for interprofessional approaches. Collaborations with fertility specialists, social work, psychology, palliative care, and chaplaincy are essential to mitigate ethical concerns and clinician barriers. In addition, oncology nursing organizations should be called upon to incorporate FP into certification courses and continuing education courses. FP education should also address parental preferences and patients’ age and maturity to ensure that RN interventions are patient-centered and age-appropriate.
Role confusion for RNs persists despite the inclusion of RNs in the 2013 ASCO FP guidelines. RNs state that clinicians and nurse practitioners are ultimately responsible (Keim-Malpass et al., 2018); however, the majority consider themselves to be capable of involvement in FP. RNs may benefit from specific guidelines from cancer institutions, oncology nursing organizations, and other professional healthcare organizations. RNs and advanced practice RNs (APRNs) occupy a variety of roles within the oncology setting, such as bedside RNs, RN navigators, clinical nurse specialists, and nurse practitioners, each of whom can address important barriers to FP for AYAs with cancer. An example of fully leveraging nursing in FP has been demonstrated at Princess Margaret Cancer Centre in Toronto, Ontario, Canada, which launched a successful AYA program where APRNs conduct consultations, identify FP needs and resources, and educate staff RNs to eliminate knowledge-related barriers (Hendershot et al., 2016). Although role confusion exists for RNs, increased role transparency, collegial support, and appropriate training could scaffold their role in FP.
Recommendations to Address Patient-Related Barriers
Patient-level barriers, including poor prognosis and severity of disease, time related to urgency of treatment, age, distress level, gender, sexuality, and HIV-positive history, continue to play a role in FP access and engagement. In exploring ways to improve FP for AYAs with cancer, evidence suggests that patients are more comfortable discussing challenging aspects of FP with RNs than physicians (King et al., 2008); therefore, RNs are in an ideal position to address patient barriers as they relate to FP. Meanwhile, patient factors, such as being married or engaged (Vadaparampil et al., 2007), having at least one child (Clayton et al., 2008), and initiating the FP conversation (King et al, 2008; Vadaparampil et al., 2007), seem to facilitate RN involvement in FP. In addition, lack of standardized documentation remains problematic in being able to assess whether FP education is actually occurring in patient encounters. Although documentation of FP education before treatment is often required, Quinn et al. (2015) noted that only 26% of providers documented discussions pertaining to infertility risk and 24% documented FP options, leaving a large population of individuals who are likely not receiving such discussions. King et al. (2008) suggested the development of an electronic notification to automatically remind healthcare professionals to discuss FP or generate referrals—a place RNs could scaffold FP-concordant care. EHR reviews provide an opportunity to assess ongoing documentation rates. Patient-related barriers to FP care should also be addressed when ideating solutions. Patient distress, a noted barrier to engaging in FP discussions (Covelli et al., 2019; Murray et al., 2016; Vadaparampil et al., 2007), can be addressed through psychological support that has been shown to reduce fertility-related distress (Skaczkowski et al., 2018) and, therefore, should be incorporated into patients’ plans of care.
Recommendations to Address Institutional Barriers
With regards to institutional barriers, time, access to FP centers/referrals and patient educational materials, availability of facility-based FP guidelines, and cost of FP emerged as the most common factors. Time remains a notable barrier to FP (Covelli et al., 2019; Keim-Malpass et al., 2018; King et al., 2008). New institutional and reimbursement structures are needed to allow discussions about fertility risks and options to be deemed billable and reimbursable. Insurance companies also need to improve coverage for cancer-induced FP to remove cost-related barriers for AYAs with cancer. Nurses should ideally be included in pretreatment discussions about FP, as well as be informed about and have the ability to initiate referral processes (Clayton et al., 2008; Covelli et al., 2019, Keim-Malpass et al., 2018). Collaborations with neighboring FP centers are particularly needed to streamline referrals.
Institutional support is needed to create facility-based guidelines and increase access to educational materials and financial resources for RNs who care for AYAs with cancer. Numerous national oncology organizations (e.g., Oncofertility Consortium, Livestrong Foundation) provide accessible national guideline–based decision support tools for providers and educational and financial resources for AYA patients. Examples of successful defined care models that address age, development, and gender-based considerations are outlined by Anazado, Ataman-Millhouse, et al. (2018), and those that address the interprofessional involvement in documentation and psychosocial support are outlined by Anazado, Laws, et al. (2018). Through institutional support, oncology RNs and APRNs can apply their dynamic roles to educate and refer patients to necessary resources. 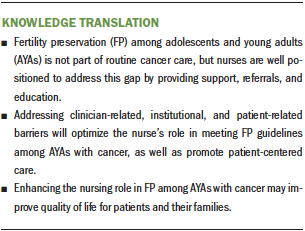
Conclusion
Although FP is an integral aspect of AYAs’ experience with cancer, to date, adherence to practice guidelines is low. The authors’ findings show that RNs pose a strong solution to providing guideline-concordant FP care; however, RNs have minimal involvement in FP because of numerous provider-, institutional-, and patient-specific barriers. Addressing these barriers will optimize nurses’ role in meeting FP guidelines among AYAs with cancer, as well as promote patient-centered care. 
About the Author(s)
Christina Crespi, MSN, APRN, FNP-C, CCRN, is a family nurse practitioner at Housecall Physicians LLC in Pembroke, MA; Lynsie Adams, MSN, APRN, FNP-C, OCN®, is a hematology-oncology nurse practitioner at Boston Medical Center in Massachusetts; Tamryn F. Gray, PhD, RN, MPH, is an instructor of medicine in the Department of Psychosocial Oncology and Palliative Care at the Dana-Farber Cancer Institute and Harvard Medical School, both in Boston, MA; and Desiree R. Azizoddin, PsyD, is a research scientist in the Department of Psychosocial Oncology and Palliative Care at the Dana-Farber Cancer Institute and Harvard Medical School and in the Department of Emergency Medicine at Brigham and Women’s Hospital, all in Boston, MA. No financial relationships to disclose. All authors contributed to the conceptualization, design, and manuscript preparation, completed the data collection, and provided statistical support and analysis. Crespi can be reached at christina.crespi@gmail.com, with copy to ONFEditor@ons.org. (Submitted November 2020. Accepted March 10, 2021.)

