Trajectories of Depression and Anxiety in Latina Breast Cancer Survivors
Objectives: To identify subgroups of Latina breast cancer survivors with unique trajectories of depression and anxiety and examine predictors associated with these subgroups.
Sample & Setting: Secondary analysis of Latina breast cancer survivors (N = 293) from three psychosocial intervention studies.
Methods & Variables: Depression and anxiety were assessed at intake and at weeks 8 and 16. Group-based growth mixture modeling was used to identify subgroups who followed distinct trajectories of depression and anxiety. Multinomial logistic regression models were used to identify predictors of trajectory-based subgroup membership.
Results: Three trajectories emerged for depression: low/moderate-stable (78%), high-improving (7%), and high-stable (15%). Three subgroups based on the trajectories of anxiety were low-stable (73%), high-improving (18%), and high-worsening (9%). Chemotherapy, age, and social support discriminated among the three depression trajectory subgroups. All anxiety trajectory subgroups had significantly different initial scores. No demographic or clinical factors were associated with anxiety trajectories.
Implications for Nursing: Latina women treated for breast cancer are at an elevated risk for depression and anxiety and follow distinct trajectories of these symptoms. Psychosocial interventions are needed to manage these symptoms, particularly for subgroups in which depression and anxiety persist or worsen.
Jump to a section
Latinos represent the fastest-growing ethnic minority in the United States and are overrepresented among lower socioeconomic and underserved groups (Ennis, Rios-Vargas, & Albert, 2011). Latina women often are diagnosed with breast cancer at younger ages, with more advanced disease, and have lower five-year survival rates than non-Hispanic White (NHW) breast cancer survivors by an estimated 20% (Siegel, Miller, & Jemal, 2017; Yanez, Thompson, & Stanton, 2011). Latina women also have poorer adjustment to a breast cancer diagnosis (Spencer et al., 1999) and greater overall distress (Eversley et al., 2005), with more social disruption as a result of their disease (Petronis, Carver, Antoni, & Weiss, 2003) compared to NHWs, Asians, and African Americans (Ashing-Giwa, Tejero, Kim, Padilla, & Hellemann, 2007). In addition, Latina breast cancer survivors report a greater number of cancer-related symptoms (Badger et al., 2013; Fu et al., 2009) and an overall symptom burden that results in lower quality of life (QOL) (Ashing-Giwa et al., 2007; Yanez et al., 2011) and emotional well-being (Janz et al., 2014).
Prevalence estimates of depression range from 32%–36% among Latina survivors (Holden, Ramirez, & Gallion, 2014) compared to 12%–25% among NHW breast cancer survivors (Krebber et al., 2014). Often comorbid with depression, anxiety is also disproportionately experienced by Latina versus NHW breast cancer survivors (Sammarco & Konecny, 2010) and is positively associated with younger age, greater pain, less education, and higher levels of fatigue (Janz et al., 2011). When untreated, psychological symptoms of depression and anxiety adversely affect QOL (Fann et al., 2008; Jacobsen & Jim, 2008), impair cancer-related immune function (Liu et al., 2012; Spiegel, Giese-Davis, Taylor, & Kraemer, 2006), and, when severe and persistent, may decrease long-term survival (Giese-Davis et al., 2011; Siegel et al., 2017). In Latina women, these consequences are even more pronounced (Ashing-Giwa, Rosales, Lai, & Weitzel, 2013; Ell et al., 2008; Yanez et al., 2011). They report fewer interactions with a mental healthcare provider or social worker and are less likely to receive medications for a mental health condition as compared to NHWs (Costas-Muñiz, Hunter-Hernández, Garduño-Ortega, Morales-Cruz, & Gany, 2017).
Despite the previously mentioned evidence from cross-sectional studies, longitudinal studies of depression and anxiety in Latina breast cancer survivors are lacking. Analyses of data from predominantly NHW samples (Avis, Levine, Case, Naftalis, & Van Zee, 2015; Kyranou et al., 2014; Saboonchi, Petersson, Wennman-Larsen, Alexanderson, & Vaez, 2015) have identified several distinct patterns of longitudinal changes in depression and anxiety after a breast cancer diagnosis. These include improving depression and anxiety over time, chronically high depression and anxiety, and a trajectory of worsening depression over time. Avis et al. (2015) found that women who followed the worsening trajectory were more likely to be non-White and of lower socioeconomic status, but low sampling of Latina women with breast cancer precluded a more detailed analysis of this ethnic group.
This secondary analysis is among the first to use a large (N = 293) sample of Latina breast cancer survivors to determine if distinct longitudinal trajectories for depression and anxiety exist in this population. Using the symptom experience model (Armstrong, 2003, 2014) as a conceptual framework to guide variable selection for this longitudinal analysis, the authors explored demographic, clinical, and psychosocial characteristics of the survivors to determine if they were predictive of depression and anxiety trajectories during the subsequent 16 weeks.
Methods
Sample and Setting
From 2008–2016, 293 Latina women receiving chemotherapy, hormonal therapy, or targeted therapy for breast cancer with or without radiation therapy and their designated informal cancer caregivers were recruited for participation in three randomized controlled trials (RCTs). Each RCT provided eight-week psychosocial interventions designed to improve QOL: telephone interpersonal counseling intervention versus telephone heath education (Badger, Segrin, Dorros, Meek, & Lopez, 2007; Badger et al., 2013; Segrin et al., 2005). Although the two interventions included women with breast cancer and their informal caregivers, only women with breast cancer were included in this analysis. All participants provided written informed consent prior to participation. The University of Arizona Institutional Review Board approved all research procedures prior to commencement of the studies. The details regarding these trials and their results have been previously published (Badger et al., 2007, 2013; Segrin et al., 2005). There were significant improvements in all intervention arms over time, with few differences among them. This secondary analysis included the adjustment for trial arm in all statistical models.
Variables
Data were collected by telephone at the time of trial enrollment, immediately after the 8-week interventions, and at 16-week follow-up. Participants had a choice of completing the measures in English or Spanish, using previously translated and validated versions.
Depression: The Center for Epidemiologic Studies–Depression (CES-D) scale is a 20-item instrument for the measurement of depressive symptoms (Hann, Winter, & Jacobsen, 1999; Radloff, 1977). For the English and Spanish versions of the scale, the internal consistency reliability exceeded 0.9 at all three time points. The CES-D provides a cutoff of 16 or higher to aid in the identification of individuals at risk for clinical depression, with good sensitivity (Ganz et al., 2002; Hann et al., 1999; Radloff, 1977).
Anxiety: The symptom of anxiety was measured with two different instruments over the course of the three studies. For studies 1 and 2, the Spielberger State-Trait Anxiety Inventory (STAI) was used. STAI is a 20-item instrument wherein a summed score ranging from 20–80 is calculated, with higher scores indicating greater anxiety (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983; Spielberger, Gorsuch, & Lushene, 1982). The internal consistency reliability was greater than 0.89 at all three time points for English and Spanish. In study 3, anxiety was measured using the PROMIS (Patient-Reported Outcomes Measurement Information System) eight-item short form. The items evaluate fear, anxious misery, hyperarousal, and somatic symptoms related to arousal. The PROMIS–Anxiety scale has been used in cancer populations and has good internal consistency with a Cronbach alpha of greater than 0.89 in English and Spanish (Cella et al., 2010; PROMIS Health Organization, 2012). The composite scores for these measures were converted to z-scores in each trial and used in the current analysis.
Symptom distress: The General Symptom Distress Scale (GSDS) (Badger, Segrin, & Meek, 2011) queries for the presence of 12 symptoms (depression, anxiety, fatigue, shortness of breath, nausea, vomiting, pain, sleep difficulties, bowel problems, difficulty concentrating, loss of appetite, and cough) and the global distress associated with the 12 symptoms on a scale ranging from 1 (not at all distressing) to 10 (extremely distressing). The GSDS has demonstrated good test–retest and internal consistency reliability with a Cronbach alpha of 0.66 or greater (Badger et al., 2011). The total number of symptoms and global distress at baseline were used in these analyses.
Social well-being: Participants’ social and role functioning in home, family, and work settings was measured by the eight-item social well-being subscale of the QOL Instrument–Breast Cancer (Ferrell, Grant, Funk, Otis-Green, & Garcia, 1997). Higher scores reflect greater social well-being, and Cronbach alpha was 0.65 or greater.
Demographic information collected in the baseline interview included age, ethnic origin, level of education, marital status, number of children living at home, income, employment, and family history of cancer. Participants were asked about the presence or absence of seven comorbid conditions (cardiovascular disease, hypertension, diabetes, stroke, arthritis, respiratory problems, other), and a summary count of comorbid conditions was derived. Breast cancer treatment information (yes or no) included surgery and administration of radiation therapy, chemotherapy, and hormonal therapy up until the time of intake into the trials.
Statistical Analysis
The sample characteristics were summarized with the descriptive statistics and summaries of frequency distributions. Group-based growth mixture modeling (GMM) was employed to identify distinct groups of women who followed similar trajectories over time in their scores of depression and anxiety. The trial arm was adjusted for as a covariate in the GMM, and models for depression and anxiety scores were fit separately. Models that contained two to four trajectory groups were tested. To select the number of trajectory groups, Bayesian information criterion (BIC) was used, with the lowest BIC score indicating the best model fit.
Once trajectory-based groups were identified, the distributions of survivor characteristics across these groups were compared using the analysis of variance or chi-squared tests. To determine factors that may be predictive of depression and anxiety trajectories, multinomial logistic regression models with generalized logit link function were fit. Depression or anxiety trajectories were the response variables in these models (one at a time), and selected baseline survivor characteristics were included as explanatory variables. Their selection was based on the Armstrong symptom experience model and literature that identified the associations of these variables with depression and anxiety in breast cancer survivors (Aguado Loi et al., 2013; Armstrong, 2003, 2014; Sammarco & Konecny, 2010). The analyses were performed using SAS, version 9.4, and the latent class mixture model package in R software. [[{"fid":"49336","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Results
Participants
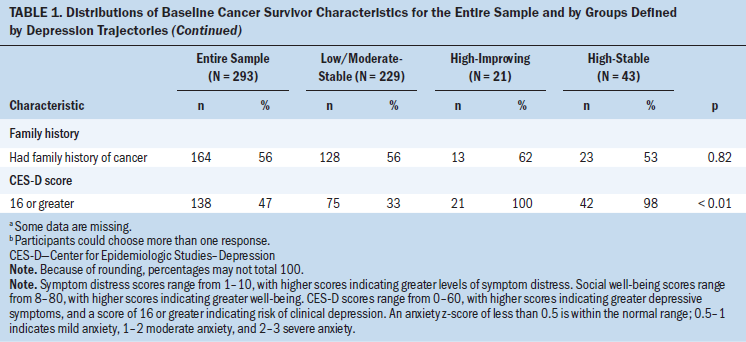
The mean age of the Latina breast cancer survivors was 49 years (SD = 10.7 years); 188 (64%) were married or partnered. Sixty-four percent (n = 188) of the women had less than or a high school education, and 202 (69%) reported a household income of less than $30,000 per year. More than half of the sample was unemployed or disabled because of being too sick to work (see Table 1). At baseline, the mean CES-D score was 17.2 (SD = 12.5), and 47% (n = 138) of the sample scored in the clinically relevant range for elevated risk of depression (CES-D score of 16 or greater). Most women received surgery and chemotherapy and reported an average of four symptoms. 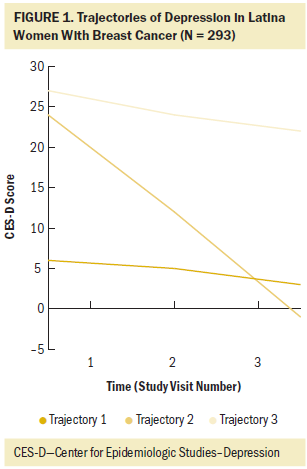
In the GMM analysis, three distinct depression trajectories emerged (see Figures 1 and 2). The majority of women (78%, n = 229) belonged to trajectory 1, which is described by relatively low to moderate depression scores at all three time points. The authors labeled this trajectory “low/moderate-stable.” Of note, about one-third of women in this trajectory had CES-D scores of 16 or higher (see Table 2); therefore, the descriptor low/moderate-stable is only relative to the other two trajectories. About 7% (n = 21) of women belonged to trajectory 2, which is described by the initial high scores that improve at later time points (high-improving). About 15% (n = 43) followed trajectory 3, which is described by high depression scores at all three time points (high-stable). Predictors of depression trajectory group membership included age, social well-being, treatment with chemotherapy, and baseline depression scores (see Table 3). 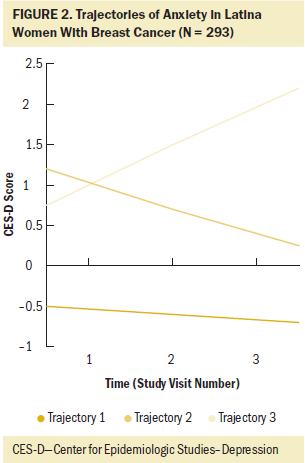
Three distinct trajectories also emerged in the GMM analysis of anxiety. Seventy-three percent (n = 215) of women belonged to trajectory 1, with low-stable anxiety scores over time. This subgroup had average z-scores below 0. Eighteen percent (n = 53) of women followed anxiety trajectory 2, and 9% (n = 25) followed anxiety trajectory 3. Trajectories 2 and 3 began at roughly the same level of one standard deviation above the mean; however, in trajectory 2 anxiety declined (high-improving) and in trajectory 3 anxiety increased (high-worsening). The baseline z-score for anxiety was the only variable significantly associated with anxiety trajectory membership. 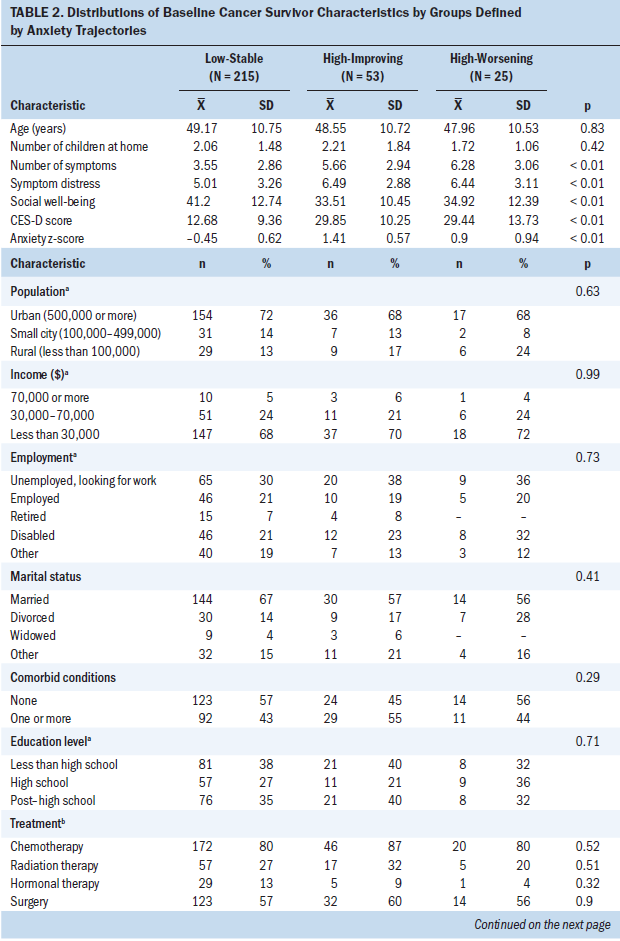
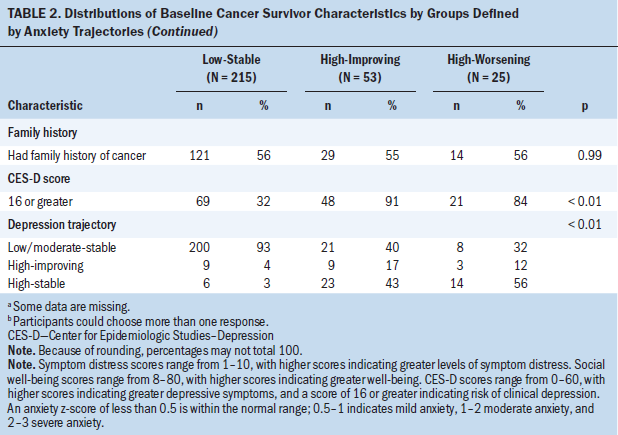
Finally, memberships in subgroups according to depression and anxiety trajectories were strongly associated (phi coefficient = 0.62, p < 0.01), with 200 women or 93% of the low-stable anxiety trajectory also following the low/moderate-stable depression trajectory; however, for those in the high-improving anxiety trajectory, 23 women (43% of those in this trajectory) also belonged to the high-stable depression trajectory that showed no improvement over time. Fourteen women (56%) of the high-worsening anxiety trajectory belonged to the high-stable depression trajectory as well. 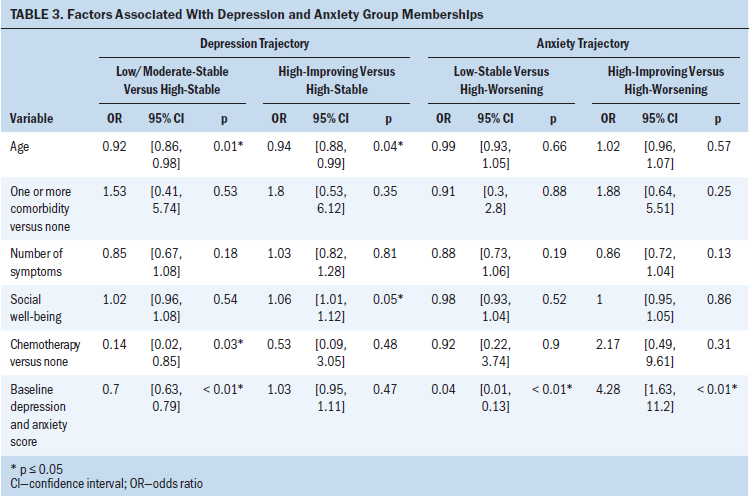
Discussion
To the authors’ knowledge, this is the first large longitudinal study of depression and anxiety in Latina women treated for breast cancer. These findings suggest that depression and anxiety are more common in the current sample of Latina breast cancer survivors than in previously studied samples of NHWs (Krebber et al., 2014). The authors identified three unique trajectories of depression among Latina women with breast cancer.
The majority of Latina women in this study followed a low/moderate-stable depression trajectory, where baseline depression levels were lower compared to the other two trajectories and remained stable over time. These findings are generally consistent with findings from studies of other ethnicities (Donovan, Gonzalez, Small, Andrykowski, & Jacobsen, 2014; Dunn et al., 2011; Kyranou et al., 2014; Stanton et al., 2015). For example, Donovan et al. (2014) found three groups of women with distinct trajectories over the course of 12 months of treatment. One group reported clinically significant symptoms of depression prior to treatment that improved slightly. A second group of women reported subclinical depressive symptoms at the start of treatment that significantly declined over 12 months. The third group of women reported minimal symptoms of depression prior to treatment with a significant decline to an even lower level. By comparison, in the current study, the baseline CES-D score could predict the first depression trajectory, whereas the other two trajectories started with the higher and not statistically different initial score.
In the current study, younger age and higher social well-being were significant predictors in distinguishing subgroups that started high but then improved versus remaining high. These findings are congruent with the current literature documenting that younger women with breast cancer are at higher risk for depression and anxiety (Avis, Levine, Marshall, & Ip, 2017; Janz et al., 2011); however, in the case of depression, social support appears to attenuate the risk for persisting elevated depression levels (Brunault et al., 2016; Luutonen, Vahlberg, Eloranta, Hyväri, & Salminen, 2011). Other studies found that receipt of chemotherapy was associated with greater symptom burden in the post-treatment survivorship period (Ganz, Kwan, Stanton, Bower, & Belin, 2011); in the current sample, receipt of chemotherapy also was predictive of membership in the trajectories with higher levels of depressive symptoms.
Even in trajectory 1, with the lowest mean CES-D over time, about one third of women scored 16 or higher, which is above the established cutoff for clinical relevance. The prevalence of elevated depressive symptoms in the entire sample was 47%, which is substantially higher than the 19% (Avis et al., 2015) previously reported in the breast cancer literature for a predominantly NHW population. This suggests the need for continued research to characterize these symptoms in Latina women, a group that could be considered at higher risk for depression after a breast cancer diagnosis.
In contrast to depression trajectories, the anxiety trajectories could only be predicted by the baseline score, and the differences between pairs of trajectories were not only statistically significant, but also sizable, exceeding half of the standard deviation. Three trajectories for anxiety emerged, with the majority (73%, n = 215) of women falling into the low-stable trajectory. The remaining 27% (n = 78) started at higher levels of anxiety. These results are similar to those reported by Saboonchi et al. (2015), in which the following four specific trajectories of anxiety were identified: high stable, high decrease, mild decrease, and low decrease. One potential explanation for this is that women in the high stable group may have had a difficult time transitioning from active care to surveillance, a time that can be troubling for some women, particularly for those who enter the diagnosis with moderate to high levels of anxiety. The current findings, along with those by Saboonchi et al. (2015), suggest that a substantial proportion of the breast cancer survivor population is in need of interventions to manage anxiety.
The strong associations between depression and anxiety trajectory group membership is consistent with findings of Kyranou at al. (2014), who found higher levels of anxiety to be correlated with elevated depressive symptoms, uncertainty about the future, and lower levels of life satisfaction and life control. In the study by Kyranou et al. (2014), of 396 women with breast cancer, higher preoperative anxiety scores, poorer physical health, decreased sense of control, and more feelings of isolation predicted higher anxiety scores over time (six months postoperatively). In contrast, for the current study, physical health, as reflected by other symptoms and comorbidity, and social well-being were not predictive of the evolution of anxiety over time above the baseline score; however, this difference in findings may be related to the shorter study time period (four versus six months) and the fact that women in the current study were recruited to participate with an informal caregiver, potentially reducing feelings of isolation.
The Latina women in the current sample were significantly younger than the median age for diagnosis of breast cancer in the Unites States (49 years compared to 61 years) (Siegel et al., 2017), and a large percentage reported children living at home. The majority reported household incomes of less than $30,000 per year and a high school education or less. These are all independent risk factors for depression and anxiety in breast cancer survivors. Given these risk factors and the distinct trajectories identified in this analysis, Latina women should be screened for depression and anxiety throughout cancer treatment. Those with elevated depression and anxiety and who are younger and have lower social support should have repeated screening throughout the continuum of care for cancer.
Limitations
Limitations to this study include a relatively narrow timespan of 16 weeks in which follow-up measures were collected. In addition, data for this secondary analysis were compiled from primary intervention studies conducted during a period of eight years and were merged to obtain a database that would support analyses of subgroups. Health insurance could be an important predictor of trajectories but was not available in the database (Costas-Muñiz et al., 2017). The current results may not be generalizable to other Latina breast cancer survivors who would not agree to take part in counseling or educational interventions with an identified cancer support person. Although intervention assignment was controlled for in the trajectory analysis, both interventions received by women could have improved their depression or anxiety and resulted in a higher proportion belonging to the low/moderate-stable and low-stable trajectories for each of these symptoms, respectively. The instrument for anxiety changed in study 3, thereby requiring the computation of a z-score to create a common dataset from studies, which may have limited the interpretation of the results. Finally, clinical characteristics, including disease stage and treatment, were self-reported and not verified in the medical health record.
Implications for Practice
The findings of this study support the American Society of Clinical Oncology’s guidelines for continued screening of psychosocial distress (Andersen, Rowland, & Somerfield, 2015). Higher rates of anxiety and clinically relevant depressive symptomatology (CES-D score of 16 or greater) in this sample suggest the high need for the management of these symptoms among Latina women with breast cancer. Factors such as levels of depression and anxiety at the initial presentation, receipt of chemotherapy treatment, age, and social support may be important targets to use in identifying women at risk for following trajectories that do not improve or worsen over time. Given their roles in assessment and delivery of cancer treatment and supportive care, nurses are ideally situated within the healthcare system to identify women most at risk for developing depression or anxiety and to refer them to psychosocial services. The allocation of available resources then can become more efficient and effective by offering interventions to those most at risk for poor longitudinal trajectories. 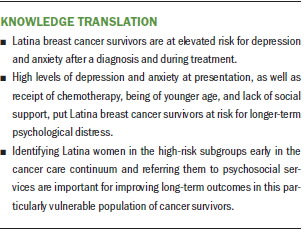
Conclusion
Future research needs to be conducted with Latina survivors who screen positively for high depression and anxiety to provide interventions early in the cancer journey. Studies that evaluate timing, dose, and efficacy of interventions are needed to determine the best intervention to meet individual needs. Moving beyond a one-size-fits-all approach, precision intervention approaches for Latina women with cancer need to be developed to provide individualized person-centered supportive care.
About the Author(s)
Tracy E. Crane, PhD, MS, RDN, is an assistant professor in the College of Nursing at the University of Arizona in Tucson; Terry A. Badger, PhD, RN, PMHCNS-BC, FAAN, is a professor in the College of Nursing and the College of Medicine at the University of Arizona and chair of the Community Health and Systems Health Science Division at the University of Arizona Cancer Center in Tucson; Alla Sikorskii, PhD, is a professor in the Department of Psychiatry and Department of Statistics and Probability at Michigan State University in East Lansing; and Chris Segrin, PhD, is a professor in the College of Social and Behavioral Science, Chiu-Hsieh Hsu, PhD, is a professor in the Mel and Enid Zuckerman College of Public Health, and Anne G. Rosenfeld, PhD, RN, is a professor emerita in the College of Nursing, all at the University of Arizona. This research was funded through a grant (principal investigator [PI]: Badger) from the Livestrong Foundation and grants (PEP-08-300-01 PC1, RSG-12-120-01-CPPB, PI: Badger) from the American Cancer Society. Crane has previously received honorarium from the Shaw Cancer Center, has previously participated on speakers bureaus for the Circuelle Foundation, and has received additional support from NRG Oncology. Badger has previously consulted for the National Cancer Institute, and has received additional support from the American Cancer Society, Merck, and the V Foundation. Crane, Badger, Sikorskii, Segrin, and Rosenfeld contributed to the conceptualization and design, provided the analysis, and contributed to the manuscript preparation. Crane, Badger, and Segrin completed the data collection. Crane, Sikorskii, and Hsu provided statistical support. Crane can be reached at tecrane@email.arizona.edu, with copy to ONFEditor@ons.org. (Submitted June 2018. Accepted October 9, 2018.)
References
Aguado Loi, C.X., Baldwin, J.A., McDermott, R.J., McMillan, S., Martinez Tyson, D., Yampolskaya, S., & VandeWeerd, C. (2013). Risk factors associated with increased depressive symptoms among Latinas diagnosed with breast cancer within 5 years of survivorship. Psycho-Oncology, 22, 2779–2788. https://doi.org/10.1002/pon.3357
Andersen, B.L., Rowland, J.H., & Somerfield, M.R. (2015). Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. Journal of Oncology Practice, 11, 133–134. https://doi.org/10.1200/JOP.2014.002311
Armstrong, T.S. (2003). Symptoms experience: A concept analysis. Oncology Nursing Forum, 30, 601–606. https://doi.org/10.1188/03.ONF.601-606
Armstrong, T.S. (2014). 2013 special topics conference: Peaks and pitfalls in longitudinal studies of symptom outcome data. Nursing Outlook, 62, 305–312. https://doi.org/10.1016/j.outlook.2014.05.005
Ashing-Giwa, K., Rosales, M., Lai, L., & Weitzel, J. (2013). Depressive symptomatology among Latina breast cancer survivors. Psycho-Oncology, 22, 845–853. https://doi.org/10.1002/pon.3084
Ashing-Giwa, K.T., Tejero, J.S., Kim, J., Padilla, G.V., & Hellemann, G. (2007). Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma. Quality of Life Research, 16, 413–428. https://doi.org/10.1007/s11136-006-9138-4
Avis, N.E., Levine, B., Marshall, S.A., & Ip, E.H. (2017). Longitudinal examination of symptom profiles among breast cancer survivors. Journal of Pain and Symptom Management, 53, 703–710. https://doi.org/10.1016/j.jpainsymman.2016.10.366
Avis, N.E., Levine, B.J., Case, L.D., Naftalis, E.Z., & Van Zee, K.J. (2015). Trajectories of depressive symptoms following breast cancer diagnosis. Cancer Epidemiology, Biomarkers and Prevention, 24, 1789–1795. https://doi.org/10.1158/1055-9965.EPI-15-0327
Badger, T., Segrin, C., Dorros, S.M., Meek, P., & Lopez, A.M. (2007). Depression and anxiety in women with breast cancer and their partners. Nursing Research, 56, 44–53.
Badger, T.A., Segrin, C., Hepworth, J.T., Pasvogel, A., Weihs, K., & Lopez, A.M. (2013). Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psycho-Oncology, 22, 1035–1042. https://doi.org/10.1002/pon.3101
Badger, T.A., Segrin, C., & Meek, P. (2011). Development and validation of an instrument for rapidly assessing symptoms: The general symptom distress scale. Journal of Pain and Symptom Management, 41, 535–548. https://doi.org/10.1016/j.jpainsymman.2010.06.011
Brunault, P., Champagne, A.L., Huguet, G., Suzanne, I., Senon, J.L., Body, G., . . . Camus, V. (2016). Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non-metastatic breast cancer patients. Psycho-Oncology, 25, 513–520. https://doi.org/10.1002/pon.3947
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., . . . Hays, R. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63, 1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011
Costas-Muñiz, R., Hunter-Hernández, M., Garduño-Ortega, O., Morales-Cruz, J., & Gany, F. (2017). Ethnic differences in psychosocial service use among non-Latina white and Latina breast cancer survivors. Journal of Psychosocial Oncology, 35, 424–437. https://doi.org/10.1080/07347332.2017.1310167
Donovan, K.A., Gonzalez, B.D., Small, B.J., Andrykowski, M.A., & Jacobsen, P.B. (2014). Depressive symptom trajectories during and after adjuvant treatment for breast cancer. Annals of Behavioral Medicine, 47, 292–302. https://doi.org/10.1007/s12160-013-9550-2
Dunn, L.B., Cooper, B.A., Neuhaus, J., West, C., Paul, S., Aouizerat, B., . . . Miaskowski, C. (2011). Identification of distinct depressive symptom trajectories in women following surgery for breast cancer. Health Psychology, 30, 683–692. https://doi.org/10.1037/a0024366
Ell, K., Xie, B., Wells, A., Nedjat-Haiem, F., Lee, P.J., & Vourlekis, B. (2008). Economic stress among low-income women with cancer: Effects on quality of life. Cancer, 112, 616–625. https://doi.org/10.1002/cncr.23203
Ennis, S.R., Rios-Vargas, & Albert, N.G. (2011). The Hispanic population: 2010. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf
Eversley, R., Estrin, D., Dibble, S., Wardlaw, L., Pedrosa, M., & Favila-Penney, W. (2005). Post-treatment symptoms among ethnic minority breast cancer survivors. Oncology Nursing Forum, 32, 250–256. https://doi.org/10.1188/05.ONF.250-256
Fann, J.R., Thomas-Rich, A.M., Katon, W.J., Cowley, D., Pepping, M., McGregor, B.A., & Gralow, J. (2008). Major depression after breast cancer: A review of epidemiology and treatment. General Hospital Psychiatry, 30, 112–126. https://doi.org/10.1016/j.genhosppsych.2007.10.008
Ferrell, B.R., Grant, M., Funk, B., Otis-Green, S., & Garcia, N. (1997). Quality of life in breast cancer. Part I: Physical and social well-being. Cancer Nursing, 20, 398–408. https://doi.org/10.1097/00002820-199712000-00003
Fu, O.S., Crew, K.D., Jacobson, J.S., Greenlee, H., Yu, G., Campbell, J., . . . Hershman, D.L. (2009). Ethnicity and persistent symptom burden in breast cancer survivors. Journal of Cancer Survivorship, 3, 241–250. https://doi.org/10.1007/s11764-009-0100-7
Ganz, P.A., Desmond, K.A., Leedham, B., Rowland, J.H., Meyerowitz, B.E., & Belin, T.R. (2002). Quality of life in long-term, disease-free survivors of breast cancer: A follow-up study. Journal of the National Cancer Institute, 94, 39–49.
Ganz, P.A., Kwan, L., Stanton, A.L., Bower, J.E., & Belin, T.R. (2011). Physical and psychosocial recovery in the year after primary treatment of breast cancer. Journal of Clinical Oncology, 29, 1101–1109. https://doi.org/10.1200/JCO.2010.28.8043
Giese-Davis, J., Collie, K., Rancourt, K.M., Neri, E., Kraemer, H.C., & Spiegel, D. (2011). Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: A secondary analysis. Journal of Clinical Oncology, 29, 413–420. https://doi.org/10.1200/JCO.2010.28.4455
Hann, D., Winter, K., & Jacobsen, P. (1999). Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychosomatic Research, 46, 437–443.
Holden, A.E., Ramirez, A.G., & Gallion, K. (2014). Depressive symptoms in Latina breast cancer survivors: A barrier to cancer screening. Health Psychology, 33, 242–248. https://doi.org/10.1037/a0032685
Jacobsen, P.B., & Jim, H.S. (2008). Psychosocial interventions for anxiety and depression in adult cancer patients: Achievements and challenges. CA: A Cancer Journal for Clinicians, 58, 214–230. https://doi.org/10.3322/CA.2008.0003
Janz, N.K., Friese, C.R., Li, Y., Graff, J.J., Hamilton, A.S., & Hawley, S.T. (2014). Emotional well-being years post-treatment for breast cancer: Prospective, multi-ethnic, and population-based analysis. Journal of Cancer Survivorship, 8, 131–142. https://doi.org/10.1007/s11764-013-0309-3
Janz, N.K., Hawley, S.T., Mujahid, M.S., Griggs, J.J., Alderman, A., Hamilton, A.S., . . . Katz, S.J. (2011). Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer, 117, 1827–1836. https://doi.org/10.1002/cncr.25740
Krebber, A.M., Buffart, L.M., Kleijn, G., Riepma, I.C., de Bree, R., Leemans, C.R., . . . Verdonck-de Leeuw, I.M. (2014). Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology, 23, 121–130. https://doi.org/10.1002/pon.3409
Kyranou, M., Puntillo, K., Dunn, L.B., Aouizerat, B.E., Paul, S.M., Cooper, B.A., . . . Miaskowski, C. (2014). Predictors of initial levels and trajectories of anxiety in women before and for 6 months after breast cancer surgery. Cancer Nursing, 37, 406–417. https://doi.org/10.1097/NCC.0000000000000131
Liu, L., Mills, P.J., Rissling, M., Fiorentino, L., Natarajan, L., Dimsdale, J.E., . . . Ancoli-Israel, S. (2012). Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain, Behavior, and Immunity, 26, 706–713. https://doi.org/10.1016/j.bbi.2012.02.001
Luutonen, S., Vahlberg, T., Eloranta, S., Hyväri, H., & Salminen, E. (2011). Breast cancer patients receiving postoperative radiotherapy: Distress, depressive symptoms and unmet needs of psychosocial support. Radiotherapy and Oncology, 100, 299–303. https://doi.org/10.1016/j.radonc.2011.01.014
Petronis, V.M., Carver, C.S., Antoni, M.H., & Weiss, S. (2003). Investment in body image and psychosocial well-being among women treated for early stage breast cancer: Partial replication and extension. Psychology and Health, 18, 1–13. https://doi.org/10.1080/0887044021000020941
PROMIS Health Organization. (2012). PROMIS item bank v1.0: Emotional distress—Anxiety short form 8a. Retrieved from http://www.healthmeasures.net/administrator/components/com_instruments/…
Radloff, L.S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Saboonchi, F., Petersson, L.M., Wennman-Larsen, A., Alexanderson, K., & Vaez, M. (2015). Trajectories of anxiety among women with breast cancer: A proxy for adjustments from acute to transitional survivorship. Journal of Psychosocial Oncology, 33, 603–619. https://doi.org/10.1080/07347332.2015.1082165
Sammarco, A., & Konecny, L.M. (2010). Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: A comparative study. Oncology Nursing Forum, 37, 93–99. https://doi.org/10.1188/10.ONF.93-99
Segrin, C., Badger, T.A., Meek, P., Lopez, A.M., Bonham, E., & Sieger, A. (2005). Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. Journal of Social and Personal Relationships, 22, 673–689. https://doi.org/10.1177/0265407505056443
Siegel, R.L., Miller, K.D., & Jemal, A. (2017). Cancer statistics, 2017. CA: A Cancer Journal for Clinicians, 67, 7–30. https://doi.org/10.3322/caac.21387
Spencer, S.M., Lehman, J.M., Wynings, C., Arena, P., Carver, C.S., Antoni, M.H., . . . Love, N. (1999). Concerns about breast cancer and relations to psychosocial well-being in a multiethnic sample of early-stage patients. Health Psychology, 18, 159–168.
Spiegel, D., Giese-Davis, J., Taylor, C.B., & Kraemer, H. (2006). Stress sensitivity in metastatic breast cancer: Analysis of hypothalamic-pituitary-adrenal axis function. Psychoneuroendocrinology, 31, 1231–1244.
Spielberger, C.D., Gorsuch, R.L., Lushene, R., Vagg, P.P., & Jacobs, G.A. (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press.
Spielberger, C.D., Gorsuch, R.L., & Lushene, R.E. (1982). STAI: Manual for the State-Trait Anxiety Inventory (self evaluation questionnaire) [Article in Spanish]. Madrid, Spain: TEA Ediciones.
Stanton, A.L., Wiley, J.F., Krull, J.L., Crespi, C.M., Hammen, C., Allen, J.J., . . . Weihs, K.L. (2015). Depressive episodes, symptoms, and trajectories in women recently diagnosed with breast cancer. Breast Cancer Research and Treatment, 154, 105–115.
Yanez, B., Thompson, E.H., & Stanton, A.L. (2011). Quality of life among Latina breast cancer patients: A systematic review of the literature. Journal of Cancer Survivorship, 5, 191–207. https://doi.org/10.1007/s11764-011-0171-0




