Relations of Mindfulness and Illness Acceptance With Psychosocial Functioning in Patients With Metastatic Breast Cancer and Caregivers
Objectives: To examine relationships in mindfulness and illness acceptance and psychosocial functioning in patients with metastatic breast cancer and their family caregivers.
Sample & Setting: 33 dyads from an academic cancer center in the United States.
Methods & Variables: Participants completed questionnaires on mindfulness, illness acceptance, relationship quality, anxiety, and depressive symptoms. Dyadic, cross-sectional data were analyzed using actor–partner interdependence models.
Results: Greater nonjudging, acting with awareness, and illness acceptance among caregivers were associated with patients’ and caregivers’ perceptions of better relationship quality. Higher levels of these processes were associated with reduced anxiety and depressive symptoms in patients and caregivers.
Implications for Nursing: Aspects of mindfulness and illness acceptance in dyads confer benefits that are primarily intrapersonal in nature. Nurses may consider introducing mindfulness and acceptance-based interventions to patients and caregivers with adjustment difficulties.
Jump to a section
Breast cancer is the most common cancer diagnosis in women in the United States (Siegel et al., 2019), with more than 154,000 women estimated to be living with metastatic breast cancer (Mariotto et al., 2017). Although advances in medical therapies have improved the prognosis of metastatic breast cancer, the disease is typically incurable and is associated with high symptom burden (Kokkonen et al., 2017). Common symptoms in metastatic breast cancer include fatigue, sleep issues, pain, depression, and anxiety—all of which can interfere with activities of daily living and reduce quality of life (Dodd et al., 2010; Kokkonen et al., 2017).
According to interdependence theory, close family members interact in a relational system in which they influence each other’s well-being (Lewis et al., 2006). Therefore, psychological and relational outcomes are hypothesized to be interrelated within patient–caregiver dyads (Park & Schumacher, 2014). Consistent with this hypothesis, studies have found that mental health and relational outcomes of patients with cancer and their caregivers are often moderately correlated (Hagedoorn et al., 2008; Hodges et al., 2005; Jacobs et al., 2017; Kim et al., 2008; Northouse et al., 2012). In addition, the degree of similarity in distress between patients with cancer and spousal caregivers has predicted quality-of-life outcomes in caregivers, highlighting the importance of addressing mental health in families (Kim et al., 2008). Patients with cancer and their spousal caregivers who collectively engage in constructive cancer-related communication and supportive behaviors (i.e., behaviors that take into account the other person’s responses and emotions) report better relationship quality (Manne & Badr, 2008; Traa et al., 2015). On the other hand, dyads who engage in mutual avoidance and unsupportive behaviors, such as hiding concerns and dismissing worries, report worse relationship functioning, mental health, and quality of life (Badr et al., 2010; Drabe et al., 2013; Traa et al., 2015).
Although healthy communication patterns between patients with cancer and caregivers have been identified (Badr et al., 2010), other processes that may promote adaptive responses to cancer, such as mindfulness and illness acceptance, have rarely been studied from a dyadic perspective. Mindfulness refers to the capacity to approach present-moment experiences without getting caught up in judgment (Kabat-Zinn, 1994), whereas illness acceptance refers to a sense of peace in confronting mortality and losses associated with the illness (Mack et al., 2008). Lower levels of mindfulness and illness acceptance have been associated with worse mental health outcomes in patients with advanced cancer (Chambers et al., 2016; Thompson et al., 2009; Xu et al., 2017). Increased mindfulness may lead to greater illness acceptance, as mindfulness involves less reactivity toward unwanted thoughts and feelings. Growing evidence supports the efficacy of mindfulness-based training programs in reducing anxiety and depressive symptoms in patients with cancer and their caregivers (Birnie et al., 2010; Milbury et al., 2018; Zhang et al., 2019).
Theory suggests that mindfulness may be an interpersonal process, such that greater mindfulness in one partner may lead to improved perceptions of relationship quality in the other partner (Karremans et al., 2017). Mindfulness practices may lead to better relational outcomes by improving emotion regulation, including awareness of one’s reactions to stressful circumstances (Boyle et al., 2017; Roemer et al., 2015). This mindful awareness may foster better communication with close others, including open discussion of painful medical realities, resulting in support provision and better relationship quality. Studies suggest that mindfulness is associated with increased receptive attentiveness and empathic communication, both of which are related to greater relationship satisfaction (Barnes et al., 2007; Wachs & Cordova, 2007). Mindfulness has also been linked to better relationship quality through higher levels of partner acceptance and perceived responsiveness to their concerns (Adair et al., 2018; Kappen et al., 2018). Because mindfulness has predicted less negative emotional experience, it is possible that mindfulness might also predict fewer maladaptive expressions of emotions, including less verbal aggression and conflictual communication patterns associated with relationship dissatisfaction (Barnes et al., 2007; Brown & Ryan, 2003; Carrère & Gottman, 1999). Consistent with this notion, mindfulness-based interventions targeting maladaptive communication patterns in healthy romantic couples have led to improved relationship satisfaction (Carson et al., 2004). In addition, mindfulness training for patients with advanced cancer and their family caregivers improved caregiver perceptions of family communication (Johns et al., 2020). In qualitative interviews, patients and caregivers also reported that the intervention strengthened their relationship (Cottingham et al., 2019).
Among studies of dyads coping with chronic illness, only three have examined the influence of one partner’s mindfulness on the other partner’s psychosocial functioning (Pakenham & Samios, 2013; Schellekens et al., 2017; Williams & Cano, 2014). Two studies of couples coping with lung cancer and multiple sclerosis found that each person’s mindfulness was negatively associated with their own distress but was unrelated to their partner’s distress (Pakenham & Samios, 2013; Schellekens et al., 2017). The third study included couples coping with chronic pain and found that spouses’ mindfulness was positively associated with patients’ relationship satisfaction and perceived partner responsiveness, but the couple was not the unit of analysis (Williams & Cano, 2014).
The current study builds on this limited literature to examine mindfulness and illness acceptance as potential dyadic processes associated with psychosocial functioning in patients with metastatic breast cancer and caregivers. Of note, the current authors used a dyadic analytic approach that accounted for potential interdependence in predictors and outcomes between patients with metastatic breast cancer and their family caregivers. Therefore, the authors examined relationships between study variables for patients and caregivers individually and as a dyad. Based on interdependence theory (Lewis et al., 2006), the authors hypothesized that greater patient and caregiver mindfulness (i.e., nonjudging, nonreactivity, and acting with awareness) and illness acceptance would be associated with their own, as well as their partner’s, increased relationship quality and reduced anxiety and depressive symptoms.
Methods
Participants
Participants were recruited for a telephone-based intervention trial from March to November 2016. The present study is a secondary analysis of participants’ baseline data. Patients were eligible if they were diagnosed with stage IV breast cancer at least three weeks prior to enrollment; were receiving care at the Indiana University Melvin and Bren Simon Cancer Center in Indianapolis; and had at least one moderate to severe symptom, defined as t scores of 55 or greater on Patient-Reported Outcomes Measurement Information System (PROMIS) measures of fatigue, pain, sleep disturbance, depressive symptoms, or anxiety (Cella et al., 2010; Pilkonis et al., 2011). Patients were ineligible if they had a self-reported Eastern Cooperative Oncology Group (ECOG) (Sørensen et al., 1993) Performance Status score of greater than 2 (able to do little activity), showed severe cognitive impairment (three or more errors on a six-item cognitive function screener) (Callahan et al., 2002), or were receiving hospice care at the time of enrollment. Eligible, consenting patients had the option of identifying a family caregiver as a potential study participant. Caregivers were eligible if they provided substantial emotional and practical support to the patient and lived with the patient or had visited the patient at least twice a week for the past month. This eligibility criterion ensured that dyads had a shared psychosocial experience of cancer. In addition, patients and caregivers had to be aged 18 years or older and fluent in English. Given the focus on dyadic associations, patients without a consenting family caregiver were excluded from the analyses in this study.
Procedures
The parent trial design, methods, and intervention effects on patient outcomes have been published previously (Mosher et al., 2018). Following Indiana University Institutional Review Board approval, potentially eligible patients were identified via chart review and consultation with the attending oncologist. Approved patients were sent study invitation letters and consent forms. Research assistants then called patients to screen for eligibility and obtain informed consent. With the consenting patient’s permission, a family caregiver was sent a study invitation letter and consent form. Research assistants then called the caregiver to screen for eligibility and obtain informed consent. Patients and caregivers completed an individual baseline telephone assessment, and each received a $25 gift card for participating in this assessment. After baseline, only patients participated in the parent trial intervention. The current study focuses on the baseline (preintervention) assessment.
Measures
Patients’ medical information was collected via chart review, and patients’ self-reported ECOG Performance Status (Sørensen et al., 1993) was obtained during eligibility screening. Patients and caregivers completed a demographic questionnaire and self-report measures. For all measures, higher scores indicate greater levels of the symptoms or outcomes. All measures have evidence of reliability and validity and have been used with patients with cancer and family caregivers.
Mindfulness and illness acceptance processes: Mindfulness was assessed with the short form of the Five Facet Mindfulness Questionnaire (Bohlmeijer et al., 2011). The following three five-item subscales were administered:
• Nonjudging (e.g., “I make judgments about whether my thoughts are good or bad.”)
• Nonreactivity (e.g., “When I have distressing thoughts or images, I am able to just notice them without reacting.”)
• Acting with awareness (e.g., “I rush through activities without being really attentive to them.”)
Responses were rated on a five-point Likert-type scale from 0 (never or very rarely true) to 4 (very often or always true). These subscales were selected because of their relationships to symptom and mental health outcomes in previous studies of patients with cancer (Cash & Whittingham, 2010; Poulin et al., 2016).
Illness acceptance was assessed with the five-item peaceful acceptance of illness subscale of the Peace, Equanimity, and Acceptance in the Cancer Experience measure (e.g., “To what extent are you able to accept your/[patient’s name]’s diagnosis of cancer?”) (Mack et al., 2008). Responses were rated on a four-point Likert-type scale from 1 (not at all) to 4 (to a large extent).
Psychosocial functioning: Patients and caregivers evaluated their relationship quality, or perceived closeness and communication with the other person, using the four-item Relationship Quality Interview (e.g., “Generally, how well do you and [name of patient/caregiver] get along together?”) (Lawrence et al., 1998). Responses were rated on four-point Likert-type scales, such as from 1 (not at all well) to 4 (very well). Anxiety and depressive symptoms were assessed with the four-item PROMIS Anxiety and Depression measures (Pilkonis et al., 2011). Sample items include “I felt fearful” and “I felt depressed,” respectively. Responses for both scales were rated on a five-point Likert-type scale from 1 (never) to 5 (always).
Statistical Methods
First, descriptive statistics were computed, and bivariate associations between demographic and medical variables and study outcomes in patients and caregivers were examined to identify potential covariates. Next, dyadic data were analyzed using actor–partner interdependence models (APIMs) with multilevel modeling (Kenny et al., 2006). In APIMs, the unit of analysis is the patient–caregiver dyad, which allows the effects within and between dyads to be examined and takes into account the interdependence of data from dyad members. Dyad members (i.e., patients and caregivers) were considered distinguishable in these models. Each APIM model included a predictor (i.e., nonjudging, nonreactivity, acting with awareness, or illness acceptance) and a study outcome (i.e., relationship quality, anxiety, or depressive symptoms) for patients and caregivers. In this analysis, “actor effects” refer to the relations of a person’s characteristics (e.g., illness acceptance) to their own outcomes (e.g., depressive symptoms), and “partner effects” refer to the relations of a person’s characteristics to their partner’s outcomes.
Results
Sample Characteristics
Of the 158 patients with metastatic breast cancer who were mailed study invitation letters, 138 were reached via telephone. Fifty patients were eligible and consented, 38 were ineligible, and 50 declined to participate. Therefore, 64% of patients reached via telephone were screened for eligibility. Of the 41 caregivers approached, 36 consented, 4 declined to participate, and 1 could not be reached. Common reasons for patients and caregivers declining to participate included lack of interest and the study time commitment. Three patients and their caregivers withdrew prior to the baseline assessment; therefore, 33 patient–caregiver dyads completed this assessment. 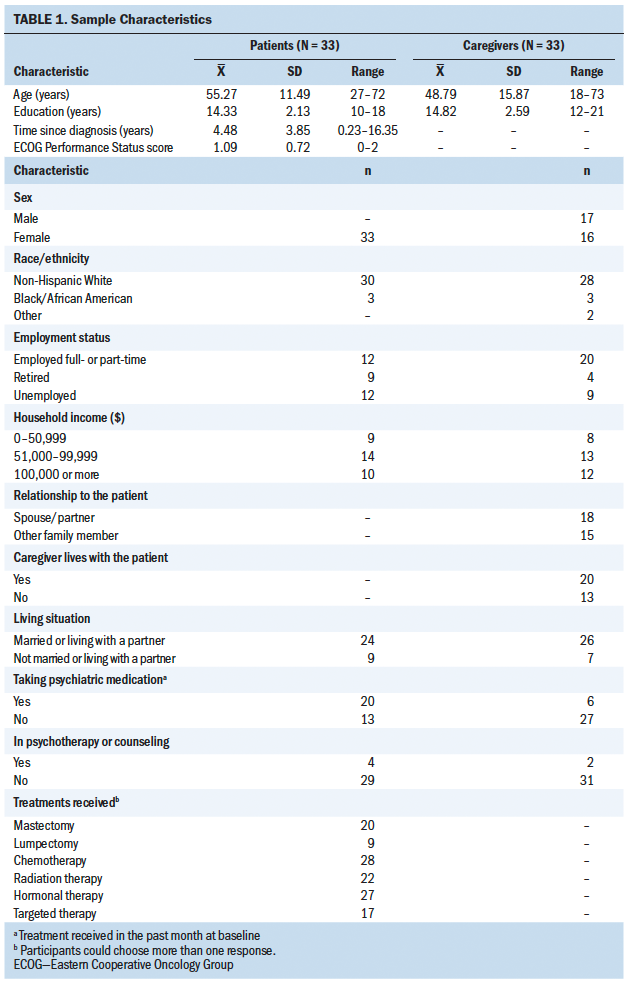
Table 1 presents sample characteristics. All patients were women, whereas about half of the caregivers were men and were spouses or partners of the patients. Most patients and caregivers were non-Hispanic White and had completed some post-secondary education. 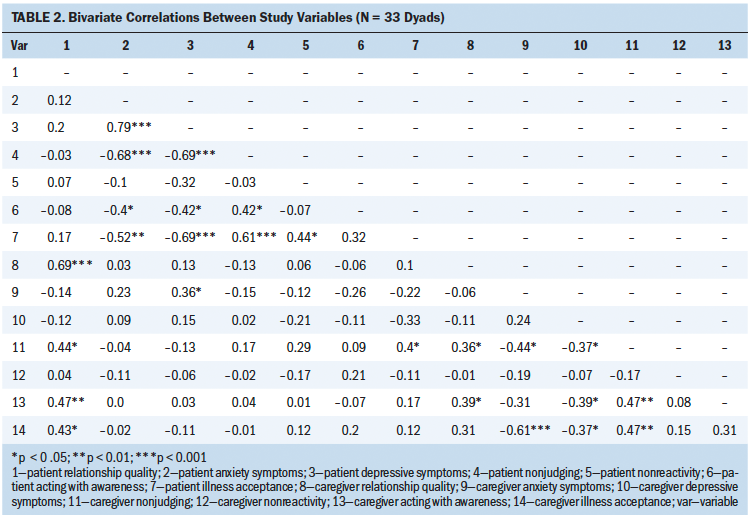
Preliminary Analyses
Descriptive statistics and bivariate correlations for main study variables are reported in Tables 2 and 3. Bivariate analyses indicated that for patients with cancer, older age was associated with lower depressive symptoms (r = –0.4, p = 0.022). Other demographic and medical factors were not significantly correlated with patient or caregiver relationship quality, anxiety, or depressive symptoms. 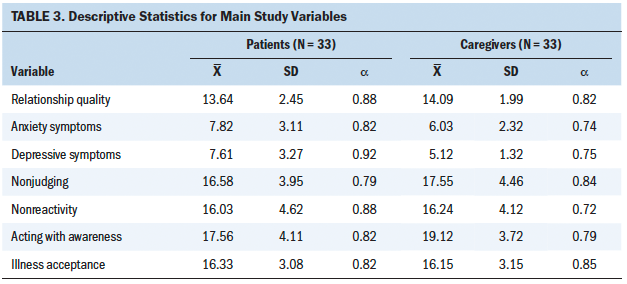
Dyadic Analyses
Using APIMs, the authors tested whether patient and caregiver mindfulness (i.e., nonjudging, nonreactivity, and acting with awareness) and illness acceptance were associated with their own, as well as their partner’s, relationship quality, anxiety, and depressive symptoms. Regarding relationship quality, the authors found significant actor and partner effects for caregivers but not for patients (see Figure 1). Specifically, caregivers’ levels of nonjudging and acting with awareness were positively associated with their own perception of their relationship quality (actor effects: beta = 0.4, p = 0.022 for nonjudging and beta = 0.39, p = 0.028 for acting with awareness), as well as patients’ perception of their relationship quality (partner effects: beta = 0.46, p = 0.007 for nonjudging and beta = 0.46, p = 0.007 for acting with awareness). The authors found a similar trend for illness acceptance, such that caregivers’ greater acceptance of the patients’ illness was associated with a marginal increase in their own perception of their relationship quality (beta = 0.3, p = 0.092) and a significant increase in patients’ perception of their relationship quality (beta = 0.41, p = 0.015). The authors found nonsignificant actor and partner effects for nonreactivity (beta = 0.00 to 0.08). 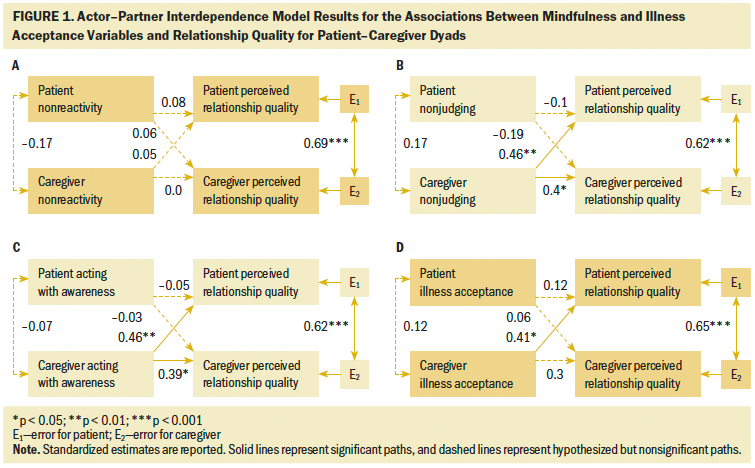
Regarding anxiety symptoms, the authors found significant actor but not partner effects (see Figure 2). Specifically, patients’ and caregivers’ levels of nonjudging and illness acceptance were negatively associated with their own anxiety symptoms (patient actor effects: beta = –0.69, p < 0.001 for nonjudging and beta = –0.53, p = 0.001 for illness acceptance; caregiver actor effects: beta = –0.42, p = 0.014 for nonjudging and beta = –0.59, p < 0.001 for illness acceptance), but were unrelated to their partner’s anxiety symptoms (beta = –0.14–0.07). For patients, greater acting with awareness was associated with a significant decrease in their own anxiety symptoms (beta = –0.4, p = 0.022) and a marginal decrease in their partner’s anxiety symptoms (beta = –0.29, p = 0.095). For caregivers, greater acting with awareness was associated with a marginal decrease in their own anxiety symptoms (beta = –0.34, p = 0.052) but not their partner’s anxiety symptoms (beta = –0.02, p = 0.891). The authors did not find significant actor and partner effects for nonreactivity (beta = –0.22 to –0.13). 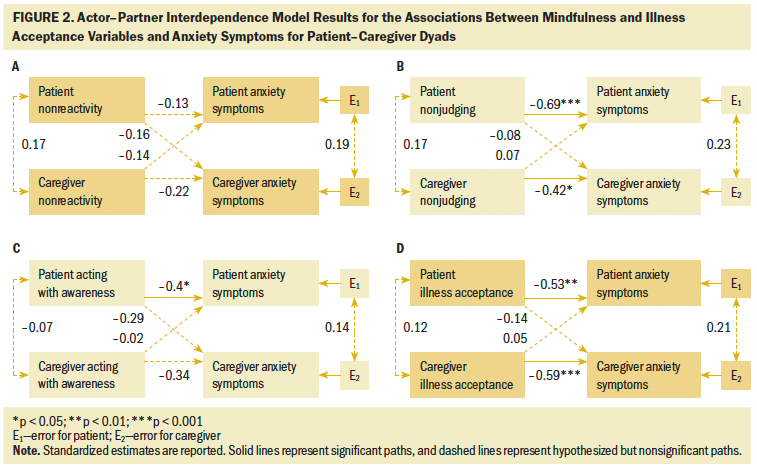
Depressive symptoms showed a similar pattern in that significant actor but not partner effects emerged (see Figure 3). For patients and caregivers, nonjudging, acting with awareness, and illness acceptance were associated with a decrease in their own depressive symptoms (patient actor effects: beta = –0.69, p < 0.001 for nonjudging, beta = –0.42, p = 0.016 for acting with awareness, and beta = –0.68, p < 0.001 for illness acceptance; caregiver actor effects: beta = –0.38, p = 0.029 for nonjudging, beta = –0.4, p = 0.021 for acting with awareness, and beta = –0.33, p = 0.047 for illness acceptance), but were not significantly related to their partner’s depressive symptoms (beta = –0.29 to 0.09). The authors also found that greater nonreactivity in patients was associated with a marginal decrease in their own depressive symptoms (beta = –0.34, p = 0.06), whereas other actor and partner effects for nonreactivity were small and nonsignificant (beta = –0.23 to –0.11). 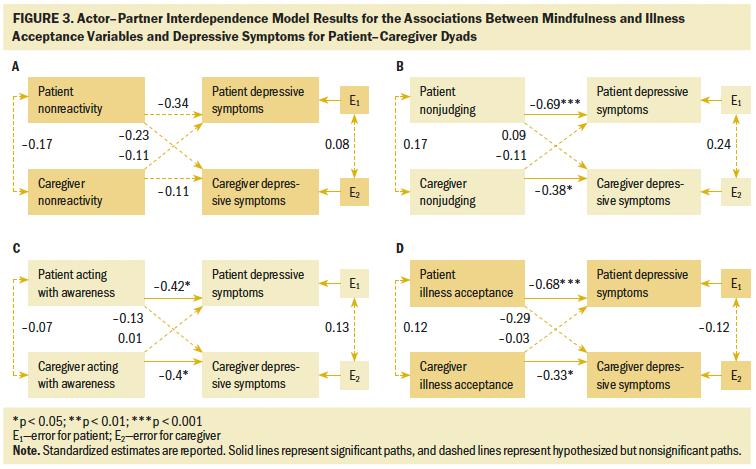
Discussion
This study examined mindfulness and illness acceptance processes in relation to psychosocial functioning in patient–caregiver dyads coping with metastatic breast cancer. Several findings should be highlighted. First, higher levels of two mindfulness facets (i.e., nonjudging and acting with awareness) and illness acceptance in caregivers were associated with more positive perceptions of relationship quality for both dyad members. However, these actor and partner effects on relationship quality were not found for patients. In addition, for patients and caregivers, greater nonjudging, acting with awareness, and illness acceptance were correlated with reduced anxiety and depressive symptoms. Contrary to hypotheses, no partner effects of mindfulness and illness acceptance processes were found for these symptoms. Taken together, results are largely inconsistent with interdependence theory, which postulates that close family members influence one another’s psychosocial outcomes (Lewis et al., 2006).
Caregivers’ greater mindfulness and illness acceptance did, however, relate to patients’ and caregivers’ perceptions of better relationship quality, which involves closeness and open communication within the dyad. These partner effects may be related to the gender composition of the sample—all patients were female, and about half of caregivers were male. Past research has found that women are more sensitive than men to emotional cues in relationships (Kiecolt-Glaser & Newton, 2001); therefore, patients in the current study may have been more aware of the other person’s emotional states (e.g., degree of self-judgment, peaceful acceptance of the illness) when rating relationship quality as compared to caregivers.
Actor and partner effects of caregiver mindfulness and illness acceptance on relationship quality may also be attributed to the caregiving role. Societal expectations differ for caregivers and patients, with caregivers expected to be emotionally resilient and strong for the patient. Caregivers endorsing higher levels of acting with awareness, for example, may perceive themselves as better caregivers, because they are keenly focused on their responsibilities. Positive self-perceptions of their competence as a caregiver might, in turn, drive their perceptions of relationship quality. Role expectations may also influence patient ratings of their relationship quality in that patients may focus on their caregiver’s ability to show emotional strength. Caregiving theory suggests that patients and their family caregivers engage in an evolving negotiation regarding the rules and expectations of their new relationship (Coeling et al., 2003). Therefore, caregivers who respond mindfully to the needs and requests of patients and maintain open communication about roles are likely to foster better relationships with them. Consistent with this notion, prior research has linked greater mindfulness to better perceived relationship quality; however, most of these studies were conducted with healthy couples, and analyses were non-dyadic (Kozlowski, 2013).
Nonjudging, acting with awareness, and illness acceptance were associated with patients’ and caregivers’ own mental health. Findings converge with previous research linking mindfulness and illness acceptance to better mental health in patients with cancer and caregivers (Birnie et al., 2010; Tang et al., 2016; Zhang et al., 2019). Mindfulness may lead to better mental health by improving emotion-regulation skills, such as the ability to manage and respond to difficult feelings (Roemer et al., 2015). Mindfulness and illness acceptance have also been related to more self-compassion, the ability to be kind to oneself in the face of personal suffering, which may lead to improved mental health (Boyle et al., 2017; Sirois et al., 2015).
The authors did not find partner effects of mindfulness or illness acceptance on mental health. The lack of partner effects of mindfulness is consistent with the small amount of literature on couples coping with lung cancer and multiple sclerosis (Pakenham & Samios, 2013; Schellekens et al., 2017). Judgment of oneself may not necessarily translate to judgment of one’s partner; therefore, lower levels of patient or caregiver mindfulness may have little effect on their partner’s mental health. It is also possible that reaching a state of acceptance of the diagnosis is a cognitive and emotional process that is not readily observed by others and, therefore, has limited effect on their well-being. Conversely, acceptance may be facilitated by cognitive and emotional processing of the illness with close others. In this study, although all caregivers were actively involved in the patient’s care, about 40% of dyads were not cohabitating, which may have affected the degree of communication about the illness. To date, illness acceptance has not been examined as a dyadic process and warrants further study in cancer dyads.
One aspect of mindfulness, nonreactivity, showed minimal effects on psychosocial functioning. Nonreactivity has been associated with mental health in other cancer samples, including patients with metastatic breast cancer and cancer survivors with chronic neuropathic pain (Poulin et al., 2016; Zimmaro et al., 2020). In the current sample of patients and caregivers, mean levels of nonreactivity were close to the scale midpoint and showed adequate variance. However, anxiety and depressive symptoms were in the mild to moderate range, which may have attenuated their relationships with nonreactivity. In addition, responding to items on nonreactivity requires skillful introspection, and samples with greater psychotherapy or mindfulness experience might have responded more accurately to nonreactivity items, increasing their associations with mental health outcomes.
Limitations
Limitations of this study include the cross-sectional analysis of baseline data from an intervention study, which does not allow for conclusions about the directionality of the findings. The sole reliance on self-report measures is another limitation; behavioral measures of mindfulness and relationship quality may be a useful supplement to self-report data in future research. In addition, the sample was primarily White and college-educated, and the relatively small sample size limited statistical power. However, because this was a pilot study, the authors focused on effect sizes to inform future research on mindfulness and acceptance processes with this understudied population. The authors did not have sufficient sample sizes to analyze the data by relationship type. Finally, the sample may differ from participants in other studies because they were recruited for an intervention study with a symptom criterion for patient eligibility. However, patients’ anxiety and depressive symptoms were similar to the levels reported by a representative sample of patients with metastatic breast cancer in the United States (Jensen et al., 2017).
Implications for Nursing
Nurses can screen patients with metastatic breast cancer and caregivers for anxiety and depression and recommend or deliver mental health services, including mindfulness-based interventions, to distressed individuals. Specific recommendations may include mindfulness-based stress reduction or mindfulness-based cognitive therapy. For patients and family caregivers who struggle with illness acceptance, nurses may also recommend acceptance and commitment therapy. The current findings in combination with the larger mindfulness literature in cancer (Schell et al., 2019; Zhang et al., 2019) suggest that nurse-led teaching of mindfulness skills to patients and caregivers may lead to better mental health and improved perceptions of their relationships. Mindfulness teaching may emphasize having a nonjudgmental, compassionate attitude toward thoughts and feelings and engaging in activities with full awareness. Trained nurses can teach specific mindfulness techniques, such as awareness-of-breath meditation, in outpatient and inpatient settings because they can be short in length and do not require equipment or materials. In addition, nurses may assist patients and caregivers in locating resources for formal mindfulness practice (e.g., mindfulness teacher, mental health therapist, guided meditations available on the Internet) and promote continued practice while assessing effects on psychosocial outcomes. 
Conclusion
The current findings contribute to a small body of research suggesting that the benefits of mindfulness and illness acceptance processes are more intrapersonal than interpersonal in nature (Pakenham & Samios, 2013; Schellekens et al., 2017). Results warrant replication in a larger, more diverse sample with various types of relationships represented (e.g., spouses/partners, parents, children, siblings). Next steps also include examining processes that may underlie the effects of mindfulness and illness acceptance on perceived relationship quality, such as improved empathy and reduced maladaptive expressions of emotions. Although a growing body of research has tested mindfulness-based interventions for patients with cancer and caregivers (Birnie et al., 2010; Johns et al., 2020; Milbury et al., 2018), few studies have adapted these interventions to an advanced cancer context. Developing efficacious interventions to meet the psychosocial needs of the growing population of patients with metastatic breast cancer and caregivers is an important goal for future research and clinical care in nursing and affiliated disciplines.
The authors gratefully acknowledge Susan Daily, BS, RT(T), and Danielle B. Tometich, MS, for their assistance with data collection in this study and the study participants for their time and effort.
About the Author(s)
Kelly Chinh, MS, and Ekin Secinti, MS, are both doctoral candidates in the Department of Psychology at Indiana University–Purdue University Indianapolis; Shelley A. Johns, PsyD, HSPP, ABPP, is an assistant professor of medicine in the Department of Medicine in the School of Medicine at Indiana University in Indianapolis; Adam T. Hirsh, PhD, is an associate professor of psychology in the Department of Psychology at Indiana University–Purdue University Indianapolis; Kathy D. Miller, MD, is the Ballve-Lantero Professor, Bryan Schneider, MD, is a professor of medicine and medical/molecular genetics, and Anna Maria Storniolo, MD, is the Andrew and Peggy Thompson Professor of Hematology/Oncology, all in the Department of Medicine in the School of Medicine at Indiana University and in the Indiana University Melvin and Bren Simon Cancer Center in Indianapolis; Lida Mina, MD, is the associate director of the breast program at the Banner MD Anderson Cancer Center in Gilbert, AZ; Erin V. Newton, MD, is a physician of medical oncology and palliative care in the Department of Medicine in the School of Medicine at Indiana University and in the Indiana University Melvin and Bren Simon Cancer Center; Victoria L. Champion, PhD, RN, FAAN, is a distinguished professor in the School of Nursing at Indiana University; and Catherine E. Mosher, PhD, is an associate professor in the Department of Psychology at Indiana University–Purdue University Indianapolis. This study was supported by a grant from the Walther Cancer Foundation. Champion and Mosher were supported by the National Cancer Institute (K05CA175048). Johns was supported by the National Cancer Institute (K05CA175048) and Walther Cancer Foundation (0175.01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or Walther Cancer Foundation. Chinh, Johns, Hirsh, Champion, and Mosher contributed to the conceptualization and design. Chinh, Miller, Storniolo, Mina, Newton, and Champion completed the data collection. Chinh, Secinti, Champion, and Mosher provided statistical support. Chinh, Secinti, and Champion provided analysis. Chinh, Secinti, Johns, Hirsh, Miller, Schneider, Storniolo, Newton, Champion, and Mosher contributed to the manuscript preparation. Chinh can be reached at kchinh@iupui.edu, with copy to ONFEditor@ons.org. (Submitted December 2020. Accepted April 29, 2020.)




