Breast Cancer Survivors’ Unmet Needs After Completion of Radiation Therapy Treatment
Purpose: To identify the unmet needs of breast cancer survivors after radiation therapy.
Participants & Setting: Patients who received radiation therapy for unilateral breast cancer with six months or longer of follow-up and exhibited no disease progression were eligible for selection to a study conducted at an outpatient radiation therapy academic practice in the southeastern United States.
Methodologic Approach: A qualitative descriptive study was undertaken using semistructured interviews, framed by the five domains of the Survivor Unmet Needs Survey and analyzed using an iterative inductive and deductive process.
Findings: Of the 24 invited patients, 17 agreed to the interview (including one male patient). Themes emerged from the emotional, relationships, and information needs domains: (a) the struggle with adapting to body image changes; (b) living with the fear of recurrence; (c) the unexpected impact of radiation dermatitis; and (d) the need for education to prepare for radiation therapy.
Implications for Nursing: Healthcare providers should perform a comprehensive needs assessment for patients with breast cancer receiving radiation therapy. Self-management assessment instruments may address patients’ confidence in managing all phases of radiation therapy side effects.
Jump to a section
Approximately 16.9 million people in the United States are considered cancer survivors, of whom about 67% have lived five years or more after initial diagnosis and 18% have lived 20 years or longer (American Cancer Society [ACS], 2020). The number of cancer survivors treated with radiation therapy is expected to reach 3.38 million in 2020 (Bryant et al., 2017). Breast cancer is among the most frequently diagnosed cancers in the United States. An estimated 320,000 individuals will be diagnosed in 2020, and approximately 40% will receive radiation therapy treatment (ACS, 2020; Bryant et al., 2017). The Institute of Medicine (IOM) report From Cancer Patient to Cancer Survivor: Lost in Transition identified the failure of the U.S. healthcare system to manage cancer survivors’ needs beyond five years (Hewitt et al., 2005). The report recommends that healthcare workers provide continuous, lifelong care for cancer survivors, as well as anticipate survivors’ needs (Hewitt et al., 2005). As cancer is more commonly being recognized as a chronic disease, as opposed to an acute diagnosis, continuity of care is vital to long-term surveillance of treatment-related side effects and early detection of secondary malignancies (National Academies of Science, Engineering, and Medicine, 2018).
Cancer Survivorship
The definition of a cancer survivor has evolved since the IOM report and is now defined as an individual from the time of cancer diagnosis throughout the balance of his or her life, including family members caring for the individual (Nekhlyudov et al., 2017). One way to address providing continuity of care for patients along the cancer trajectory was the recommendation from the IOM to develop a survivorship care plan (SCP) to facilitate evidence-based surveillance guidelines and assessment tools for the management of treatment-related side effects (Hewitt et al., 2005). However, SCPs may not sufficiently address the physical, psychosocial, and financial needs and concerns of the patient after treatment concludes.
Radiation Therapy for Breast Cancer
Radiation therapy treatment for breast cancer is recommended as part of an interprofessional approach, and it most often occurs after surgery and systemic therapy. The most common side effects include skin-related changes in the treatment field (e.g., radiation dermatitis), fatigue, and psychosocial concerns such as fear of recurrence (Halkett et al., 2009, 2012; Hess & Chen, 2014; Kole et al., 2017). The completion of radiation therapy treatment for patients with breast cancer often signifies the end of active treatment and the transition to lifelong survivorship care. Many SCP templates currently available focus on systemic therapy and provide helpful information for use within a medical oncology practice, but not within a radiation oncology practice (Koontz et al., 2016). In 2014, the American Society of Radiation Oncology surveyed member physicians to identify barriers to survivorship care because radiation oncologists typically provide long-term follow-up care for patients treated with curative intent. The study described barriers to survivorship care, including lack of information concerning radiation therapy side effects in SCP templates, cost associated with creating a radiation therapy–specific SCP, and lack of uniformity in SCP design (Chen et al., 2016; Frick et al., 2018; Koontz et al., 2016).
Existing SCPs do not adequately address long-term management of potential late side effects related to radiation therapy, including secondary malignancies, radiation pneumonitis, fibrosis, cardiotoxicity, and brachial plexopathy (Cogswell et al., 2018). The transfer of treatment information and symptom management varies and is dependent on each institution because of the lack of a comprehensive and standardized SCP. To adequately care for patients throughout the survivorship continuum, it is important to identify areas for improvement. Studies have found high rates of anxiety in patients with breast cancer prior to receiving radiation therapy; however, relatively little is known about the perceptions and unmet needs of patients with breast cancer after completion of radiation therapy (Halkett et al., 2008; Hess & Chen, 2014). Therefore, a better understanding of the specific needs experienced by patients with breast cancer is required as they transition into the survivorship phase.
Survivor Unmet Needs Survey
The Survivor Unmet Needs Survey (SUNS) is a validated instrument developed with a sample of 550 English-speaking Canadian adult cancer survivors and additionally tested for validity with 715 hematologic cancer survivors from Australia (Campbell et al., 2010; Hall et al., 2014). The survey asks respondents to measure unmet needs experienced during the past month and consists of 89 unmet needs items included within the following five domains: emotional health, access and continuity of care, relationships, financial concerns, and information needs (Campbell et al., 2010; Hall et al., 2014). A literature search did not reveal any published studies using SUNS to address unmet needs specifically related to breast cancer survivors after receiving radiation therapy. Therefore, the five overarching domains were used as a framework to inform the grand tour questions for interviews.
The primary aim of this study was to understand the unmet needs of patients treated with radiation therapy for breast cancer using the five domains of the SUNS instrument as a framework (Hall et al., 2014; Campbell et al., 2010). The secondary aim was to evaluate for any area of concern not included in the SUNS categories for survivors of breast cancer after completion of radiation therapy.
Methods
Study Design
This study employed a qualitative descriptive design using the five domains from the SUNS instrument as a framework to inform the open-ended questions asked to participants. SUNS is a validated instrument designed to determine the unmet needs of adult cancer survivors (aged 18 years or older) inclusive of many cancer types and has been previously used in breast cancer research (Campbell et al., 2010; Hall et al., 2014). Data show high internal consistency (overall Cronbach alpha = 0.99; range = 0.983 for emotional health to 0.932 for information needs), high acceptability (greater than 85% ease of use and comprehension), item test-retest reliability, and excellent content and construct validity (Campbell et al., 2010). An iterative process was used for data collection and analysis to develop themes from transcribed interviews regarding patient experiences after radiation therapy for breast cancer (Strauss & Corbin, 1990).
Sample
Patients in this study were recruited from an outpatient academic radiation oncology practice. A purposeful sampling method was used to identify potential participants. A list of patients with breast cancer previously treated with radiation therapy was sorted according to the following times from last treatment: 1 year (SD = 6 months), 4 years (SD = 12 months), and 8 years (SD = 24 months). All patients with breast cancer who met the above time frame criterion were included. Exclusion criteria included those who had experienced a metastatic or breast cancer recurrence, those who had not been seen in the clinic within the past two years, and non–English-speaking patients. Male and female patients aged 18 years or older were included, and the sample consisted of a mix of socioeconomic level (as determined by insurance), race, type of surgical procedure (lumpectomy versus mastectomy), and menopause status.
Procedure
The institutional review boards at the Medical University of South Carolina (MUSC) and the University of Florida, Jacksonville, approved the study. Each participant was assigned an alpha numeric code for anonymity. The principal investigator (M.P.) contacted potential participants who met the inclusion criteria via telephone and asked for their participation in the study. Interested candidates were then offered a date and time for an interview. Prior to each interview, the principal investigator explained the purpose of the study and obtained written informed consent.
Data Collection
Demographic data were collected through chart review and included age, gender, race or ethnicity, time since last radiation therapy treatment, type of radiation therapy received (proton, conventional, or both), type of surgery, menopause status, history of systemic therapy for breast cancer, and type of insurance. Individual face-to-face audio-recorded interviews were conducted in June and July 2018. Semistructured questions were guided by the five domains of SUNS: emotional health, access and continuity of care, relationships, financial concerns, and information needs (see Figure 1). Using a grounded theory framework, data collection and analysis were iterative and involved comparing interview to interview, refining questions, and developing themes (Strauss & Corbin, 1990). The number of participants included in a qualitative study depends on whether new themes emerge with increasing participation (Strauss & Corbin, 1990). Additional interview questions were added for clarification, as needed. The length of each interview was dependent on the amount of data shared. 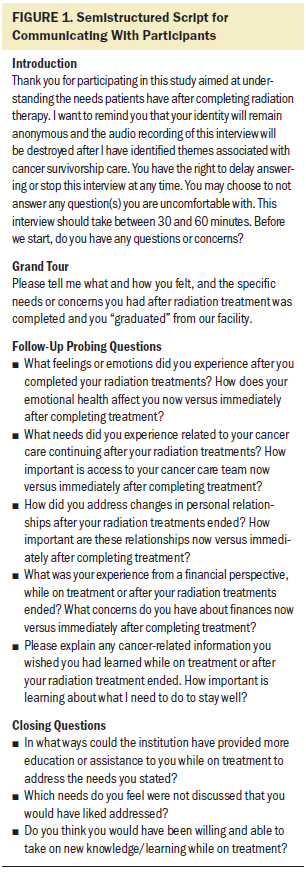
Data Analysis
Audio files collected from the interviews were electronically uploaded for professional transcription. Each transcription was then uploaded to NVivo, version 12.0 Pro, and the principal investigator conducted line-by-line coding to identify keywords and condensed phrases, assigning each word or phrase a subcategory. This analysis resulted in 35 categories, which were then reviewed by all authors and associated into one of the five larger categories of the SUNS domains for development of themes.
A senior qualitative mentor reviewed interview transcripts and guided the initial coding of data with the principal investigator to develop a consensus on themes, data saturation, and theory development. All authors reviewed interview transcripts and assisted with the categorization of subcategories and common themes. Data recording was conducted after a complete re-review of each transcribed interview.
Results
This study was open to as many as 25 participants; however, no new themes emerged, and data saturation was achieved after 17 participant interviews.
Demographic Data
Seventeen of 24 patients invited to participate enrolled in the study and were interviewed. Most participants were female (n = 16), postmenopausal (n = 13), aged older than 50 years (n = 14), and elected breast-conserving surgery/lumpectomy (n = 11). The median length of time from last radiation therapy treatment was 42 months (range = 7–136 months) (see Table 1). 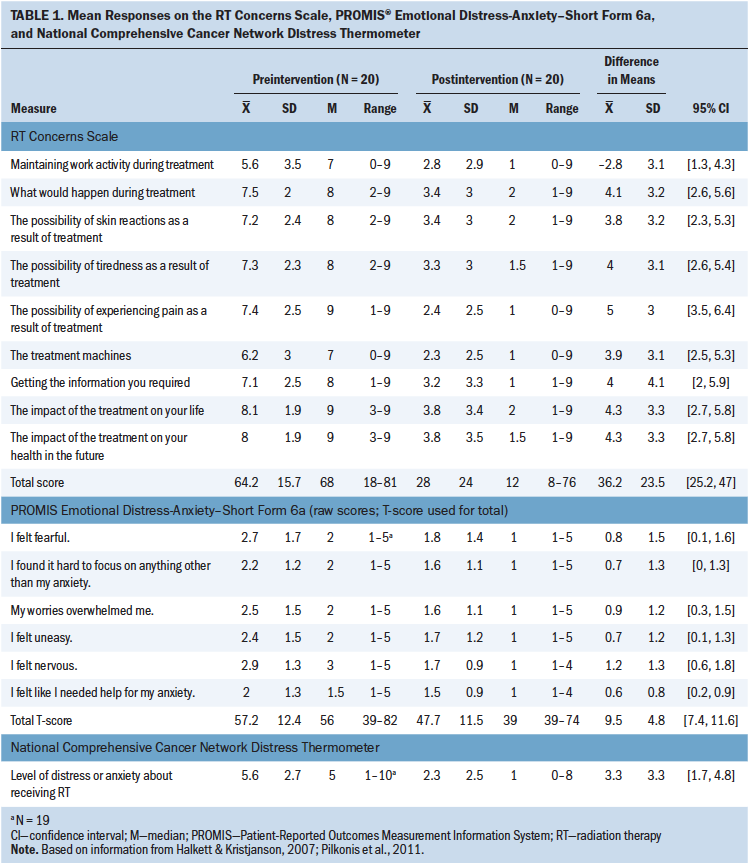
Emerging Themes
Data from three categories of the SUNS instrument reported the highest frequency of unmet needs concerning emotional health, information needs, and relationships. Financial concerns were reported by two participants, and unmet needs regarding access and continuity of care were reported by four participants. Table 2 summarizes the frequency with which the five main domains of the SUNS instrument and their associated subcategories emerged as prominent themes. The question(s) for each of the five domains begins each of the following category summaries. 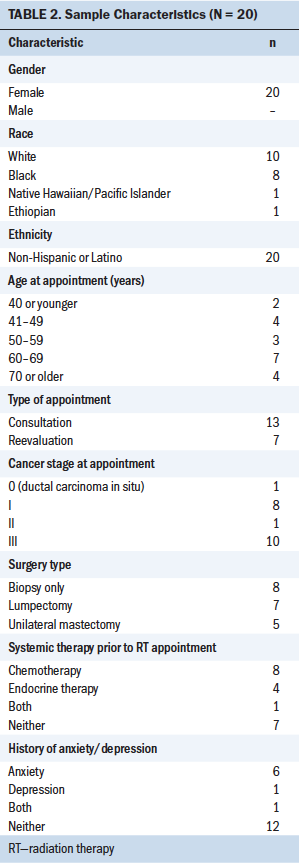
Emotional health: “What feelings or emotions did you experience after you completed your radiation treatments? How does your emotional health affect you now versus immediately after completing treatment?”
The main subcategories that emerged from the interviews included an expanse of coping mechanisms, emotional concerns, body distortion and image concerns, and the fear of recurrence. One participant asked, “How do I manage the life that I have now and still make the life that I want to be able to have?”
The lone male participant expressed feelings of isolation: “I don’t know how many times I’ve heard this. ‘No way! Men don’t get this!’” He and his wife stated feelings of isolation during his diagnosis and treatment and shared frustration with the lack of support group inclusion.
The fear of recurrence was reported by 10 participants, one of whom stated, “[The] fear that it’s going to come back . . . it’s always there. It never goes away.” A few participants relied on their faith and spirituality to manage the fear of recurrence. One participant stated the following:
I’m going to do the things I know that I can do (to prevent a recurrence), and then for me, personally, as a Christian, I have to release it to God. I know that we all have an expiration date. But, yet, still there is that fear, what is the process [of dying] going to be like?
Another participant made a deliberate decision to worry about other challenges in her life, but not a cancer recurrence: “I am worried about a lot of stuff, and I said to myself, ‘Don’t worry about it.’ . . . If it were to come, I’d deal with it.”
Access and continuity of care: “What needs did you experience related to your cancer care continuing after your radiation treatments? How important is access to your cancer care team now versus immediately after completing treatment?”
Most patients reported high satisfaction with the process of radiation therapy treatment and the friendly supportive staff, including physicians, nurses, radiation therapists, and administrative personnel. One participant said, “You guys were great throughout the whole thing. All the doctors. Everybody I encountered was great.” One participant commented on how she felt like part of a family while undergoing treatment, and verbalized a sense of loss when treatment ended and she no longer experienced the weekday support from staff. Additional positive comments included praise for the healing experienced through the art therapy program, cleanliness of the facility, and new knowledge gained by attending the weekly patient lunches where staff members presented education on a specific disease site or highlighted new research being conducted.
One participant, after undergoing chemotherapy, surgery, and radiation therapy, stated the following regarding survivorship and follow-up care: “[It is] a little confusing. What provider is going to care for what symptoms?” Another participant expressed an unmet need related to having different radiation therapy treatment times each day, which made scheduling other activities challenging. Only two participants expressed interactions during treatment that left them feeling objectified. One said, “I had 29 marks all over me, and I felt more like an object than a person as I was going through the process.”
The one male participant verbalized frustration with finding a support group that would welcome him.
No male information. Even though . . . ductal carcinoma is the same for male and female, yet, you know, when I would call up to ask, “Can I come down [to support group meetings]?” . . . they didn’t want a male there. I even called up a breast cancer foundation and everything that they advertised that you see, everything female, they might have put something for male in there, but no.
Relationships: “How did you address changes in personal relationships after your radiation treatments ended? How important are these relationships now versus immediately after completing treatment?”
The impact of treatment for breast cancer affects both personal and work relationships. One participant said, “It just sucks because you kind of get tired of having to explain to people why you can’t do things.” Many participants reported feeling relieved once radiation therapy treatment was finished; however, one verbalized a sense of sadness because her team provided a deeper sense of caring than her other social groups: “You know, that relationship we developed during my treatments . . . it was very supportive . . . and I adjusted, but you know, initially, I felt depressed when treatment ended.” Two participants reported uncertainty with how to handle work relationships and the responsibilities of transitioning back to work. One participant said, “Return-to-work transition was a big thing. . . . Sometimes it sucks to have to explain to people, like, my white blood cell count is super low . . . and, at work, like, there is an event for a lot of kids and I have to say, like, I can’t.” She suggested more information be available to employers on what to expect from employees finishing cancer treatment.
The other participant would have liked some coaching on how to inform coworkers without differential treatment.
There were some people at work who I didn’t tell because, when you say “cancer” . . . people look at you differently, and I didn’t want sympathy. . . . I didn’t want anybody pitying me. I didn’t want people to see me. I’m a supervisor at work. I supervise people, so I needed that relationship to be there as it was, so there was a lot of people I didn’t tell, but maybe a little more education on how do you . . . who to tell . . . how do you tell them . . . how do you approach the subject without people freezing? You know, face it, cancer is a frightening thing.
Another area of unmet needs that emerged was body image, sexuality, and intimacy, with nine participants reporting concerns. Some participants commented on body distortion and body image. One participant expressed avoiding intimacy after her unilateral mastectomy: “I don’t want anybody to see me nude or without clothes or any of that. I don’t want any touching or any of that, in terms of an intimate thing.” Another said, “My breasts have been big my whole life, so to have them so small, I felt like my body didn’t match anymore.”
Financial concerns: “What was your experience from a financial perspective, while on treatment or after your radiation treatments ended? What concerns do you have about finances now versus immediately after completing treatment?”
Fifteen participants reported adequate insurance coverage for treatment, and only two participants expressed any concerns with insurance or financial worries. The greatest concern was reported from the male participant:
They fought for almost a year with Medicare, and finally Medicare approved [radiation treatment] and paid for it. . . . But, Medicare, the biggest thing with Medicare was this was a male, not a female. They didn’t want to hear it. He’s a male and this doesn’t apply to males. It only applies to females.
Fortunately for this participant, treatment was not delayed because of the insurance denial and appeal process. The other participant discussed losing her job two months prior to her breast cancer diagnosis and enrolling for a large out-of-pocket deductible to keep her monthly premium low.
You read the fine print and it says $6,500 out of pocket except for, you know, then they start listing them, and then that $6,500 all of a sudden became $10,000. So there goes your savings.
Information needs: “Please explain any cancer-related information you wished you had learned while on treatment or after your radiation treatment ended. How important is learning about what I need to do to stay well?”
Nine participants verbalized unmet needs associated with a side effect of treatment. Two patients described the unexpected impact of radiation dermatitis:
The one thing that I didn’t really expect was the terrible sunburn. That was . . . I knew it might get red, but it was very, very bad sunburn to me.
In honesty, I didn’t expect that it would be so difficult. It was worse than chemo. Radiation was worse than chemo for me. Usually people are afraid of chemo, but chemo was okay, you know. A day or two after the treatment I didn’t feel well and then I came back. But radiation, the first week was okay, but then I was burnt to ashes. My breast was burnt to ashes.
One participant commented on a lack of understanding in how providers described skin changes: “I didn’t expect that to be a skin break. I didn’t understand [what a] skin break is.”
Another area of unmet needs verbalized by participants was information regarding preparation for radiation therapy treatment. With standard-of-care teaching including written and spoken education, 11 participants felt prepared for radiation therapy. Nurse case managers and radiation oncologists spend approximately two hours with patients during the initial consultation and verbally describe treatment logistics, such as side effects and the markings during the planning session. Written education is also presented to patients for reference after the consultation is completed. However, six participants reported that they still felt unfamiliar with what to expect for the treatment planning session and the first day of treatment. To improve on existing radiation therapy treatment preparation, video education was recommended by six participants. One participant stated the following:
The downfall for me anyway was the lack of preparation, emotionally, during the course of radiation . . . how many target marks would end up being placed on my body before it was finished. I felt more like an object than a person as I was going through the process . . . you’re exposed enough (open gown, bare chest).
Another participant paralleled her sentiments and reported needing more information.
What to expect with the radiation . . . you know, because even before you even start, you got to go through this mold process and, you know, exams and markings and . . . and there is a whole set up to it and there is like a method to the madness, so to speak, that you have to kind of experience.
Another participant remembered from the teaching that she would not feel the radiation beams, but stated she wished someone had told her the machines would be noisy at times.
Unmet needs in the area of nutrition were reported by eight participants. One participant said, “That’s really the only regret that I have . . . that I did not know about. I did a lot of personal research. I wouldn’t want to be eating something that could feed my cancer.”
Discussion
This study used a qualitative design to better understand the perceptions and unmet needs of patients with breast cancer after radiation therapy treatment completion. All participants expressed one or more unmet needs, and the most common number of unmet needs was six. Using the five domains from SUNS as a framework, several unmet needs emerged and were identified and associated with one or more of the 89 questions contained within the instrument. The greatest unmet needs identified in this study were from the emotional health, information needs, and relationships domains.
More than 50% of participants reported an unmet need in emotional health and relationships. Results of this study align with ongoing research evaluating emotional and physical needs of patients with cancer. A workshop conducted in 2018 assessed the progress made in the field of cancer survivorship since the IOM’s landmark report (Hewitt et al., 2005). One recommendation was to integrate psychosocial care for cancer survivors and their caregivers as a means to address the ongoing emotional needs of patients with cancer (National Academies of Science, Engineering, and Medicine, 2018). Screening patients with cancer for depression and distress should be implemented into clinical practice and incorporated into standards of care (Andersen et al., 2014; Holtzman et al., 2018). Another recommendation was to establish a means to assess physical and psychological strains as survivors re-enter the workforce after cancer treatment ends (National Academies of Science, Engineering, and Medicine, 2018).
Travis et al. (2011) reported that 20% of cancers diagnosed in the United States are a second, third, or fourth cancer. The fear of recurrence was reported by 10 of 17 study participants. Factors contributing to a secondary cancer include lifestyle practices such as smoking and lack of exercise, increasing age, genetic mutations and hereditary links, previous cancer treatment, and a combination of one or more factors. Evidence-based post-treatment guidelines for surveillance of recurrences and secondary malignancies remain in development; however, interest in designing risk-prediction models that include previous cancer treatments are currently being investigated (National Academies of Science, Engineering, and Medicine, 2018). Research continues to trial varying models of survivorship care, and recommendations include transitioning into a tiered care approach based on severity of symptoms, risk of recurrence, extent of services needed, and determination of best provider to deliver care (National Academies of Science, Engineering, and Medicine, 2018).
Radiation dermatitis has been a focus of studies aimed to understand the variations in skin changes and their impact on quality of life (Lee et al., 2017; Schnur et al., 2011). About half of the study participants reported an unmet need either in feeling prepared for radiation dermatitis or in knowing how to care for the skin-related changes. Lee et al. (2017) found that more than 90% of patients with breast cancer self-reported that the greatest unmet need related to radiation side effects was understanding and managing radiation dermatitis (Lee et al., 2017). Investigators of another study reported results that underscore the extent to which radiation dermatitis effects the physical, psychosocial, and emotional health perspective of patients with breast cancer, and they recommended the use of a multidimensional assessment tool to better evaluate the physical skin changes and the emotional impact of dermatitis (Schnur et al., 2011). In addition, healthcare providers need to be mindful of how treatment interventions for such side effects influence each patient’s ability to function at work, at home, and in social settings (National Academies of Science, Engineering, and Medicine, 2018).
Patients with breast cancer typically exhibit heightened anxiety prior to radiation therapy (Andersen et al., 2014; Murchison et al., 2019). Some of this anxiety is related to a fear of the unknown, such as the extent of side effects, treatment logistics, and how long treatment will last (Murchison et al., 2019; Thewes et al., 2004). Six of 17 study participants reported feeling unprepared for the treatment planning session or radiation therapy delivery. To better prepare patients for radiation therapy treatment, studies have improved education through verbal, written, and visual (video) modes of delivery (Halkett et al., 2012; Harrison et al., 1999; Jahraus et al., 2002; Sterba et al., 2015). Results from studies conducted with patients with breast cancer suggest that neither written nor verbal radiation therapy education adequately prepares patients for what to expect during radiation therapy treatment planning and delivery (Hahn et al., 2005; Harrison et al., 1999; Jahraus et al., 2002). Recommendations include supplementing with a form of visual education. Video education to prepare patients with breast cancer for radiation therapy treatment has been previously studied, and high patient satisfaction scores were reported (Hahn et al., 2005).
Although many of the themes identified by analyzing the transcribed interviews could be associated within the five domains of SUNS, there were other themes not included and worthy of mention, such as overall quality of life, sexuality and intimacy, gender differences (specifically the lack of support for men with breast cancer), and assessment of self-management for symptom mitigation. In addition, while identifying the unmet needs of patients with breast cancer after receiving radiation therapy treatment at an outpatient clinic, numerous positive comments emerged, such as the friendliness of the staff, benefits of the art therapy program, support from the healthcare providers, cleanliness of the facility, weekly educational lunches, follow-up visits, and the sense of belonging to a family.
Limitations
This was a single-institution qualitative study conducted using a purposive sampling method and was not intended to be generalizable; however, this research was intended to be hypothesis-generating and formative to pilot intervention development. All participants were actively engaged in their surveillance as evidenced by repeat follow-up clinic visits, and results may have varied if patients considered lost to follow-up were interviewed. Although the male perspective on receiving radiation therapy for breast cancer was enlightening, only one male participant was interviewed, and results may have been different if other male perspectives were included. Memory recall may have skewed some answers of participants who were further from their treatment experience. Socioeconomic status was measured by type of insurance only. Other socioeconomic status variables, such as level of education, household income, and occupation status, may have contributed to a greater understanding of financial concerns.
Implications for Nursing
Nurses working with patients undergoing radiation therapy for breast cancer should address each of the five health domains (emotional health, access and continuity of care, relationships, financial concerns, and information needs) during each of their comprehensive patient assessments throughout the survivorship continuum. Each of the main themes that emerged during this qualitative study has the potential to affect a patient’s adherence to surveillance guidelines and contribute to a less-than-optimal quality of life. Nurses are well equipped to meet the unmet health needs (physically, socially, and emotionally) of patients through education, identification of barriers to best health practices, and promotion of chronic disease self-management. In addition, nurses can serve as a conduit to direct patients for referral services, including social workers and other allied mental health professionals, as needed. 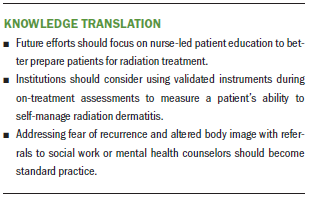
Conclusion
The significance of this study is in understanding the unmet needs of patients and their experiences after completing radiation therapy for breast cancer. This study is unique in its approach to understanding and identifying, from the patients’ perspectives, common themes of unmet needs after completion of radiation therapy for breast cancer. The data collected from participant interviews identified areas of improvement for satisfying the unmet needs of patients with breast cancer, including (a) the need to better prepare patients for the logistics of and setup for radiation therapy treatment; (b) the need to provide greater education to prepare for and manage radiation dermatitis; and (c) the need to evaluate how to incorporate instruments to assess patients for emotional health. Establishing a comprehensive educational program designed to meet the needs of patients with breast cancer can promote a patient-centric model of care aimed to meet the physical, emotional, and financial needs of cancer survivors.
The authors gratefully acknowledge Nancy Mendenhall, MD, and Gail Sarto, BSN, OCN®, for their support of nursing research and Jessica Kirwin, MA, for her assistance with editing and formatting.
About the Author(s)
Michelle Pembroke, PhD, RN, OCN®, was, at the time of this writing, a case manager at the University of Florida Health Proton Therapy Institute in Jacksonville; Julie Bradley, MD, is an associate professor in the department of radiation oncology at the University of Florida in Jacksonville; and Lynne S. Nemeth, PhD, RN, FAAN, is a professor in the College of Nursing at the Medical University of South Carolina in Charleston. This article was supported by the Jill Teston Grant, which was established at the University of Florida Health Proton Therapy Institute to support breast cancer research. All authors contributed to the conceptualization and design and manuscript preparation and provided analysis. Pembroke completed the data collection.Pembroke can be reached at michellefpembroke@gmail.com, with copy to ONFEditor@ons.org. (Submitted September 2019. Accepted February 20, 2020.)




