Self-Management Support in Patients With Incurable Cancer: How Confident Are Nurses?
Objectives: To explore how nurses perceive their self-efficacy and performance in supporting self-management among patients with incurable cancer, and whether these perceptions differ between community and hospital nurses.
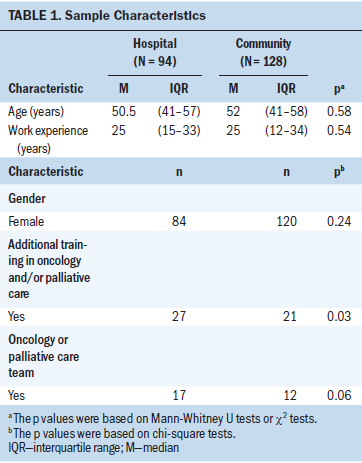
Sample & Setting: 222 hospital nurses (n = 94) and community nurses (n = 128) working with adult patients with incurable cancer.
Methods & Variables: An online survey included the Self-Efficacy and Performance Into Self-Management Support instrument. Possible differences in age, gender, work setting, and additional training in oncology between groups were explored.
Results: Nurses felt confident about their self-efficacy, particularly in assessing patients’ knowledge and beliefs and in advising about their disease and health status. Nurses felt less confident in their performance, particularly in the use of technology (arranging follow-up care), but also in agreeing on collaborative goals and assisting patients in achieving these goals. Compared to hospital nurses, community nurses reported significantly higher scores on self-efficacy and performance.
Implications for Nursing: More effort is needed to increase nurses’ confidence in providing self-management support, with a focus on arranging follow-up care with the use of technology and on collaborating with patients in setting and achieving goals.
Jump to a section
Living with incurable cancer can have devastating effects on psychological, social, physical, economic, and cultural aspects of a person’s life (Johnston et al., 2009; Lin & Bauer-Wu, 2003). Patients with incurable cancer must cope with life-limiting, changing conditions, as well as the consequences of the disease and treatment in daily life (Khan, Mant, Carpenter, Forman, & Rose, 2011; Lenihan, Oliva, Chow, & Cardinale, 2013; Lin & Bauer-Wu, 2003; Schulman-Green et al., 2011). Assisting with self-management might help patients deal with these consequences, improve problem-solving skills, and prepare for death (Johnston, Milligan, Foster, & Kearney, 2012; McCorkle et al., 2011; Tocchi, McCorkle, & Knobf, 2015).
Self-management can be described as a person’s ability to manage physical and psychosocial symptoms and to make decisions concerning treatment and/or care to integrate the disease as well as possible into daily life and to maintain a satisfactory quality of life despite the disease (Barlow, Wright, Sheasby, Turner, & Hainsworth, 2002; Bodenheimer, Lorig, Holman, & Grumbach, 2002). At the end of life, self-management focuses on “living with dying”; activities are likely to be beneficial if focused on symptoms or impending death and directed toward emotional and psychological adjustment to the incurable illness. For instance, activities can focus on how to deal with fatigue or pain, how to plan important moments or daily care, and how to rest in between these moments. In addition, changes in personal (physical, emotional, or social) or care aspects (cancer status, treatment, or palliative phase) prompt changes in self-management(Schulman-Green et al., 2011). Support should acknowledge these possible transitions and be directed toward present and future care needs, quality of life, and other outcomes identified by patients as necessary for self-management (Landier, 2009; Noonan et al., 2017; Schulman-Green et al., 2011).
Literature Review
Self-management support acknowledges patients’ central role in their own care, fostering a sense of responsibility for their own health (Battersby et al., 2010). It uses proven programs that provide adequate information about actual or potential problems, emotional support, and strategies for living with a chronic illness that enable patients to care for themselves in a way they prefer (McCorkle et al., 2011; Schulman-Green et al., 2012). Using a collaborative approach, providers and patients work together to assess problems, set priorities, establish goals, create treatment plans, and solve problems (Von Korff, Gruman, Schaefer, Curry, & Wagner, 1997). The role of nurses in supporting self-management in patients with incurable cancer is important (Johnston et al., 2009), and it requires a range of educational, supportive, and communicational competencies (Elissen et al., 2013; Sahlsten, Larsson, Sjöström, Lindencrona, & Plos, 2007). These competencies can be distinguished by the phases of the 5 As model, which include the following (Glasgow, Davis, Funnell, & Beck, 2003; van Hooft, Dwarswaard, Bal, Strating, & van Staa, 2016):
• Assessing the patient’s knowledge, beliefs, and behaviors
• Advising the patient by providing specific information about the disease and information about the patient’s health status in an understandable manner so that patients can relate their self-management skills and behaviors to their health status
• Agreeing on goals collaboratively set with the patient and according to the patient’s priorities
• Assisting the patient by identifying and resolving barriers that make it difficult for the patient to achieve the goals set
• Arranging follow-up (such as by email or telephone)
The 5 As are interrelated and provide a structure for self-management support (Glasgow et al., 2003).
A precondition for performing self-management support activities is self-efficacy—the confidence a person has in his or her skills and perceived ability to perform the behavior (Bandura, 1977). Self-efficacy as perceived by nurses can be an indicator for the activities they perform; more confidence in skills (e.g., using technology) is a predictor of choices and behavior (e.g., applying technology) (Bandura, 1991). A study with 598 respondents revealed a discrepancy between higher reported self-efficacy and lower reported performance of self-management support activities in a general nursing population (van Hooft et al., 2016). This discrepancy increased in the subsequent phases of the 5 As model, with larger differences between self-efficacy and performance in the Agree, Assist, and Arrange phases (Duprez et al., 2016; van Hooft et al., 2016). Nurses seem to focus mainly on assessment of background (Assess) and advice and information (Advise) (Duprez et al., 2016; van Hooft et al., 2016); whereby such advice seems restricted to physical problems and psychological problems and receives less attention (Been-Dahmen, Dwarswaard, Hazes, van Staa, & Ista, 2015; Ventura, Burney, Brooker, Fletcher, & Ricciardelli, 2014). Activities in the Agree, Assist, and Arrange phases seem to be limited, although these aspects are essential in self-management support (Elissen et al., 2013; Slev et al., 2017).
Studies using the 5 As model reported inconsistencies regarding self-management support in patients with chronic illnesses (Duprez, Vandecasteele, Verhaeghe, Beeckman, & Van Hecke, 2017; van Hooft et al., 2016). However, knowledge about nurses supporting self-management in people with incurable cancer is still limited. Several studies have suggested that setting and additional training (e.g., in oncology) improve the provision of self-management support (Faithfull, Samuel, Lemanska, Warnock, & Greenfield, 2016; Griffiths, Simon, Richardson, & Corner, 2013), which is based on the perceptions of nurses or patients. As a result, the current authors expected that nurses caring for patients with incurable cancer would perceive their self-efficacy and subsequent performance as better than nurses caring for patients with chronic conditions. The first aim of the current study was to explore how nurses perceived their self-efficacy and performance in supporting self-management activities in patients with incurable cancer.
In addition, in the Netherlands, the role of nurses in supporting self-management is currently emphasized more for community nurses than for hospital nurses, who focus more on medical treatment (van Hooft et al., 2016). The authors hypothesized that community nurses would have more positive perceptions about their self-efficacy and performance and their support of self-management in the subsequent phases of the 5 As model. The second aim of the study was to determine to what extent the setting (community versus hospital) affected nurses’ perceived self-management support for patients with incurable cancer.
Methods
Design and Ethical Approval
In June 2016, the authors conducted a cross-sectional quantitative study among nurses using an online questionnaire. For such a study, Dutch legislation (Medical Research Involving Human Subjects Act) does not require ethical approval by a medical ethics committee. Study participation was voluntary, and participant consent was assumed upon return of completed questionnaires. The questionnaire data were stored and analyzed anonymously, in accordance with the Dutch Personal Data Protection Act.
Study Population
Nurses working in hospitals or the community were selected from a preexisting research sample, the Nursing Staff Panel. This panel consists of a nationwide representative sample of nursing staff members working in various healthcare sectors. Members of the Nursing Staff Panel are mainly recruited via Dutch employee insurance agencies (with which every healthcare employee is registered). All participants of the Nursing Staff Panel agree to complete questionnaires about issues in nursing on a regular basis (at least twice a year). To recruit participants for this study, the authors sent an email with information about the aim and content of the survey, as well as a link to the questionnaire, to members of the Nursing Staff Panel (n = 692) who worked as RNs in the community or at a general or university hospital. One or two email reminders were sent to nonresponders after one and three weeks to improve the response rate. No incentives were provided. After entering the online site, potential participants answered study-specific questions about age, gender, work experience, work setting, and additional training in oncology. If they stated that they had provided care to adult patients with incurable cancer in the past 12 months, they were invited to complete the questionnaire and were included.
Instrument
The primary outcome was a quantification of nurses’ self-efficacy and performance in providing self-management support. The authors used the validated Self-Efficacy and Performance Into Self-Management Support (SEPSS) instrument, Dutch version (Duprez et al., 2016). SEPPS consists of six subscales, which are based on the 5 As model (Assess, Advise, Agree, Assist, and Arrange) and a subscale that addresses the overall competencies that are necessary in each step of the model, such as respecting the cultural background of the patient, reflecting on their own performance, and recognizing ethical dilemmas (Duprez et al., 2016). Each subscale of the SEPSS contains six items (a total of 36 items). Self-efficacy, defined as the nurse’s belief in his or her ability to perform a specific behavior (i.e., self-management support) was assessed with the statement “I can do this,” which was rated on a five-point Likert-type scale ranging from 0 (not at all) to 4 (good). Performance (i.e., the actual behavior) was assessed with the statement “I do this,” which was rated on a five-point Likert-type scale ranging from 0 (never) to 4 (always). In the final section, nurses could add free-form text about their needs in terms of improving self-management support for patients with incurable cancer.
In previous studies, the Cronbach alpha was 0.96 for self-efficacy and 0.95 for behavior, respectively (Duprez et al., 2016; van Hooft et al., 2016). In the current study, the Cronbach alpha was 0.96 for both self-efficacy and performance.
Analysis
Data were screened for repetitive response patterns, and questionnaires with less than 10% variation in answers (i.e., identical answers to at least 64 out of 72 items) were excluded from further analysis. In addition, data were screened for missing subscale scores (all subscales were complete).
Descriptive analyses were used for summarizing demographic characteristics of nurses, including age (years), gender (male or female), work experience (years), additional training in oncology (yes or no), and setting (community or hospital).
To determine perceived self-efficacy and performance, the authors computed sum scores for each of the subscales, as well as average sum scores for self-efficacy and performance (range 0–4, indicating not at all or never to good or always). Because the scores on the SEPSS subscales were not normally distributed, nonparametric presentation (median scores with interquartile ranges [IQRs]) and analyses were used to present the scores.
Differences between perceived self-efficacy and performance in each group were calculated with Wilcoxon tests, and differences between community and hospital nurses were calculated using Mann-Whitney U tests. Linear regression analyses were used to estimate the differences in self-efficacy and performance that were associated with the setting (community or hospital). Because age and work experience were correlated (Pearson correlation coefficient = 0.83), only age was included in the model.
All statistical analyses were performed with IBM SPSS Statistics, version 22.0. A p value of less than 0.05 was considered statistically significant.
Results
A total of 334 members of the Nursing Staff Panel returned the questionnaire (response rate = 48%). Of these, 234 had cared for adult patients with incurable cancer in the previous 12 months. Twelve questionnaires were excluded from analysis, mainly because of repetitive or absent responses. Of 222 questionnaires that were included in the analysis, most were completed by female nurses with a median age of 51 years and median work experience of 25 years (see Table 1). Responders were older than nonresponders (median of 52 and 42 years, respectively, p < 0.001) and had more work experience (median of 25 and 16 years, respectively, p < 0.001). No significant difference in gender was noted between responders and nonresponders.
Self-Efficacy in Self-Management Support
The overall median score for self-efficacy in self-management support was 2.8 (IQR = 2.5–3.1) (see Table 2), which was considered almost sufficient, based on the response categories ranging from 0 (not at all) to 4 (good). With respect to the subscales, nurses perceived their self-efficacy as sufficient (median = 3) in “assessing patients’ knowledge and belief,” “advising about disease and health status,” and the subscale “overall competencies.” The remaining subscales were perceived as almost sufficient.
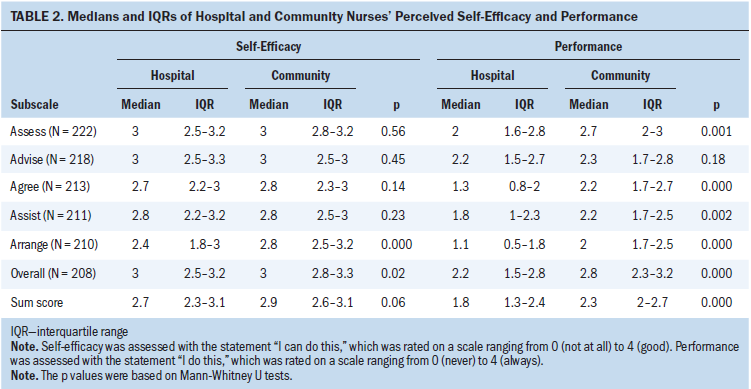
When focusing on single items, nurses felt least confident with using assistive devices and technology (i.e., e-health) to provide remote guidance (median = 1, indicating not sufficient) and discussing with patients how they can use self-management assistive devices (e.g., a diary) in their daily activities (median = 2, indicating more or less competent).
Performance of Self-Management Support
The overall median score on performing self-management support was 2.1 (IQR = 1.7–2.6), which was considered as occasional performance (response categories ranged from 0 [never] to 4 [always]). With respect to the subscales, nurses reported occasional to frequent performance in overall competencies (median = 2.7), assessing patients’ knowledge and beliefs (median = 2.3), and advising (median = 2.2). Nurses reported that they rarely to occasionally arranged follow-up care by email or telephone (median = 1.8). They also reported that they never used assistive devices and technology to provide remote guidance to the patient (median = 0), rarely discussed how patients could use self-management assistive devices in their daily activities (median = 1), and rarely discussed with patients who they will inform about their condition (median = 1).
Comparison of Community and Hospital Nurses
Nurses working in the community perceived their self-efficacy in the Arrange phase as higher than nurses working in hospitals (median values = 2.8 and 2.4, respectively, p < 0.001). This indicates that community nurses felt more confident in their ability to arrange follow-up contact. After adjusting for gender, age, and additional training, the authors found that community nurses still perceived their self-efficacy in self-management support as higher than hospital nurses (estimated difference = 0.18, 95% confidence interval [CI] [0.04, 0.37], p = 0.01) (see Table 3).
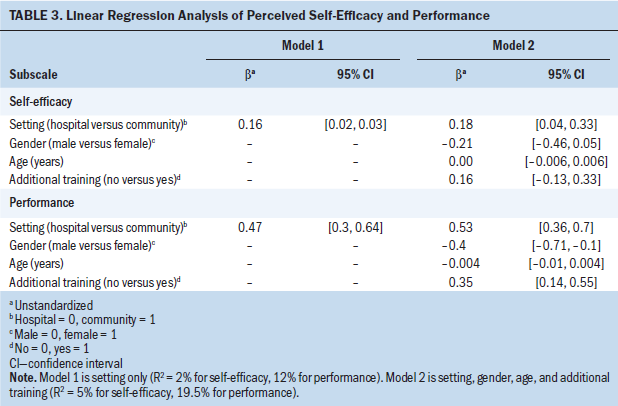
Considering perceived performance, community nurses had significantly higher median scores in four out of five subscales of the 5 As model; the subscale Advise was the only one in which no significant differences were found in perceived performance. After adjusting for gender, age, and additional training, the authors found that community nurses still perceived their performance as higher than hospital nurses (estimated difference = 0.53, 95% CI [0.36, 0.7], p < 0.001). Male gender and additional training also made a statistically significant contribution (estimated differences = 0.4 and 0.35, respectively).
Community and hospitals nurses perceived their self-efficacy as higher than their performance. All differences between self-efficacy and performance in the subsequent subscales were statistically significant.
Discussion
Community nurses and hospital nurses reported occasionally performing self-management support activities in patients with incurable cancer and reported their self-efficacy as almost sufficient. Community nurses reported an average of 0.5 points higher in performance (on a five-point Likert-type scale) than hospital nurses, particularly in the phases of assessing, agreeing on goals, and arranging follow-up contact. They also reported 0.2 points higher in self-efficacy.
The self-reported performance and self-efficacy reveal deficits in the self-management support provided by nurses. Self-management support for patients with incurable cancer seems comparable to that given to patients in general. Other studies using SEPSS among university hospital nurses (van Hooft et al., 2016) or nurses (including students) from various settings (Duprez et al., 2016) revealed comparable results for self-efficacy. However, in terms of performance, the current results are 0.4 points higher than those in other studies, mainly because of more self-management activities performed by community nurses.
More hospital nurses had additional training in oncology; however, they reported lower self-efficacyand performance. One study suggested that inadequate preparation of student nurses hampers transferring theory of self-management support into practice, as well as a lack of role models and hours of training to increase self-confidence; the study did not include additional training (van Hooft, Becqué, Dwarswaard, van Staa, & Bal, 2018). Another study suggested that the perceived difference between performance (occasional) and self-efficacy (sufficient) is influenced by knowledge about self-management support, role conflict, lack of engagement, and time (Faithfull et al., 2016; Tocchi et al., 2015; van Hooft et al., 2016). As a result, both initial and additional training should focus not only on medical management and knowledge of medical management, but also on self-management skills and techniques, as well as collaborative and proactive care planning together with the patient (Faithfull et al., 2016; van Hooft et al., 2018).
The 10% higher scores of community nurses confirm the current authors’ hypothesis that these professionals apply self-management support in patients with incurable cancer more often than hospital nurses (van Hooft et al., 2016). In community care, self-management support takes place in the social context of the patient. Community nurses have stronger coordination skills and knowledge of other healthcare providers and services. These competencies might explain the difference between community and hospital nurses in the phases Agree, Assist, and Arrange of the 5 As model. In particular, hospital nurses did not feel sufficiently confident in arranging follow-up care and hardly ever performed this task.
In patients with incurable cancer, hospital and community nurses felt most confident in assessing patient knowledge, beliefs, and behavior and in advising patients about the disease and health status. This is in line with other studies in cancer and chronic care, which concluded that self-management support focuses primarily on personal situations and wishes (Assess) and medical management and treatment compliance (Advise) (Elissen et al., 2013; Ercolano et al., 2016; Slev et al., 2017; Ter Maten-Speksnijder, Dwarswaard, Meurs, & van Staa, 2016). Other aspects, such as managing psychosocial problems or planning and documenting care (Agree), are not carried out by nurses (Ausserhofer et al., 2014; Slev et al., 2017). From the provider’s perspective, coaching skills, which are necessary throughout all phases, are used to a lesser extent (Ter Maten-Speksnijder et al., 2016). Activities for which the required time and effort are difficult to estimate, such as talking to patients or educating patients and families, are more often omitted and seem to receive the lowest priority (Ausserhofer et al., 2014). The lowest scores were found for arranging follow-up care (Arrange); nurses hardly initiate or facilitate follow-up care with patients prior to discharge. In nurse education, less attention is given to this aspect (van Hooft et al., 2018). In addition, in some hospitals, follow-up care is arranged by transferring nurses or case managers, which might have contributed to the low scores on the items.
Scores for single items revealed that assistive devices and technology are hardly ever used by community or hospital nurses. Technology may provide opportunities for nurses (related to symptom management, patient education, or training interventions) (Knobf, 2013; Tocchi et al., 2015). In an online focus-group study, nurses expressed a positive attitude toward technology (Slev et al., 2017). However, one study reported that nurses and nursing students do not feel self-competent about using technology (van Houwelingen, 2018; van Houwelingen, Ettema, Kort, & ten Cate, 2017). In addition, technology may not be available in everyday practice, and nurses may not have time to learn about applying technology in patient care. More people are becoming familiar with assistive devices (Knobf, 2013), and technology provides opportunities for self-management support. In people with cancer, technologic applications positively affect perceived support, knowledge levels, and information competence (Hoek, Schers, Bronkhorst, Vissers, & Hasselaar, 2017; Slev et al., 2016). Future training should focus on competencies and the possibilities for using technology for supporting self-management in patients with incurable cancer.
Limitations
The data in this study reflect nurses’ self-reported perceptions of their self-management support for patients with incurable cancer. These perceptions might not reflect their actual performance. Additional observations may provide a better picture of the actual self-management support.
The response rate was fair (48%) but not high enough to eliminate the risk of selection bias. It may represent an underestimate of the actual response rate of eligible nurses. Nurses may have moved or changed positions in recent months and, consequently, had not been providing care to patients with incurable cancer. Some mentioned this upon returning the survey; others may not have responded for this reason.
In addition, the authors could not include the educational background of nurses in the analysis. The information about education among the Nursing Staff Panel members is continuously changing because of job rotation and professional development. Not all changes are communicated; as a result, the authors decided not to include this variable.
The SEPPS instrument was limited in that it focuses on self-management support of patients; questions do not include informal caregivers. The latter are crucial in the support of patients with advanced cancer; they may experience psychosocial burdens, strain, or distress (Girgis, Lambert, Johnson, Waller, & Currow, 2013), and they need support in terms of information, what to expect, and how to manage consequences in daily care (Johnston et al., 2012).
Implications for Nursing
The findings of this study indicate that more effort is needed to increase nurses’ confidence in supporting self-management. Nurses are not confident in agreeing on goals set collaboratively, in assisting patients in achieving these goals, and in arranging follow-up care. Integrating the 5 As model in training and in team practice is recommended, with emphasis on the phases Agree, Assist, and Arrange. In addition, specific attention should be given to the use of devices and technology, for which nurses reported a lack of knowledge and a lack of time to learn about.
Future research should focus on developing and evaluating training programs for self-management support skills in nurses and, more specifically, on collaborating with patients in care planning and coaching. In addition, studies should examine preferences and possibilities of applying technology in patients with incurable cancer, from both a nursing and a patient perspective, in hospital and community care. They should also explore the relationship between nurses’ self-efficacy to support self-management and patients’ self-efficacy to perform it.
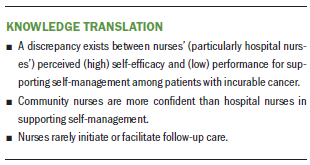
Conclusion
This cross-sectional study found a discrepancy between nurses’ (particularly hospital nurses’) perceived (high) self-efficacy and (lower) performance for supporting self-management among patients with incurable cancer. Community nurses were more confident than hospital nurses in supporting self-management in this population. More effort is needed to increase self-management support by nurses, with a focus on arranging follow-up care and use of technology.
About the Author(s)
Irene P. Jongerden, PhD, RN, is a senior researcher and Vina N. Slev, MSc, is a PhD candidate in the Center of Expertise in Palliative Care, both in the Department of Occupational and Public Health at the VU University Medical Center in Amsterdam, Netherlands; Susanne M. van Hooft, PhD, RN, is a researcher in the Research Centre Innovations in Care at the Rotterdam University of Applied Sciences in the Netherlands; H. Roeline Pasman, PhD, is an associate professor in the Department of Occupational and Public Health and Irma M. Verdonck-de Leeuw, PhD, is a professor of psychosocial oncology in the Department of Clinical, Neuro and Developmental Psychology, both at the VU University Medical Center; Anke J.E. de Veer, PhD, is a senior researcher at the Netherlands Institute for Health Services Research in Utrecht; Cornelia F. van Uden-Kraan, PhD, is a senior researcher in the Department of Clinical, Neuro and Developmental Psychology at the VU University Medical Center; and Anneke L. Francke, PhD, is a professor at the Netherlands Institute for Health Services Research. This research was funded by a grant (520002001) from the Netherlands Organisation for Health Research and Development. Verdonck-de Leeuw has previously received support from Achmea, Bristol-Myers Squibb, Danone Nutricia, Redkite, and Zilveren Kruis. Jongerden, Slev, van Hooft, Verdonck-de Leeuw, van Uden-Kraan, and Francke contributed to the conceptualization and design. Slev, de Veer, and van Uden-Kraan completed the data collection. Jongerden, Slev, and van Uden-Kraan provided statistical support. Jongerden, Slev, van Hooft, Pasman, van Uden-Kraan, and Francke provided the analysis. Jongerden and Slev contributed equally to the manuscript. All authors contributed to the manuscript preparation. Jongerden can be reached at i.jongerden@vumc.nl, with copy to ONFEditor@ons.org. (Submitted May 2018. Accepted August 1, 2018.)
References
Ausserhofer, D., Zander, B., Busse, R., Schubert, M., De Geest, S., Rafferty, A.M., . . . Schwendimann, R. (2014). Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross-sectional RN4CAST study. BMJ Quality and Safety, 23, 126–135. https://doi.org/10.1136/bmjqs-2013-002318
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215.
Bandura, A. (1991). Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes, 50, 248–287. https://doi.org/10.1016/0749-5978(91)90022-L
Barlow, J., Wright, C., Sheasby, J., Turner, A., & Hainsworth, J. (2002). Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling, 48, 177–187.
Battersby, M., Von Korff, M., Schaefer, J., Davis, C., Ludman, E., Greene, S.M., . . . Wagner, E.H. (2010). Twelve evidence-based principles for implementing self-management support in primary care. Joint Commission Journal on Quality and Patient Safety, 36, 561–570.
Been-Dahmen, J.M.J., Dwarswaard, J., Hazes, J.M.W., van Staa, A., & Ista, E. (2015). Nurses’ views on patient self-management: A qualitative study. Journal of Advanced Nursing, 71, 2834–2845. https://doi.org/10.1111/jan.12767
Bodenheimer, T., Lorig, K., Holman, H., & Grumbach, K. (2002). Patient self-management of chronic disease in primary care. JAMA, 288, 2469–2475.
Duprez, V., Van Hooft, S.M., Dwarswaard, J., van Staa, A., Van Hecke, A., & Strating, M.M.H. (2016). The development and psychometric validation of the self-efficacy and performance in self-management support (SEPSS) instrument. Journal of Advanced Nursing, 72, 1381–1395. https://doi.org/10.1111/jan.12918
Duprez, V., Vandecasteele, T., Verhaeghe, S., Beeckman, D., & Van Hecke, A. (2017). The effectiveness of interventions to enhance self-management support competencies in the nursing profession: A systematic review. Journal of Advanced Nursing, 73, 1807–1824. https://doi.org/10.1111/jan.13249
Elissen, A., Nolte, E., Knai, C., Brunn, M., Chevreul, K., Conklin, A., . . . Vrijhoef, H. (2013). Is Europe putting theory into practice? A qualitative study of the level of self-management support in chronic care management approaches. BMC Health Services Research, 13, 117. https://doi.org/10.1186/1472-6963-13-117
Ercolano, E., Grant, M., McCorkle, R., Tallman, N.J., Cobb, M.D., Wendel, C., & Krouse, R. (2016). Applying the chronic care model to support ostomy self-management: Implications for oncology nursing practice. Clinical Journal of Oncology Nursing, 20, 269–274. https://doi.org/10.1188/16.CJON.20-03AP
Faithfull, S., Samuel, C., Lemanska, A., Warnock, C., & Greenfield, D. (2016). Self-reported competence in long term care provision for adult cancer survivors: A cross sectional survey of nursing and allied health care professionals. International Journal of Nursing Studies, 53, 85–94. https://doi.org/10.1016/j.ijnurstu.2015.09.001
Girgis, A., Lambert, S., Johnson, C., Waller, A., & Currow, D. (2013). Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. Journal of Oncology Practice, 9, 197–202. https://doi.org/10.1200/JOP.2012.000690
Glasgow, R.E., Davis, C.L., Funnell, M.M., & Beck, A. (2003). Implementing practical interventions to support chronic illness self-management. Joint Commission Journal on Quality and Safety, 29, 563–574.
Griffiths, P., Simon, M., Richardson, A., & Corner, J. (2013). Is a larger specialist nurse workforce in cancer care associated with better patient experience? Cross-sectional study. Journal of Health Services Research and Policy, 18(1 Suppl. 2), 39–46. https://doi.org/10.1177/1355819612473451
Hoek, P.D., Schers, H.J., Bronkhorst, E.M., Vissers, K.C.P., & Hasselaar, J.G.J. (2017). The effect of weekly specialist palliative care teleconsultations in patients with advanced cancer—A randomized clinical trial. BMC Medicine, 15, 119. https://doi.org/10.1186/s12916-017-0866-9
Johnston, B., McGill, M., Milligan, S., McElroy, D., Foster, C., & Kearney, N. (2009). Self care and end of life care in advanced cancer: Literature review. European Journal of Oncology Nursing, 13, 386–398. https://doi.org/10.1016/j.ejon.2009.04.003
Johnston, B.M., Milligan, S., Foster, C., & Kearney, N. (2012). Self-care and end of life care—Patients’ and carers’ experience a qualitative study utilising serial triangulated interviews. Supportive Care in Cancer, 20, 1619–1627. https://doi.org/10.1007/s00520-011-1252-3
Khan, N.F., Mant, D., Carpenter, L., Forman, D., & Rose, P.W. (2011). Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: A database study. British Journal of Cancer, 105(Suppl. 1), S29–S37. https://doi.org/10.1038/bjc.2011.420
Knobf, M.T. (2013). Being prepared: Essential to self-care and quality of life for the person with cancer. Clinical Journal of Oncology Nursing, 17, 255–261. https://doi.org/10.1188/13.CJON.255-261
Landier, W. (2009). Survivorship care: Essential components and models of delivery. Oncology (Williston Park), 23(4 Suppl. Nurse Ed), 46–53.
Lenihan, D.J., Oliva, S., Chow, E.J., & Cardinale, D. (2013). Cardiac toxicity in cancer survivors. Cancer, 119(Suppl. 11), 2131–2142. https://doi.org/10.1002/cncr.28061
Lin, H.R., & Bauer-Wu, S.M. (2003). Psycho-spiritual well-being in patients with advanced cancer: An integrative review of the literature. Journal of Advanced Nursing, 44, 69–80.
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians, 61, 50–62. https://doi.org/10.3322/caac.20093
Noonan, V.K., Lyddiatt, A., Ware, P., Jaglal, S.B., Riopelle, R.J., Bingham, C.O., III, . . . Ahmed, S. (2017). Montreal Accord on patient-reported outcomes (PROs) use series—Paper 3: Patient-reported outcomes can facilitate shared decision-making and guide self-management. Journal of Clinical Epidemiology, 89, 125–135. https://doi.org/10.1016/j.jclinepi.2017.04.017
Sahlsten, M.J.M., Larsson, I.E., Sjöström, B., Lindencrona, C.S., & Plos, K.A.E. (2007). Patient participation in nursing care: Towards a concept clarification from a nurse perspective. Journal of Clinical Nursing, 16, 630–637. https://doi.org/10.1111/j.1365-2702.2006.01660.x
Schulman-Green, D., Bradley, E.H., Knobf, M.T., Prigerson, H., DiGiovanna, M.P., & McCorkle, R. (2011). Self-management and transitions in women with advanced breast cancer. Journal of Pain and Symptom Management, 42, 517–525. https://doi.org/10.1016/j.jpainsymman.2010.12.007
Schulman-Green, D., Jaser, S., Martin, F., Alonzo, A., Grey, M., McCorkle, R., . . . Whittemore, R. (2012). Processes of self-management in chronic illness. Journal of Nursing Scholarship, 44, 136–144. https://doi.org/10.1111/j.1547-5069.2012.01444.x
Slev, V.N., Mistiaen, P., Pasman, H.R.W., Verdonck-de Leeuw, I.M., van Uden-Kraan, C.F., & Francke, A.L. (2016). Effects of eHealth for patients and informal caregivers confronted with cancer: A meta-review. International Journal of Medical Informatics, 87, 54–67. https://doi.org/10.1016/j.ijmedinf.2015.12.013
Slev, V.N., Pasman, H.R.W., Eeltink, C.M., van Uden-Kraan, C.F., Verdonck-de Leeuw, I.M., & Francke, A.L. (2017). Self-management support and eHealth for patients and informal caregivers confronted with advanced cancer: An online focus group study among nurses. BMC Palliative Care, 16, 55. https://doi.org/10.1186/s12904-017-0238-4
Ter Maten-Speksnijder, A.J., Dwarswaard, J., Meurs, P.L., & van Staa, A. (2016). Rhetoric or reality? What nurse practitioners do to provide self-management support in outpatient clinics: An ethnographic study. Journal of Clinical Nursing, 25, 3219–3228. https://doi.org/10.1111/jocn.13345
Tocchi, C., McCorkle, R., & Knobf, M.T. (2015). Multidisciplinary specialty teams: A self-management program for patients with advanced cancer. Journal of the Advanced Practitioner in Oncology, 6, 408–416.
van Hooft, S.M., Becqué, Y.N., Dwarswaard, J., van Staa, A., & Bal, R. (2018). Teaching self-management support in Dutch Bachelor of Nursing education: A mixed methods study of the curriculum. Nurse Education Today, 68, 146–152. https://doi.org/10.1016/j.nedt.2018.06.005
van Hooft, S.M., Dwarswaard, J., Bal, R., Strating, M.M., & van Staa, A. (2016). What factors influence nurses’ behavior in supporting patient self-management? An explorative questionnaire study. International Journal of Nursing Studies, 63, 65–72. https://doi.org/10.1016/j.ijnurstu.2016.08.017
van Houwelingen, C.T.M. (2018). Telehealth competence in nursing: Enhancing skills and practice in providing care remotely (Doctoral dissertation). Retrieved from https://dspace.library.uu.nl/handle/1874/364125
van Houwelingen, C.T.M., Ettema, R.G.A., Kort, H.S.M., & ten Cate, O. (2017). Internet-generation nursing students’ view of technology-based health care. Journal of Nursing Education, 56, 717–724. https://doi.org/10.3928/01484834-20171120-03
Ventura, A.D., Burney, S., Brooker, J., Fletcher, J., & Ricciardelli, L. (2014). Home-based palliative care: A systematic literature review of the self-reported unmet needs of patients and carers. Palliative Medicine, 28, 391–402. https://doi.org/10.1177/0269216313511141
Von Korff, M., Gruman, J., Schaefer, J., Curry, S.J., & Wagner, E.H. (1997). Collaborative management of chronic illness. Annals of Internal Medicine, 127, 1097–1102.


