Racial Differences in Pain Management for Patients Receiving Hospice Care
Objectives: To investigate racial differences in implementation of 11 evidence-based cancer pain management strategies in a matched sample of patients in hospice.
Sample & Setting: 32 African American and 32 Caucasian American older adults (aged 65 years or older) with cancer pain receiving hospice care in the midwestern United States.
Methods & Variables: Matched cohort secondary data analysis of postintervention data in a cluster randomized controlled trial was used. Main outcomes are the summative and individual Cancer Pain Practice Index scores.
Results: There were few statistically significant or clinically meaningful differences in implementation of individual best practices for pain management by race. Assessment of primary pain characteristics and management of opioid-induced constipation with a bowel regimen was significantly lower in African Americans than in Caucasian Americans.
Implications for Nursing: African American older adults receiving hospice care at the end of life received pain management that was, overall, comparable to matched Caucasian American older adults. Hospice and oncology nurses play a critical role in effective pain management and should continue to implement evidence-based guidelines for pain management into daily practice. Diffusing the hospice model and principles of pain and symptom management into other settings and specialty care areas may reduce widespread pain disparities.
Jump to a section
Pain and suffering are among the most feared consequences of cancer across the adult lifespan. Although advancements have been made in the treatment of cancer, management of common cancer-related issues, such as pain, at the end of life (EOL) remains challenging, particularly in older adults. Adding to this challenge is the likelihood that older adults concurrently experience other persistent pain conditions (Brunello et al., 2019). Despite efforts to improve care of older adults with cancer pain, implementation of evidence-based pain management practices remains variable and inconsistent (Herr et al., 2010; Shuman et al., 2018). This is problematic because studies show that pain is a major physical and emotional issue for older adults and, in particular, for African Americans living with advanced cancer (Vallerand et al., 2019; Yeager et al., 2018) who are also more likely to experience disparities in cancer pain care (Anderson et al., 2002; Meghani et al., 2014). Existing knowledge of racial disparities in actual pain care practices at EOL in older adults is gravely underdeveloped. This focused retrospective secondary data analysis was conducted to identify differences in nurse-provided cancer pain management practices in a matched set of African American and Caucasian American older adults (aged 65 years or older) receiving hospice care.
Background
Cancer Pain in Older Adults
The incidence of cancer increases substantially with advancing age; 1 in 3 men aged 70 years or older and 1 in 4 women aged 70 years or older will develop some type of cancer (Siegel et al., 2019). For example, a study by Lau et al. (2016) of 2,825 individuals aged 65 or older receiving hospice care who were taking opioids during the last week of life found that 41% had cancer as their primary hospice diagnosis. In addition, many patients receiving hospice care report pain, as determined by Herr et al. (2010) in a study of 399 patients receiving hospice care; about 89% of these patients had a report of pain or an existing pain diagnosis at hospice admission. Similarly, a qualitative study by McPherson et al. (2013) of older adults with advanced cancer and their family caregivers revealed that patient participants reported having some degree of daily cancer pain as well as other types of chronic pain. Likewise, in a study by Pimentel et al. (2015) of 8,094 newly admitted nursing home residents with cancer, about 66% reported experiencing pain; more than 17% of residents in daily pain received no analgesics, including about 12% with daily severe pain and about 17% with daily moderate pain. Adequate pain management has been found to be a major concern for EOL care among older patients with cancer (Finkelstein et al., 2015).
The American Cancer Society projected for 2019 that African Americans would account for more than 200,000 new cases of cancer and about 73,000 deaths (DeSantis et al., 2019). In addition, African Americans report higher intensity of pain than other racial and ethnic populations (Kamal et al., 2017; Martinez et al., 2014) and approach cancer pain with greater negative and fatalistic stigma and fear (Im et al., 2008), perhaps because they are less knowledgeable than other populations about cancer pain management (Baker et al., 2013). It is not surprising then that, when comparing Black and White cancer survivors, Green et al. (2011) found that Black participants experienced more cancer-related pain interference (e.g., mood, work, relationships, sleep). Combined, these realities exponentially place African American older adults at risk for inadequate management of cancer pain.
Evidence-Based Practice Regarding Cancer Pain in Hospice
Cancer pain is generally poorly treated at EOL in older adults. In a study of community-based hospice settings by Herr et al. (2010), older adults with cancer received an average of 32% of key evidence-based practices (EBPs) applicable to their situation using the Cancer Pain Practice Index (CPPI). Hospice care has been slower to adopt EBPs, even those intended for pain management, despite the mission of hospice, which is to provide pain management and comfort care and improve quality of life for those with life-limiting illnesses (Jones, 2013; Sanders et al., 2010). One concern is that systematic integration of EBPs may ignore personhood and the subjective experience of suffering (Jones, 2013). Much of the research has focused on translating and assessing evidence-based pain care in nursing homes and acute care settings (Hunnicutt et al., 2017; Mack et al., 2018; Shuman et al., 2018; Titler et al., 2009). Herr et al. (2010), in their study involving 16 midwestern U.S. hospices, found that recommended EBPs for assessing and managing pain in older adults with cancer are not being fully implemented or documented. Gaps in practice observed were related to additional components of a comprehensive assessment completed within 48 hours of admission, review of the pain treatment plan at each reassessment, reassessment of moderate or greater pain, consecutive pain reports of 5 or greater (indicating pain of at least a moderate level on a scale of 0–10) followed by pain medication increases, monitoring of analgesic-induced side effects, initiation of a bowel regimen for patients with an opioid order, and documentation of nonpharmacologic therapies and written pain management plans (Herr et al., 2010). However, on a more positive note, most patients had their pain assessed at admission using a valid pain scale and had primary components of a comprehensive assessment completed at admission; in addition, most patients with admission reports of pain had medication ordered (Herr et al., 2010).
Numerous regulatory, provider, and patient barriers and facilitators further influence the use of EBPs for cancer pain in hospices. In a study by Klein-Fedyshin (2015), hospice and palliative care nurses across several sites reported a need for drug or disease information and access to evidence-based resources, including databases; the most frequent source of information was colleagues, followed by Internet searches, which could expose nurses to unreliable or noncurrent evidence for managing EOL symptoms. A study by Sanders et al. (2010) identified various institutional barriers to implementation of EBP, including lack of agency involvement, particularly in terms of spearheading and supporting EBP initiatives; insufficient staff knowledge about hospice care and pain management; and inability of staff to take on additional responsibilities. Hospices may be motivated by regulatory and quality standards or organizational values to use and improve EBP in areas such as pain treatment (Dy et al., 2015).
Few studies have addressed the degree of disparities in nurses’ delivery of evidence-based management of cancer pain in hospice settings. In a study of the nursing home setting by Mack et al. (2018), African American residents with cancer were found to be less likely to have self-reported pain documented or to receive analgesics and nonpharmacologic interventions than Caucasian American residents. In addition, African Americans have been found to receive similar or better care as Hispanic and/or Caucasian Americans in hospices for most care domains, including management of symptoms and pain, but not for emotional and religious care, according to family caregivers (Price et al., 2017; Sharma et al., 2017).
When examining individual indicators of EOL care, it is not uncommon for African American family members to be less satisfied with pain management of their loved ones, which necessitates more research to understand their experiences in hospice (Rhodes et al., 2007; Sharma et al., 2017). Conversely, studies by Campbell et al. (2012) and Stephenson et al. (2009) found that African American and Caucasian American patients and their families were satisfied with hospice interventions and pain management. Although these studies present contrasting findings, they provide insight on the extent to which quality and evidence-based pain care is provided in hospice, as well as the perceptions and roles of family members in pain management. However, individuals in racial and ethnic minorities remain under-represented in symptom science studies (Johnson, 2013), limiting knowledge of their experiences in hospice and spurring the need for the current study, which focuses on African Americans.
Methods
Design
This was a secondary data analysis of a completed cluster randomized controlled trial (RCT) designed to test a multifaceted translational intervention to diffuse and improve pain EBPs in hospices (i.e., translating research into practice–cancer [TRIP-CA], which occurred from February 2007 to February 2010). A detailed discussion of the procedures and the intervention are published elsewhere (Herr et al., 2012). The TRIP-CA intervention was developed using Rogers’s diffusion of innovation framework and involved disseminating EBPs through a multicomponent communication, education, and empowerment process to change the culture of the organizations (i.e., hospice) and users (i.e., nurses), facilitate adoption of the cancer EBPs, and positively affect patient outcomes (Herr et al., 2012). The parent study (Herr et al., 2012) did not find that the intervention improved cancer pain practices. However, it was unable to examine practices by race because of the limited total sample size of racial and ethnic minorities; consequently, examination of this topic using a matched analysis design is warranted. Matching was intended to reduce extraneous sources of variation. In addition, matching enhances validity, and having exact number of cases and controls minimizes the variance in statistical parameters (Rose & van der Laan, 2009).
Sample
Data for 32 African American older adults and 32 Caucasian American older adults were selected based on case-matching criteria: age (plus or minus three years), sex, and cancer diagnosis (when possible). This yielded 32 pairs for a total sample of 64 patients. Participants were from hospices assigned to the experimental and control arms of the RCT, and data were pooled from two time points (i.e., immediately postintervention and six months postintervention). The parent study did not find significance between the experimental and control groups (i.e., suggesting equivalence between groups) or between postintervention phases, which strengthens the case for pooling all available data for this secondary data analysis. Six months elapsed between postintervention phases, during which time no new EBP guidelines were published, limiting threats to internal validity.
Setting
The parent RCT was conducted in 16 hospices in the midwestern United States. These hospices provided care in the home and were representative of small (average daily census [ADC] = 25 or less), medium (ADC = 26–100), and large (ADC = greater than 100) institutions. Secondary data analyzed included patients from 11 hospices that were primarily medium and large urban institutions; no African Americans and three Caucasian Americans were enrolled from small, rural hospices.
The parent RCT was approved by the University of Iowa Institutional Review Board (IRB). Because this was a secondary data analysis using deidentified data, the IRB determined that additional approval was not required for this study.
Variables
The CPPI was developed using rigorous and iterative reliability and validity testing (Fine et al., 2010). The outcome variable was the adoption of the 11 EBPs listed in the CPPI for pain. These practices were related to timely, focused, and comprehensive assessment and reassessment, treatment using appropriate analgesics and nonpharmacologic therapies, the existence of a bowel regimen when taking opioids, and proper documentation. Each practice was scored either as met (1 point) or unmet (0 points) or by the number of components completed. A total CPPI score was derived by taking the number of points received on the applicable items for that particular patient (numerator) divided by the maximum score possible on each applicable item (denominator), resulting in the percentage of EBPs a patient received. For example, indicator 4 would have a range of 0–1; that is, if all components are completed, 7 would be divided by 7, and a patient would receive a score of 1. Detailed development and psychometric properties of the CPPI are provided in several articles (Fine et al., 2010; Herr et al., 2012). Song et al. (2015) used this tool to examine nursing documentation practices and reported 95% inter-rater reliability of the tool to extract data from 10 randomly selected tools.
Because the current authors’ interests lie in understanding the individual-level differences in pain between African Americans and Caucasian Americans, a total (mean) difference in total CPPI score and individual scores for each indicator between each group was calculated. The higher the CPPI score, the greater number of EBPs the patient received.
Pain intensity was measured using a 0–10 numeric rating scale, with higher scores indicating greater pain severity. The mean pain intensity for two weeks (i.e., 1–7 days and 8–14 days) and maximum pain intensity (highest pain intensity reported) were used in statistical analysis. Patients with cognitive impairment who were unable to report pain intensity were not included because other measurements of pain (such as a nonverbal pain behavior scale) were not available in most hospices. The mean difference for African Americans and Caucasian Americans was calculated for mean and maximum pain intensities.
Length of stay in hospice was determined by the number of days spent in hospice from admission to death. The mean difference in number of days spent in hospice between African Americans and Caucasian Americans was calculated and included in the predictive model as an independent variable.
Statistical Analyses
All statistical tests were performed using SAS, version 9.4, and IBM SPSS Statistics, version 23.0. The data were observed for normality, and variables did not require statistical transformation. Descriptive statistics using means and standard deviations for continuous variables and frequencies and proportions for categorical variables are used to describe participant characteristics. To identify bivariate differences in CPPI indicators, Wilcoxon rank-sum test (for practices treated as continuous/scaled variables) and chi-square test or Fisher’s exact test (for practices coded as categorical/non-scaled variables) were used. If an indicator was not met by at least 30% of participants, then no statistical comparison was made (i.e., indicators 6, 8, and 10). In addition, two African Americans and four Caucasian Americans were removed from all analyses because they did not have pain documented at admission. All analyses were two-tailed, and an alpha of 0.05 or less indicated significance.
Results
Table 1 describes characteristics of the sample, which was comprised of 40 women and 24 men, with an average age of 78 years. African Americans had lower mean pain and maximum pain intensity scores compared to Caucasian Americans, but these were not significantly different. On average, African Americans were in hospice 1.25 days less than Caucasian Americans, and significantly more African Americans were in large urban hospices compared to Caucasian Americans (p = 0.0132). 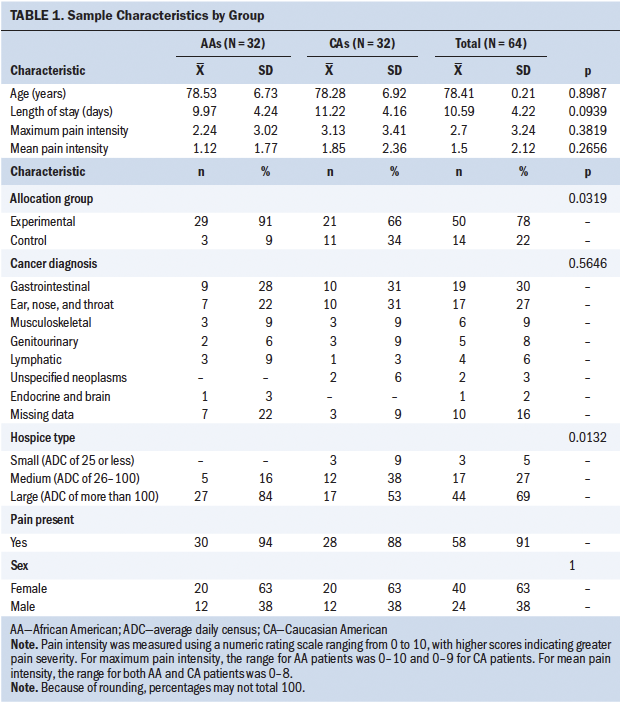
Overall, total CPPI score was also not significantly different between race groups. However, the care provided to African Americans and Caucasian Americans did not fully meet CPPI standards, as indicated by low means and the proportion of patients receiving care (see Table 2). As previously noted, there were none or too few older adults who met the criteria for indicators 6 (reports of moderate to severe pain [5 or greater] led to reassessment of pain intensity within 24 hours), 8 (consecutive reports of moderate to severe pain [5 or greater] were followed with increases in opioid dose or additional analgesic added within 24 hours), and 10 (patients with opioid orders are monitored each day for opioid-induced side effects [e.g., respiratory depression, constipation]). Bivariate analysis found no significant differences in practices between African American older adults and Caucasian American older adults, except for indicators 1 and 9, where statistically fewer African Americans had a comprehensive pain assessment at admission (p = 0.04) and orders for a bowel regimen while taking opioids (p = 0.05). Although not statistically significant, fewer African Americans received recommended care on all other indicators except 7 and 11. In these cases, more African Americans compared to Caucasian Americans had orders for non-opioids and documentation of nonpharmacologic therapies in the past week. 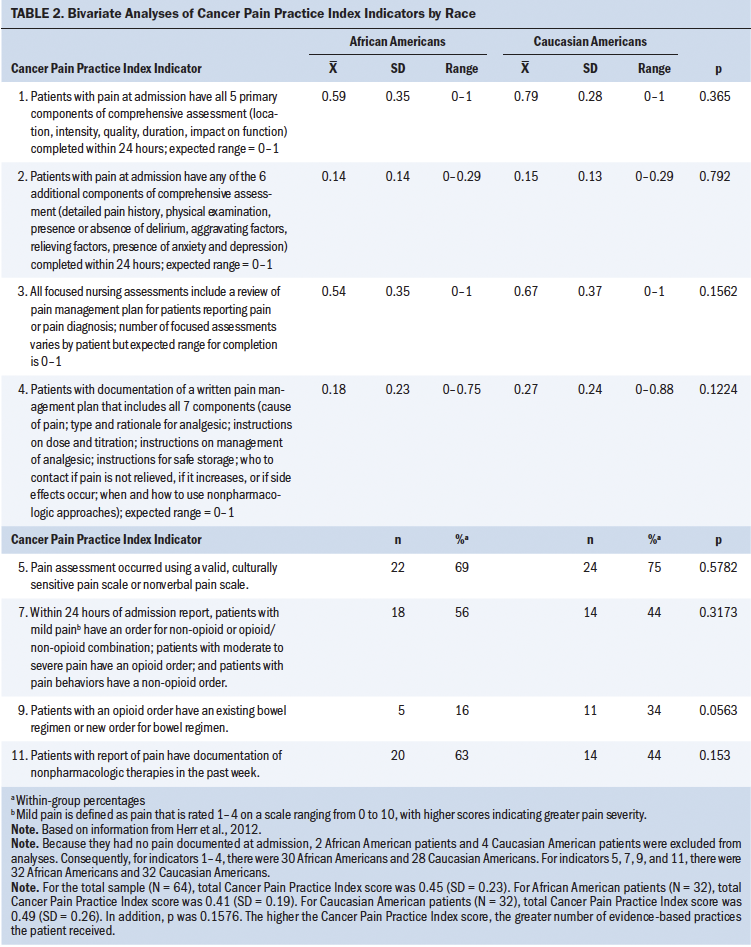
Discussion
This study provides novel insight into the pain management of African American and Caucasian American older adults receiving hospice care. Although mean CPPI score did not reveal statistically significant differences in performance of pain EBPs by providers, there was a significant difference in individual indicators, such as pain assessment between African Americans and Caucasian Americans. Fewer African Americans received a comprehensive pain assessment within 24 hours of admission, and this would undoubtedly affect the provision of the other CPPI indicators in African Americans, particularly if no standardized pain management process is in place at each hospice. Thorough and comprehensive pain assessment drives pain treatment, and an inaccurate or incomplete assessment may contribute to undermanagement. Consistent with other studies, African American older adults in hospice have a lower likelihood of having pain assessment at admission and subsequent frequent assessments (Cea et al., 2016; Mack et al., 2018). Cea et al. (2016) found that although patients in hospice aged 65 years or older received a high level of pain assessment, there was a relatively low level of use of valid pain scales. A seminal study by Anderson et al. (2002) of 31 socioeconomically disadvantaged minority patients with cancer showed that 21% of the African American participants (N = 14) reported difficulty with talking about having cancer pain, as opposed to none of the Hispanic patients (N = 17). Consequently, using a reliable and culturally sensitive tool to measure pain is important to enhance patients’ reporting of pain and to accurately measure changes in pain intensity over time. Recommendations for appropriate pain measurement tools for African American and Caucasian American older adults are available (Booker et al., 2016; Robinson-Lane & Booker, 2017; Ware et al., 2015).
In the current study, African Americans received more non-opioids and nonpharmacological interventions than Caucasian Americans. This is an interesting, yet not unusual, finding in pain and palliative care research. The reasons for this finding are unclear; however, it may be related to lower pain levels reported at admission, patient or family member preferences to avoid opioids unless necessary, and patient or family member beliefs that opioids may hasten death or cause changes in mental status (Mack et al., 2018; Stephenson et al., 2009).
Another significant finding was the lack of a bowel regimen among African Americans; fewer African Americans had an existing or new order for a bowel regimen if taking opioids. This is consistent with Lau et al.’s (2016) findings that racial minorities in hospice had lower odds of using a laxative in tandem with opioids than White participants. Post-hoc review of data from the current study found that although more Caucasian Americans had a bowel regimen, most patients (African Americans or Caucasian Americans) had either a stool softener or a laxative, but not both as recommended. Without a complete bowel regimen, opioid users may experience additional distressing symptoms, such as opioid-induced constipation.
There were few significant differences in the number of African Americans and Caucasian Americans receiving or not receiving evidence-based pain care. Although this finding is encouraging, it also highlights significant gaps in optimal care for both groups. To meet the standard, all components of each CPPI indicator had to be addressed. In some cases, only parts of the standard were performed. For example, one participant had four reports of moderate to severe pain, but the nurse(s) followed up with a reassessment within 24 hours just twice (indicator 6). Similarly, the majority of older adult patients in hospice using opioids were not being monitored for opioid-induced side effects (indicator 10). This is a major issue because these side effects could create additional pain and suffering during the EOL transition.
Nurses may be partially compliant with standards, but practice is often not consistent, in part because of the lack of diffusion of and education on EBP in healthcare settings. For example, using an evaluation tool modified from the CPPI, Song et al. (2015) examined documentation of evidence-based cancer pain management by nurses on an oncology unit and determined that the participating nurses documented 90% of the recommended EBPs; however, documentation was suboptimal for pain reassessment, pharmacologic interventions, and bowel regimen.
In addition, any differences in frequency of EBPs, significant or not, suggest that differences may not be based on race but on care setting. Race does not always predict disparities or inequities in health because it is only one aspect of many social determinants that affect how pain care is provided and received. A study by Price et al. (2017) reported that caregivers of African American and Hispanic patients reported slightly better care experiences than Caucasian Americans when care is provided within the same hospice; the proportion of caregivers satisfied with getting help for symptoms was comparable across the three racial groups. Similarly, Sharma et al. (2017) did not find significant racial differences in various aspects of the quality of EOL care. The current study extends the knowledge base across multiple community-based hospices, not just within an individual hospice organization.
Although not a strong focus of the current study, mean pain intensities were generally low, which could be attributed to under-reporting, particularly if the patient was actively dying and unable to fully perceive and communicate pain. In addition, in contrast to the existing literature, pain intensity was higher in Caucasian Americans, but there was no significant difference between races. This is clinically meaningful because most research consistently highlights that African Americans not only report higher pain intensity but also have lower pain thresholds (Ezenwa et al., 2018; Kim et al., 2017; Martinez et al., 2014). Pain intensity may have been lower in African Americans for several reasons. The literature shows that African American older adults are less likely to have a self-reported pain score documented (Mack et al., 2018) and that they commonly under-report and minimize pain (Booker, 2016); this may have been the case in the current study, given the number of pain reports documented as zero. Culturally, differences in pain reporting may indicate that African American older adults are less open to complaining about pain and feel uncomfortable showing or sharing when pain is severe, particularly those who are at EOL. Unfortunately, this leads to under-reporting. It is also possible that numeric pain scores may not accurately reflect African Americans’ cancer pain experience, in that there may be other areas that are more important than pain intensity, such as function or mood, which are more introspective of the totality of pain severity. At this time, there are no brief, culturally appropriate tools to measure cancer pain intensity.
Another reason that pain intensity may have been lower in African Americans in this study is that, because cancer pain is not always persistent, perhaps the participants were not experiencing pain at the time of assessment. In addition, although the subjectivity of pain intensity varies across and within individuals, having the same or similar cancer pathology between both racial groups may have contributed to an insignificant difference in pain intensity. African Americans having shorter hospice stays could have affected the mean and maximum pain intensities, particularly if they were unable to consistently self-report numeric pain intensity at EOL; in the current study, there was no use of a nonverbal pain scale. Studies show that African Americans use hospice care at much lower rates than Caucasian Americans, often delaying being discharged to hospice until late in the disease trajectory or disenrolling from hospice altogether (Haines et al., 2018; Rizzuto & Aldridge, 2018). As a result, capturing pain consistently is a practical and methodologic issue worth further investigation.
Although hospice use is lower for African Americans, a review by Wilkie and Ezenwa (2012) concluded that there are fewer racial disparities than expected in pain management at EOL, suggesting that hospice and palliative care may be effectively fulfilling its role in adequately providing pain relief to dying patients. In addition, EBP use in cancer pain management is more satisfactory than expected, given that pain is a common problem encountered in oncology nursing practice.
Strengths and Limitations
The current study had several strengths; it used a validated EBP tool; had limited missing data on variables of interest, which reflects the sustained engagement of nursing staff at study sites; and employed participant matching. However, a few limitations of the study were identified. Some may consider race to be an arbitrary measure of assessing for disparities; any significant findings could be a result of the culture of care in various hospices rather than race. Perhaps a larger sample size could further explicate racial mechanisms; the authors acknowledge the small-scale nature of this secondary analysis. In addition, there were too few African Americans in the preintervention phase for a comparative analysis with postintervention phases, and exclusion of older adults with cognitive impairment further limits understanding of cancer pain and its management in this vulnerable group. Because of the small sample size, no African American participant was from a small hospice, which precludes understanding of how race affects pain care in more intimate settings. Also, the data from this study are more than 10 years old; however, these data are often difficult to obtain given the contextual circumstances related to hospice use, length of stay, and ethical concerns surrounding research at EOL (Mackin et al., 2009). The current study had a unique opportunity to examine racial differences to address an identified gap in the literature. This foundational study raises questions and the need for additional prospective study, given that it takes, on average, 17–23 years for research to be translated into practice (Morris et al., 2011). Findings from the current study remain relevant in the present climate of pain management and can serve as a model for improving nursing practice. Most importantly, this research adds to the limited knowledge base on cancer pain and its treatment in an older, diverse population receiving hospice care, providing promising results that disparities may not exist, may be improving, or may be less pervasive in settings of hospice for older adults.
Implications for Nursing
Nursing Practice
The Institute of Medicine (2013) report Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis states that the U.S. healthcare system is inadequately equipped to support cancer care that is evidence based and cost effective; as such, improving knowledge of the clinical workforce through dissemination of EBP guidelines is one feasible solution to enhancing cancer pain management. Although the parent RCT study used this approach and found no significant differences in care, nurses and other healthcare professionals are still expected to possess the knowledge and skills necessary to manage cancer pain amid physiological and psychological challenges that aging and chronic disease present.
In 2018, the American Society for Pain Management Nursing released a position statement on management of pain at EOL and made recommendations that support the current study’s indicators for good pain care (Coyne et al., 2018). Specifically, pain management should be comprehensive and ongoing, particularly in patients who are nonverbal; in addition, healthcare providers should obtain evidence-based education and support patients’ wishes, and they should make nonpharmacologic and pharmacologic treatments accessible (Coyne et al., 2018). A position statement from the American Nurses Association (2018) also reinforces the ethical position of nurses to provide good pain management and reduce suffering amid the national opioid problem. In the midst of challenges related to pain care and the opioid crisis, high-quality pain care is imperative because many individuals’ preferences for EOL care are centered on alleviating pain and suffering (Arnstein & Herr, 2019; Institute of Medicine, 2014).
Nurses and other providers should continuously engage in quality improvement to ensure that gains in reducing disparities are maintained, as well as to increase effective pain management for all older adults with cancer. Providers at all levels must consider ways to deliver population health interventions that focus on prevention and palliation of pain in the older adult population because there may be potential to extend the hospice and palliative care model outside of traditional hospice settings. Greater hospice and palliative care consultation use could reduce racial disparities in pain management and EOL care (Johnson et al., 2016; Kamal et al., 2017). In addition, models of care should also actively engage caregivers, ensuring that they have the knowledge and skills to care for and advocate for their dying loved ones. One promising intervention for African Americans living with cancer is Power Over Pain–Coaching, which was developed to improve function and decrease pain-related distress (Vallerand et al., 2018). Initiating this intervention early in the diagnosis, when possible, may offset any inequities and disparities that patients may experience once they transition to hospice-based treatment, particularly if patients and caregivers are empowered to advocate for and implement a home-based pain management routine.
Research
Findings from the current study support two of the National Institute of Nursing Research’s (2016) scientific foci: symptom management and EOL and palliative care. In this study, the authors were able to provide a more careful look at evidence-based pain practices rather than patient-reported pain outcomes. Evaluating processes and practices in addition to outcomes is often overlooked. This work provides a launching point for additional research to establish methods to translate best practices across settings of care and populations and to measure quality of hospice and palliative care not only from a nursing perspective but also from a patient perspective. Future research might explore the extent to which culturally informed EBPs of pain are implemented, particularly for hospices where there is more racial and ethnic diversity. Nurses’ compliance with established standards and use of pain tools, along with partnerships with family members and caregivers, is imperative to providing good evidence-based pain care. Synergistic leadership and practice between an institution’s administration and clinical staff will contribute to a culture of EBP in more autonomous settings, such as community-based hospices.
Policy
The National Quality Forum (NQF) adopted standards to assess and manage conditions and symptoms, including pain (NQF, 2012b), and to have a documented plan of care for pain in individuals undergoing chemotherapy and radiation (NQF, 2012a). The adoption of pain-related NQF policies by the Centers for Medicare and Medicaid Services (CMS) is encouraging. CMS (2019) requires hospices to report the number of patients being treated with opioids who have an established bowel regimen, who receive pain screening during admission, and who undergo comprehensive pain assessment if they screened positive for pain during admission. However, pain outcomes in hospice settings (e.g., skilled nursing facilities providing hospice care, inpatient hospice clinics, outpatient or community-based hospice) should be expanded to include other relevant best practices. Examples include tracking opioid-induced adverse effects, documenting pain management plans, and permitting patients to use their allowable one-time visit with a healthcare provider to discuss options for pain management. Measuring What Matters is a joint initiative of the American Academy of Hospice and Palliative Medicine and the Hospice and Palliative Nurses Association; it consists of 10 clinically relevant indicators for measuring quality hospice and palliative care and includes specific measures for pain screening and treatment (Dy et al., 2015). The Interagency Pain Research Coordinating Committee (2016), in National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain, offers recommendations
to increase the precision of information about chronic pain prevalence overall, for specific types of pain, and in specific population groups and to track changes in pain prevalence, impact, treatment over time, to enable evaluation of population-level interventions and identification of emerging needs. (p. 4)
Transforming clinical practice, research, and policy into best practices for older adults is a critical component of reducing the burden of pain and, subsequently, disparities in this population. Healthcare providers cannot lose sight of the goal of ensuring that practices and policies sufficiently address those with cancer pain. 
Conclusion
The current study uncovered few significant differences in pain management practices between races at EOL in home-based hospice. Older adults make up a large population of patients confronted with cancer pain at EOL, and it is and will remain imperative that nurses understand that pain is best managed when EBPs are implemented consistently and equitably.
The authors gratefully acknowledge Lauren Sager, MS, for her assistance in statistical preparation and analysis.
About the Author(s)
Staja Q. Booker, PhD, RN, is an assistant professor in the College of Nursing at the University of Florida in Gainesville; Keela A. Herr, PhD, RN, AGSF, FGSA, FAAN, is the Kelting Professor in Nursing and the associate dean for faculty in the College of Nursing at the University of Iowa in Iowa City; and Cynthia Wilson Garvan, PhD, MA, is a research professor in the College of Medicine, Department of Anesthesiology, at the University of Florida. This study was supported by grants from the National Cancer Institute (R01CA115363 [principal investigator (PI): Herr]), the National Institute of Nursing Research (T32 NR011147 [co-PI: Herr]), and the National Institute on Aging (T32 T32AG049673-01S1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors provided analysis and contributed to the con-ceptualization, design, and manuscript preparation. Booker and Garvan provided statistical support. Booker can be reached at bookers@ufl.edu, with copy to ONFEditor@ons.org. (Submitted August 2019. Accepted November 4, 2019.)
References
American Nurses Association. (2018). The ethical responsibility to manage pain and the suffering it causes. https://www.nursingworld.org/~495e9b/globalassets/docs/ana/ethics/theet…
Anderson, K.O., Richman, S.P., Hurley, J., Palos, G., Valero, V., Mendoza, T.R., . . . Cleeland, C.S. (2002). Cancer pain management among underserved minority outpatients: Perceived needs and barriers to optimal control. Cancer, 94(8), 2295–2304. https://doi.org/10.1002/cncr.10414
Arnstein, P., & Herr, K. (2019). Shifting focus: From the opioid crisis to quality pain management. Journal of Gerontological Nursing, 45(6), 3–5. https://doi.org/10.3928/00989134-20190509-01
Baker, T.A., O’Connor, M.L., Roker, R., & Krok, J.L. (2013). Satisfaction with pain treatment in older cancer patients: Identifying variants of discrimination, trust, communication, and self-efficacy. Journal of Hospice and Palliative Nursing, 15(8), 455–463. https://doi.org/10.1097/NJH.0b013e3182a12c24
Booker, S.Q. (2016). African Americans’ perceptions of pain and pain management: A systematic review. Journal of Transcultural Nursing, 27(1), 73–80. https://doi.org/10.1177/1043659614526250
Booker, S.Q., Herr, K.A., & Tripp-Reimer, T. (2016). Culturally conscientious pain measurement in older African Americans. Western Journal of Nursing Research, 38(10), 1354–1373. https://doi.org/10.1177/0193945916648952
Brunello, A., Ahcene-Djaballah, S., Lettiero, A., Tierno, G., Fiduccia, P., Guglieri, I., . . . Zagonel, V. (2019). Prevalence of pain in patients with cancer aged 70 years or older: A prospective observational study. Journal of Geriatric Oncology, 10(4), 637–642. https://doi.org/10.1016/j.jgo.2019.01.005
Campbell, C.L., Baernholdt, M., Yan, G., Hinton, I.D., & Lewis, E. (2012). Racial/ethnic perspectives on the quality of hospice care. American Journal of Hospice and Palliative Medicine, 30(4), 347–353. https://doi.org/10.1177/1049909112457455
Cea, M.E., Reid, M.C., Inturrisi, C., Witkin, L.R., Prigerson, H.G., & Bao, Y. (2016). Pain assessment, management, and control among patients 65 years or older receiving hospice care in the U.S. Journal of Pain and Symptom Management, 52(5), 663–672. https://doi.org/10.1016/j.jpainsymman.2016.05.020
Centers for Medicare and Medicaid Services. (2019). Current measures. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Ins…
Coyne, P., Mulvenon, C., & Paice, J.A. (2018). American Society for Pain Management Nursing and Hospice and Palliative Nurses Association position statement: Pain management at the end of life. Pain Management Nursing, 19(1), 3–7. https://doi.org/10.1016/j.pmn.2017.10.019
DeSantis, C.E., Miller, K.D., Goding Sauer, A., Jemal, A., & Siegel, R.L. (2019). Cancer statistics for African Americans, 2019. CA: A Cancer Journal for Clinicians, 69(3), 211–233. https://doi.org/10.3322/caac.21555
Dy, S.M., Kiley, K.B., Ast, K., Lupu, D., Norton, S.A., McMillan, S.C., . . . Casarett, D.J. (2015). Measuring what matters: Top-ranked quality indicators for hospice and palliative care from the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association. Journal of Pain and Symptom Management, 49(4), 773–781. https://doi.org/10.1016/j.jpainsymman.2015.01.012
Ezenwa, M.O., Molokie, R.E., Wang, Z.J., Yao, Y., Suarez, M.L., Dyal, B., . . . Wilkie, D.J. (2018). Differences in sensory pain, expectation, and satisfaction reported by outpatients with cancer or sickle cell disease. Pain Management Nursing, 19(4), 322–332. https://doi.org/10.1016/j.pmn.2017.11.010
Fine, P., Herr, K., Titler, M., Sanders, S., Cavanaugh, J., Swegle, J.,. . . Reyes, J. (2010). The Cancer Pain Practice Index: A measure of evidence-based adherence for cancer pain management in older adults in hospice care. Journal of Pain and Symptom Management, 39(5), 791–802. https://doi.org/10.1016/j.jpainsymman.2009.09.027
Finkelstein, E.A., Bilger, M., Flynn, T.N., & Malhotra, C. (2015). Preferences for end-of-life care among community-dwelling older adults and patients with advanced cancer: A discrete choice experiment. Health Policy, 119(11), 1482–1489. https://doi.org/10.1016/j.healthpol.2015.09.001
Green, C.R., Hart-Johnson, T., & Loeffler, D.R. (2011). Cancer-related chronic pain: Examining quality of life in diverse cancer survivors. Cancer, 117(9), 1994–2003. https://doi.org/10.1002/cncr.25761
Haines, K.L., Jung, H.S., Zens, T., Turner, S., Warner-Hillard, C., & Agarwal, A. (2018). Barriers to hospice care in trauma patients: The disparities in end-of-life care. American Journal of Hospice and Palliative Care, 35(8), 1081–1084. https://doi.org/10.1177/1049909117753377
Herr, K., Titler, M., Fine, P.G., Sanders, S., Cavanaugh, J.E., Swegle, J., . . . Forcucci, C. (2012). The effect of a translating research into practice (TRIP)—Cancer intervention on cancer pain management in older adults in hospice. Pain Medicine, 13(8), 1004–1017. https://doi.org/10.1111/j.1526-4637.2012.01405.x
Herr, K., Titler, M., Fine, P., Sanders, S., Cavanaugh, J., Swegle, J., . . . Tang, X. (2010). Assessing and treating pain in hospices: Current state of evidence-based practices. Journal of Pain and Symptom Management, 39(5), 803–819. https://doi.org/10.1016/j.jpainsymman.2009.09.025
Hunnicutt, J.N., Tjia, J., & Lapane, K.L. (2017). Hospice use and pain management in elderly nursing home residents with cancer. Journal of Pain and Symptom Management, 53(3), 561–570. https://doi.org/10.1016/j.jpainsymman.2016.10.369
Im, E.-O., Lim, H.-J., Clark, M., & Chee, W. (2008). African American cancer patients’ pain experience. Cancer Nursing, 31(1), 38–46. https://doi.org/10.1097/01.ncc.0000305685.59507.9e
Institute of Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. National Academies Press.
Institute of Medicine. (2014). Dying in America: Improving quality and honoring individual preferences near the end of life: Key findings and recommendations. National Academies Press.
Interagency Pain Research Coordinating Committee. (2016). National pain strategy: A comprehensive population health-level strategy for pain. https://www.iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy…
Johnson, K.S. (2013). Racial and ethnic disparities in palliative care. Journal of Palliative Medicine, 16(11), 1329–1334. https://doi.org/10.1089/jpm.2013.9468
Johnson, K.S., Payne, R., Kuchibhatla, M.N., & Tulsky, J.A. (2016). Are hospice admission practices associated with hospice enrollment for older African Americans and Whites? Journal of Pain and Symptom Management, 51(4), 697–705. https://doi.org/10.1016/j.jpainsymman.2015.11.010
Jones, B.W. (2013). Evidence-based practice in hospice: Is qualitative more appropriate than quantitative? Home Healthcare Nurse, 31(4), 184–188. https://doi.org/10.1097/NHH.0b013e3182885ec4
Kamal, A.H., Bull, J., Wolf, S.P., Portman, D., Strand, J., & Johnson, K.S. (2017). Unmet needs of African Americans and Whites at the time of palliative care consultation. American Journal of Hospice and Palliative Medicine, 34(5), 461–465. https://doi.org/10.1177/1049909116632508
Kim, H.J., Yang, G.S., Greenspan, J.D., Downton, K.D., Griffith, K.A., Renn, C.L., . . . Dorsey, S.G. (2017). Racial and ethnic differences in experimental pain sensitivity: Systematic review and meta-analysis. Pain, 158(2), 194–211. https://doi.org/10.1097/j.pain.0000000000000731
Klein-Fedyshin, M. (2015). Translating evidence into practice at the end-of-life: Information needs, access and usage by hospice and palliative nurses. Journal of Hospice and Palliative Nursing, 17(1), 24–30. https://doi.org/10.1097/NJH.0000000000000117
Lau, D.T., Dwyer, L.L., & Shega, J.W. (2016). Concomitant opioid and laxative use in older adults in hospice care in the United States: 2007. Journal of the American Geriatrics Society, 64(11), e160–e165. https://doi.org/10.1111/jgs.14462
Mack, D.S., Hunnicutt, J.N., Jesdale, B.M., & Lapane, K.L. (2018). Non-Hispanic Black-White disparities in pain and pain management among newly admitted nursing home residents with cancer. Journal of Pain Research, 11, 753–761. https://doi.org/10.2147/JPR.S158128
Mackin, M.L., Herr, K., Bergen-Jackson, K., Fine, P., Forcucci, C., & Sanders, S. (2009). Research participation by older adults at end of life: Barriers and solutions. Research in Gerontological Nursing, 2(3), 162–171. https://doi.org/10.3928/19404921-20090421-05
Martinez, K.A., Snyder, C.F., Malin, J.L., & Dy, S.M. (2014). Is race/ethnicity related to presence or severity of pain in colorectal and lung cancer? Journal of Pain and Symptom Management, 48(6), 1050–1059. https://doi.org/10.1016/j.jpainsymman.2014.02.005
McPherson, C.J., Hadjistavropoulos, T., Lobchuk, M.M., & Kilgour, K.N. (2013). Cancer-related pain in older adults receiving palliative care: Patient and family caregiver perspectives on the experience of pain. Pain Research and Management, 18(6), 293–300. https://doi.org/10.1155/2013/439594
Meghani, S.H., Kang, Y., Chittams, J., McMenamin, E., Mao, J.J., & Fudin, J. (2014). African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: A mediation analysis study. Journal of Clinical Oncology, 32(25), 2773–2779. https://doi.org/10.1200/JCO.2013.54.7992
Morris, Z.S., Wooding, S., & Grant, J. (2011). The answer is 17 years, what is the question: Understanding time lags in translational research. Journal of the Royal Society of Medicine, 104(12), 510–520. https://doi.org/10.1258/jrsm.2011.110180
National Institute of Nursing Research. (2016). The NINR Strategic Plan: Advancing science, improving lives. A vision for nursing science. https://www.ninr.nih.gov/sites/files/docs/NINR_StratPlan2016_reduced.pdf
National Quality Forum. (2012a). Endorsement summary: Cancer measures. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&Item…
National Quality Forum. (2012b). Endorsement summary: Palliative care and end-of-life care measures. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&Item…
Pimentel, C.B., Briesacher, B.A., Gurwitz, J.H., Rosen, A.B., Pimentel, M.T., & Lapane, K.L. (2015). Pain management in nursing home residents with cancer. Journal of the American Geriatrics Society, 63(4), 633–641. https://doi.org/10.1111/jgs.13345
Price, R.A., Parast, L., Haas, A., Teno, J.M., & Elliott, M.N. (2017). Black and Hispanic patients receive hospice care similar to that of White patients when in the same hospices. Health Affairs, 36(7), 1283–1290. https://doi.org/10.1377/hlthaff.2017.0151
Rhodes, R.L., Teno, J.M., & Connor, S.R. (2007). African American bereaved family members’ perceptions of hospice care: Lessened disparities, but opportunities to improve remain. Journal of Pain and Symptom Management, 34(5), 472–479. https://doi.org/10.1016/j.jpainsymman.2007.06.004
Rizzuto, J., & Aldridge, M.D. (2018). Racial disparities in hospice outcomes: A race or hospice-level effect? Journal of the American Geriatrics Society, 66(2), 407–413. https://doi.org/10.1111/jgs.15228
Robinson-Lane, S.G., & Booker, S.Q. (2017). Culturally responsive pain management for Black older adults. Journal of Gerontological Nursing, 43(8), 33–41. https://doi.org/10.3928/00989134-20170224-03
Rose, S., & van der Laan, M.J. (2009). Why match? Investigating matched case-control study designs with causal effect estimation. International Journal of Biostatistics, 5(1), 1. https://doi.org/10.2202/1557-4679.1127
Sanders, S., Mackin, M.L., Reyes, J., Herr, K., Titler, M., Fine, P., & Forcucci, C. (2010). Implementing evidence-based practices: Considerations for the hospice setting. American Journal of Hospice and Palliative Medicine, 27(6), 369–376. https://doi.org/10.1177/1049909109358695
Sharma, R.K., Freedman, V.A., Mor, V., Kasper, J.D., Gozalo, P., & Teno, J.M. (2017). Association of racial differences with end-of-life care quality in the United States. JAMA Internal Medicine, 177(12), 1858–1860. https://doi.org/10.1001/jamainternmed.2017.4793
Shuman, C.J., Xie, X.-J., Herr, K.A., & Titler, M.G. (2018). Sustainability of evidence-based acute pain management practices for hospitalized older adults. Western Journal of Nursing Research, 40(12), 1749–1764. https://doi.org/10.1177/0193945917738781
Siegel, R.L., Miller, K.D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(1), 7–34. https://doi.org/10.3322/caac.21551
Song, W., Eaton, L.H., Gordon, D.B., Hoyle, C., & Doorenbos, A.Z. (2015). Evaluation of evidence-based nursing pain management practice. Pain Management Nursing, 16(4), 456–463. https://doi.org/10.1016/j.pmn.2014.09.001
Stephenson, N., Dalton, J.A., Carlson, J., Youngblood, R., & Bailey, D. (2009). Racial and ethnic disparities in cancer pain management. Journal of the National Black Nurses’ Association, 20(1), 11–18.
Titler, M.G., Herr, K., Brooks, J.M., Xie, X.-J., Ardery, G., Schilling, M.L., . . . Clarke, W.R. (2009). Translating research into practice intervention improves management of acute pain in older hip fracture patients. Health Services Research, 44(1), 264–287. https://doi.org/10.1111/j.1475-6773.2008.00913.x
Vallerand, A.H., Hasenau, S.M., Robinson-Lane, S.G., & Templin, T.N. (2018). Improving functional status in African Americans with cancer pain: A randomized clinical trial. Oncology Nursing Forum, 45(2), 260–272. https://doi.org/10.1188/18.ONF.260-272
Vallerand, A.H., Templin, T.N., Hasenau, S.M., & Maly, A. (2019). Modifiable pathways from pain to functional status: Confirmatory baseline results from a randomised trial of African American patients with cancer pain. European Journal of Cancer Care, 28(2), e12994. https://doi.org/10.1111/ecc.12994
Ware, L.J., Herr, K.A., Booker, S.S., Dotson, K., Key, J., Poindexter, N., . . . Packard, A. (2015). Psychometric evaluation of the Revised Iowa Pain Thermometer (IPT-R) in a sample of diverse cognitively intact and impaired older adults: A pilot study. Pain Management Nursing, 16(4), 475–482. https://doi.org/10.1016/j.pmn.2014.09.004
Wilkie, D.J., & Ezenwa, M.O. (2012). Pain and symptom management in palliative care and at the end of life. Nursing Outlook, 60(6), 357–364. https://doi.org/10.1016/j.outlook.2012.08.002
Yeager, K.A., Quest, T.E., Vena, C., & Sterk, C.E. (2018). Living with symptoms: A qualitative study of Black adults with advanced cancer living in poverty. Pain Management Nursing, 19(1), 34–45. https://doi.org/10.1016/j.pmn.2017.10.017




