Fear of Cancer Recurrence: A Systematic Review of Randomized, Controlled Trials
Problem Identification: Fear of cancer recurrence (FCR) is prevalent among people with cancer; therefore, it is important to determine whether interventions offered to this population are effective in alleviating FCR. This review summarizes randomized, controlled trials in the literature about the effect of psychosocial interventions on FCR in people with cancer.
Literature Search: A systematic review of the literature was conducted using PubMed, Web of Science, EMBASE, and Cochrane Library.
Data Evaluation: Extracted data included cancer type, number of participants, intervention type and duration, follow-ups, and primary and secondary outcomes.
Synthesis: 10 studies met inclusion criteria. Types of interventions included mindfulness-based therapy (n = 3), cognitive behavioral therapy (n = 4), psychoeducational interventions (n = 1), gratitude interventions (n = 1), and communication interventions (n = 1).
Implications for Practice: Psychosocial interventions are beneficial for alleviating FCR and positively affect depression, anxiety, and quality of life in people with cancer.
Jump to a section
Fear of cancer recurrence (FCR) is defined as “fear, worry, or concern about cancer returning or progressing” (Lebel et al., 2016, p. 3,267). This is one of the most normal and aversive psychological phenomena among people with cancer and is also one of the top concerns consistently described (Simard, Savard, & Ivers, 2010). FCR may persist many years after cancer treatment (Wagner et al., 2011). Evidence has shown that its incidence was as high as 99%, and about one-third of people reported high FCR, which seriously affected their physical and mental health (Koch et al., 2014). In addition, people with cancer who experience high levels of FCR may report negative behavior changes (Lasry & Margolese, 1992), difficulties making future plans (Hart, Latini, Cowan, & Carroll, 2008), excessive use of health services (Lebel, Tomei, Feldstain, Beattie, & McCallum, 2013), and greater psychological distress (Alfano & Rowland, 2006). For example, among those with clinical FCR, 36% met the screening criteria for general anxiety disorder, and 43% met the screening criteria for hypochondriasis (Thewes et al., 2013). In particular, even high levels of FCR can become a chronic problem for people with cancer (Custers et al., 2014). If FCR could be alleviated or reduced, people with cancer may enjoy better quality of life. The high occurrence of FCR and its potentially negative impacts make it imperative to identify valid treatments aimed at helping people address FCR.
Psychosocial interventions are aimed at satisfying the psychological, mental, and social needs of patients rather than treating the disease itself (Turner et al., 2005). Psychosocial interventions include behavioral therapy, cognitive therapy, counseling, psychological therapy, and education (Coughtrey et al., 2018). Given the key role of supportive care interventions in improving health and wellness (Wolin & Colditz, 2011), researchers have actively explored the effects of psychosocial interventions on FCR. A number of studies have revealed that psychosocial interventions could contribute to relieving FCR and improving quality of life among people with cancer (Wagner et al., 2011). A meta-analysis indicated a positive effect of mindfulness-based stress reduction (MBSR) on reducing FCR in people with breast cancer. However, this review included only two studies (Zhang, Xu, Wang, & Wang, 2016). Another review of the literature suggested that interventions to manage uncertainty and FCR in women with breast cancer may have positive and negative effects, but the articles included in the review were not all well-designed randomized, controlled trials (RCTs) (Dawson, Madsen, & Dains, 2016). RCTs are the gold standard for evidence-based clinical research and could provide reliable and useful information for relieving FCR. Given the limitations of these studies (Dawson et al., 2016; Zhang et al., 2016), the current systematic review, which covers a wide range of cancer types, high-quality RCTs, and diverse psychosocial intervention methods, is warranted.
Decisions regarding specific treatment options for people with cancer should be informed by knowledge of all effective interventions for FCR and incorporate individuals’ preferences in the management of FCR. To provide healthcare professionals with useful information, the authors based the current study on RCTs examining the effect of psychosocial interventions on FCR. The study identifies research limitations and proposes recommendations on the application of psychosocial interventions for the management of FCR. In addition, the authors focus on secondary consequences improved by psychosocial interventions. Specifically, they hypothesized that psychosocial interventions would be effective in reducing FCR.
Methods
Search Strategy
PubMed, Web of Science, EMBASE, and the Cochrane Library were comprehensively searched for articles that were published through August 2017. Search terms were combined from conjunctions of the following terms: (“Neoplasia” OR “Neoplasias” OR “Neoplasm” OR “Tumors” OR “Tumor” OR “Benign Neoplasms” OR “Neoplasms, Benign” OR “Benign Neoplasm” OR “Neoplasm, Benign” OR “Malignancy” OR “Malignancies” OR “Cancer” OR “Cancers” OR “Neoplasms”) AND (“Randomized Controlled Trial” OR “Clinical Trials, Randomized” OR “Trials, Randomized Clinical” OR “Controlled Clinical Trials, Randomized” OR “Randomized Controlled Trials as Topic”) AND (“fear of recurrence” OR “fear of recurrences” OR “recurrence worries” OR “recurrence worry” OR “recurrence concerns” OR “recurrence concern” OR “uncertainties” OR “uncertainty” OR “fear of progression” OR “fears of progressions” OR “fear” OR “fears”). Manual searches were conducted for cited references in relevant articles, and review articles were extracted from the database searches and in Google Scholar by using the combination of terms.
Eligibility Criteria
Inclusion criteria were as follows:
• People with cancer aged older than 18 years
• People with cancer who received psychosocial interventions
• Study designs were RCTs.
• FCR was an outcome measure.
Exclusion criteria for the systematic review were as follows:
• Studies did not report FCR as an outcome.
• Only study protocols were reported.
• Intervention methods were not psychosocial interventions.
• Participants who did not have or never had cancer.
• Studies were quasiexperimental designs.
Study Selection
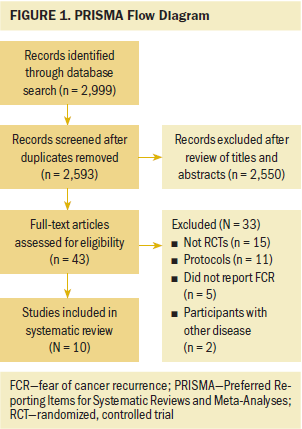
The review was conducted and reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009). After eliminating duplicate studies, two reviewers independently screened the titles and abstracts of all potentially relevant studies. The authors finally obtained the full-text articles for this systematic review and identified the articles that coincided with the eligibility criteria.
Data Extraction and Analysis
The data were extracted from the included articles using standardized extraction forms. Data included sample characteristics, number of participants in experimental and control groups, duration of interventions, intervention methods, follow-ups, and outcomes. Two reviewers independently conducted data extraction on each study, and any inconsistencies were resolved through discussion with a third reviewer. Authors of the studies were contacted if more data were needed. Given the heterogeneity of cancer types, study designs, intervention approaches, assessments of risk of bias, and outcome measurements, the authors did not conduct a meta-analysis. Review Manager, version 5.3, was used to systematically review the outcomes of the diverse psychosocial interventions for FCR in people with cancer.
Quality Assessment
Two reviewers (CDD and SWJ) independently assessed the quality of all studies with the Cochrane Collaboration Risk of Bias Tool. Studies were assessed using six criteria: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias (Higgins, Altman, & Sterne, 2011). If two reviewers disagreed, a third author (ZW) was available for assessment.
Results
The selection process is illustrated in Figure 1. The authors retrieved 2,999 articles from the database at the beginning of the study. Because of duplicates, 406 documents were removed, leaving 2,593 articles that were included and screened for further assessment. Ten RCTs completely matched eligibility criteria for systematic review.
Study Characteristics and Quality
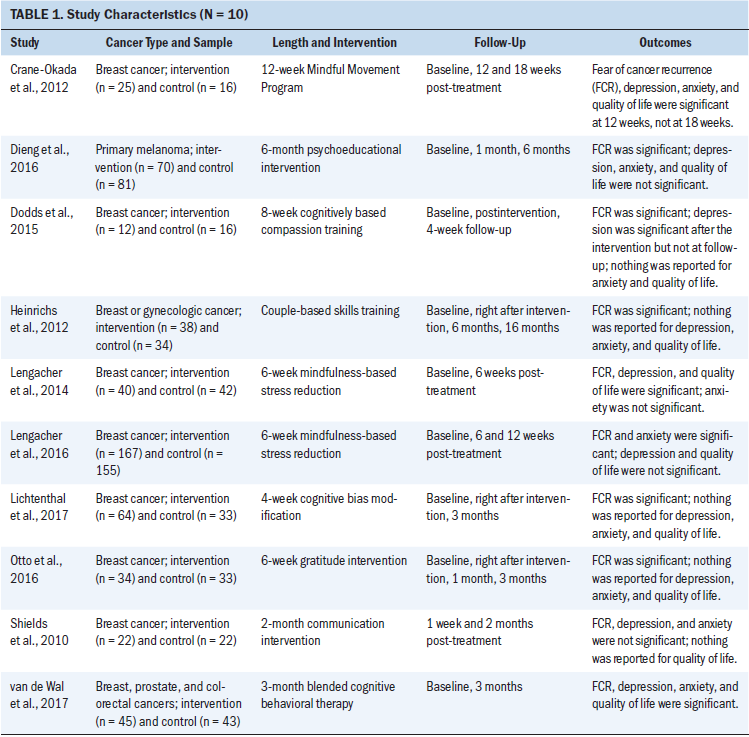
Table 1 summarizes the characteristics of the included studies. A total of 992 people with cancer were included in this study. Out of the 10 included studies, 7 sampled people with breast cancer, 2 included people with breast cancer and people with others cancers, and 1 sampled people with primary melanoma. The types of interventions included were MBSR (n = 3), cognitive behavioral therapy (CBT) (n = 4), psychoeducational interventions (n = 1), gratitude interventions (n = 1), and communication interventions (n = 1).
Most studies randomized participants to either a treatment or control group. However, allocation concealment was not adequately described. Most interventions did not perform the procedure of blinding, which may increase bias. Attrition bias and reporting bias were low. Overall, most of the studies were of medium methodologic quality.
Effectiveness of Psychosocial Interventions
Mindfulness-based stress reduction: Three studies involving 445 participants examined the effect of MBSR on FCR in people with cancer (Crane-Okada et al., 2012; Lengacher et al., 2014, 2016). The duration of the intervention varied from 6 weeks (Lengacher et al., 2014, 2016) to 12 weeks (Crane-Okada et al., 2012). The follow-ups lasted from 6 weeks (Lengacher et al., 2014) to 18 weeks (Crane-Okada et al., 2012).
Lengacher et al. (2014) evaluated the outcomes of a six-week MBSR program on the psychological and physical symptoms of people with cancer, with FCR examined as a mediator. Participants attended weekly two-hour sessions conducted by an experienced psychologist and received a training manual and four audiotapes for home practice, which consisted of sitting meditation, walking meditation, body scans, and gentle yoga.
Lengacher et al. (2016) explored the viability of a six-week MBSR program intervention on people with breast cancer. Similarly, the intervention provided two-hour sessions by a clinical psychologist trained in MBSR once per week for six weeks. The psychologist provided participants with training manuals and CDs, and taught informal skills of integrating mindfulness into daily practice. Adherence was assessed by the number of classes attended, the number of minutes practiced, and the completion of diaries.
Crane-Okada et al. (2012) explored the efficacy of a 12-week Mindful Movement Program (MMP) combining mindfulness with self-directed movement on quality of life in women with breast cancer. The MMP used the concept of mindfulness to stimulate self-directed movements and guide participants to explore and understand their thoughts, feelings, and sensations. A typical two-hour MMP session included time allocation of the MMP contents and standard forms of walking or other types of movement; exploration of specific body parts; verbal sharing; soft, slow, and small movements; discovery (more conscious effort); positive motivation; and some partner work (e.g., while moving in relation to “another,” still paying attention to the “self”).
Crane-Okada et al. (2012) reported no significant effect of the MMP on FCR in the intervention group at 18 weeks post-treatment compared to the control group. However, this study reported a significant effect of MMP on FCR at 12 weeks post-treatment in people with cancer compared to the intervention group. Three studies (Crane-Okada et al., 2012; Lengacher et al., 2014, 2016) reported a significant effect of MBSR on FCR in people with cancer compared to the control group. In addition, for secondary outcomes, Lengacher et al. (2014) showed that MBSR reduced depression and improved quality of life, and although there was a reduction in state anxiety, it did not reach statistical significance. Lengacher et al. (2016) showed significant improvements in anxiety in the experimental group but reported no differences in depression and quality of life. Crane-Okada et al. (2012) found that participants in the MMP group had significant improvements in depression, anxiety, and quality of life at 12 weeks post-treatment. In addition, patients reported no significant differences in outcomes at 18 weeks post-treatment.
Cognitive behavioral therapy: Four studies with 285 participants examined the effects of CBT on FCR and other secondary outcomes among people with cancer (Dodds et al., 2015; Heinrichs et al., 2012; Lichtenthal et al., 2017; van de Wal, Thewes, Gielissen, Speckens, & Prins, 2017). The intervention duration varied from 4 weeks (Lichtenthal et al., 2017) to 3 months (van de Wal et al., 2017). The follow-up period lasted from 4 weeks (Dodds et al., 2015) to 16 months (Heinrichs et al., 2012).
Dodds et al. (2015) investigated the efficacy of Cognitively Based Compassion Training (CBCT) on people with breast cancer. This involved pedagogy and class discussions to guide meditation exercises eight times per week during two-hour classes. Participants were required to perform at least three meditation exercises per week, use guided meditation recordings (average 30 minutes), and maintain practice logs. Participants had access to a recording on a private website (and/or received a flash drive). Participants in the CBCT group showed significant improvements in functional impairment associated with FCR (Dodds et al., 2015). For reported depression, differences between groups were detected after the intervention but not at the one-month follow-up (Dodds et al., 2015).
Lichtenthal et al. (2017) tested a four-week cognitive bias modification training to manage FCR. The intervention consisted of 8 personalized treatments, 30 minutes per treatment twice a week, for a total of 4 weeks. The first part was completed at the clinic, and the subsequent parts were completed at home. The intervention involved completing the attention modification task and the interpretation modification task. Lichtenthal et al. (2017) found a significantly positive effect of the intervention on FCR compared to that of the usual care group.
Van de Wal et al. (2017) tested the feasibility of blended cognitive behavioral therapy (BCBT) for high FCR in people with breast, prostate, and colorectal cancer. Interventions were offered within three months via five 1-hour face-to-face meetings (sessions 1–3, 5, and 8) and three 15-minute electronic consultations (chat application, no video) with access to the website (conversation 4, 6, and 7). If participants were unable to use the website or had no access to the Internet, they received three 15-minute telephone consultations and a workbook. Websites and workbooks had congruent content. Intervention techniques included psychological education, cognitive restructuring, and behavior modification. Significant improvements in depression, anxiety, and quality of life scores were observed (van de Wal et al., 2017).
Heinrichs et al. (2012) assessed the effects of a couples-based skills training on cancer distress in women with breast or gynecologic cancer. The intervention consisted of four biweekly face-to-face sessions with a therapist in the couple’s home, and each session lasted two hours. The core of the intervention was communication skills and dyadic coping training. Communication skills training using speaker and listener guidelines aimed to teach couples to discuss disturbing topics within the relationship. The three-phase method was designed to increase dyadic coping. Those who received BCBT reported significantly less FCR than those who received usual care. Women receiving the intervention showed larger reductions of FCR during the intervention.
Psychoeducational intervention: One study with 151 participants investigated the efficacy of a psychoeducational intervention on FCR in people at high risk for developing another primary melanoma (Dieng et al., 2016). The intervention lasted six months, and the follow-ups occurred at one month and six months postintervention. This intervention included two key components: a newly developed psychoeducational booklet and three individual telephone-based psychotherapeutic sessions with a psychologist. The intervention group reported lower FCR severity, trigger, and distress scores than the control group in the baseline-adjusted models at six months. However, the authors did not find statistically significant effects of the intervention on depression, anxiety, and quality of life between the experimental and control groups.
Gratitude intervention: One study with 67 participants investigated a gratitude intervention, randomly assigning participants to a six-week online gratitude intervention (n = 34) or a six-week online control condition (n = 33) (Otto, Szczesny, Soriano, Laurenceau, & Siegel, 2016). Each week, the participants in the gratitude intervention were asked to write a letter for 10 minutes to express their gratitude to a person of their choice. The participants in the control group were asked to spend 10 minutes listing and briefly describing 20 activities in which they had engaged in the past several weeks. The authors found a significant decrease in death-related FCR in the intervention group compared to the controls across the study period.
Communication intervention: Shields et al. (2010) conducted an intervention to improve communication between people with breast cancer and their physicians. In the intervention, the coach asked each survivor to say what she wanted to tell her oncologist about cancer-related concerns; the coach then asked each participant to prioritize what she wanted to discuss with her oncologist. The coach typed the survivors’ concerns into a summary form and mailed it to them so that, at their upcoming visit, they could tell their oncologist about the issues that normally remained unspoken. Surprisingly, no significant differences in FCR were found between groups, but the authors reported that the intervention led to increased self-efficacy. Changes in self-efficacy predicted changes in anxiety, depression, and womanhood fears (the Womanhood Fears is a subscale of the Concerns About Recurrence Scale and assesses breast cancer recurrence-related worries about womanhood), which was an aspect of FCR. As a result, communication interventions could indirectly affect FCR.
Discussion
This study systematically reviewed the effects of MBSR, CBT, psychoeducational interventions, gratitude interventions, and communication interventions on FCR and secondary outcomes (depression, anxiety, quality of life) in people with cancer. The 10 studies were rather heterogeneous in terms of the type of intervention content, sample characteristics, and intervention duration. Although the effects of psychosocial interventions on the intervention outcomes differed, this review provided support for psychosocial interventions as feasible, acceptable, and potentially efficacious methods for psychosocial outcomes.
Most studies in the current review were conducted in women with breast cancer, presenting a relative bias. The current authors noted that at least 686 of 992 participants had breast cancer, which is the most common type of cancer and the most common cause of cancer death in women worldwide (Ferlay et al., 2015; Hortobagyi et al., 2005). Although the five-year relative survival rate of people with breast cancer is on the rise (Siegel, Ma, Zou, & Jemal, 2015), the long-term and adverse effects of breast cancer treatment still exist (Fang, Fetzer, Lee, & Kuo, 2018). It is possible that people with breast cancer are most concerned about FCR (Ashing-Giwa & Lim, 2011). The current findings for the effect of MBSR on FCR were consistent with previous evidence indicating that MBSR was effective in reducing FCR (Zhang et al., 2016). Mindfulness practices may reduce the intensity of cognitive processes by lowering the frequency of negative automatic thinking (Frewen, Evans, Maraj, Dozois, & Partridge, 2008) or by affecting physiologic arousal (Shi & MacBeth, 2017). The performance of the MBSR was similar among the three included studies in terms of session content. However, Crane-Okada et al. (2012) indicated no significant improvements in FCR at 18 weeks post-treatment in the intervention group, although participants reported improvements at 12 weeks post-treatment. This may have been because the reduction in FCR in the intervention group was retained at 12 weeks (Crane-Okada et al., 2012). As a result, MBSR may be an important strategy for reducing FCR.
In the systematic review, CBT consisted of CBCT, cognitive bias modification training, BCBT, and a couples-based skills training. Notable content differences existed among the four types of CBT. CBT focuses on identifying and changing a person’s adaptation to a mode of negative thinking to reduce negative emotions and promote psychological adjustment. It has been used for many diseases and has achieved positive effects (Galla et al., 2012; Greer et al., 2012; Lopez et al., 2011). The current study showed that CBT had a beneficial effect on FCR in people with cancer, which is consistent with the results of two other studies (DiBonaventura, Erblich, Sloan, & Bovbjerg, 2010; Herschbach et al., 2010). Chronic illnesses follow a treatment trajectory similar to that of cancer, which includes periods of absence from education, long treatment times, and painful procedures. As a result, CBT intervention effects may be transferable and effective across diagnoses (Coughtrey et al., 2018).
One study showed that psychoeducational interventions could be a feasible and well-accepted method of reducing FCR in people at high risk for developing another primary melanoma (Dieng et al., 2016). However, the sample was small, and actual implementation results need to be verified. In addition, because of the debate regarding the Fear of Cancer Recurrence Inventory clinical cutoff score (Lebel et al., 2016) and the observation of other health and educational benefits in this trial, the current authors concluded that this intervention should be provided only to patients who reported FCR within clinical practice without further research to address this issue (Dieng et al., 2016).
Gratitude has consistently yielded individual and interpersonal benefits, including increased well-being and life satisfaction (Peterson, Ruch, Beermann, Park, & Seligman, 2007; Sheldon & Lyubomirsky, 2006). Gratitude may have improved well-being by motivating increases in overall positive affect (Otto et al., 2016). Compared to existing psychosocial interventions for people with cancer, gratitude interventions are relatively low cost, scalable, and portable, and do not require experienced healthcare professionals for delivery. These results provide support for the clinical application of the gratitude intervention.
This study revealed no effects of the communication intervention on FCR. The communication intervention had no direct effect on FCR, but changes in self-efficacy directly predicted FCR (Shields et al., 2010). Several reasons may account for this finding. The decreased power related to a small sample size was an issue. In addition, Shields et al. (2010) conducted an intervention to test methods for improving the communication of people with breast cancer with their physicians about fears and concerns regarding their illness. However, FCR was not the immediate focus of this communication intervention, which resulted in a failure to detect significant changes. However, the indirect effect on FCR in this study inspired the current authors to focus on the communication intervention and conduct additional studies to determine its efficacy and effectiveness.
In addition to FCR, this systematic review aimed to analyze the effects of psychosocial interventions on secondary outcomes concerning depression, anxiety, and quality of life. Seven articles reported these outcomes (Crane-Okada et al., 2012; Dieng et al., 2016; Dodds et al., 2015; Lengacher et al., 2014, 2016; Shields et al., 2010; van de Wal et al., 2017). Among these studies, four (Dieng et al., 2016; Lengacher et al., 2014, 2016; Shields et al., 2010) showed no changes in depression, anxiety, and quality of life, which was inconsistent with the suggested benefits of psychosocial interventions reported in a systematic review in pediatric oncology (Coughtrey et al., 2018). Several factors may explain the effects of this intervention. In Dieng et al. (2016), the low levels of depression and anxiety reported at baseline resulted in floor effects. In addition, relatively small effect sizes may have resulted from low symptom levels at baseline (floor effects), particularly because Lengacher et al. (2016) did not screen for high levels of anxiety and/or depression before enrollment. Lengacher et al. (2014) and Shields et al. (2010) did not state specific reasons. Overall, psychosocial interventions are promising therapies for people with cancer.
Limitations
This study retrieved only English literature from four databases, and there may be incomplete information contained in the publication bias. Because of some methodologic flaws in the literature, additional well-designed RCTs with large sample sizes are needed to confirm effectiveness of these preliminary estimates. Most of the studies were also conducted in the United States, so the generalization of the results to other countries may not be possible. Additional research needs to be conducted on larger sample sizes in more areas. In addition, most of the included studies used interventions conducted during a six-week period; studies that examine the long-term effects of psychosocial interventions and their follow-ups on outcomes of individuals with cancer are needed. Limitations notwithstanding, the current review suggested that most psychosocial interventions were effective in reducing FCR and other psychosocial outcomes.
Implications for Nursing
This systematic review provides evidence supporting interventions for FCR and other psychological problems in people with cancer. Ultimately, the use of psychosocial interventions by healthcare professionals may relieve FCR, depression, or anxiety and improve quality of life in people with cancer. Specifically, MBSR and CBT were widely used, and the effects of interventions were promising. This effort will contribute to effective patient-centered nursing care in oncology.
As the population with cancer increases, there is a greater need for research on FCR. Research should be conducted to determine the most effective psychosocial interventions in terms of intervention method, intervention time, and session content. The authors propose additional studies that compare the different types of interventions and perform a meta-analysis in homogeneous intervention subgroups.
Also, most interventions were carried out by trained psychologists. As coordinators and advocates of patient care, nurses rarely participated in the psychosocial interventions, perhaps because they cannot deliver professional psychological interventions to people with cancer. In addition, oncology departments do not always have enough available resources to employ psychologists. As a result, it is important for nurses to complete professional training and education in psychological interventions when cooperating with psychotherapists, particularly in implementing interventions, improving intervention compliance, and consolidating the efficacy of different aspects of interventions. For example, nurses can leverage information resources by educating themselves about a range of psychological interventions aimed at reducing FCR in people with cancer and incorporate those interventions into their practice. In addition, institutions could invite psychologists to train and educate nurses and encourage qualified nurses to obtain further certification. Finally, nursing can be involved in nurse-led, patient-centered psychological interventions. Meanwhile, investigating the cost-effectiveness of nurses delivering psychological interventions and exploring the mechanisms through which these psychological interventions work are areas for future research. [[{"fid":"47441","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Conclusion
Several psychosocial intervention options are available for managing FCR in people with cancer. Of the interventions reported in this review, not all were effective; however, sufficient evidence shows that psychosocial interventions are beneficial in alleviating FCR. The principles of patient-centered care require healthcare professionals to provide a range of effective interventions rather than a one-size-fits-all solution. This systematic review offers evidence of effective psychosocial interventions that should be considered part of a management strategy for people with cancer who are experiencing FCR. Because of the many other beneficial effects of psychosocial interventions, healthcare professionals should encourage people with cancer to accept these interventions.
About the Author(s)
Dandan Chen, RN, Weijia Sun, RN, Na Liu, RN, and Jie Wang, RN, are postgraduate students, Jingxia Zhao, MM, is a senior experimentalist, Yue Zhang, MM, and Jinquan Liu, MM, are research assistants, and Wei Zhang, PhD, is an associate professor, all in the School of Nursing at Jilin University in Changchun, China. The authors gratefully acknowledge the student nurses who participated in the investigation. No financial relationships to disclose. Chen, Zhao, and W. Zhang contributed to the conceptualization and design. Sun, N. Liu, Wang, Y. Zhang, J. Liu, and W. Zhang completed the data collection. Chen, N. Liu, Wang, Y. Zhang, and W. Zhang provided statistical support. N. Liu, Wang, Zhao, J. Liu, and W. Zhang provided the analysis. Chen and W. Zhang contributed to the manuscript preparation. W. Zhang can be reached at hlzhangw99@163.com, with copy to ONFEditor@ons.org. (Submitted April 2018. Accepted June 13, 2018.)
References
Alfano, C.M., & Rowland, J.H. (2006). Recovery issues in cancer survivorship: A new challenge for supportive care. Cancer Journal, 12, 432–443.
Ashing-Giwa, K.T., & Lim, J.-W. (2011). Examining emotional outcomes among a multiethnic cohort of breast cancer survivors. Oncology Nursing Forum, 38, 279–288. https://doi.org/10.1188/11.ONF.279-288
Coughtrey, A., Millington, A., Bennett, S., Christie, D., Hough, R., Su, M.T., . . . Shafran, R. (2018). The effectiveness of psychosocial interventions for psychological outcomes in pediatric oncology: A systematic review. Journal of Pain and Symptom Management, 55, 1004–1017. https://doi.org/10.1016/j.jpainsymman.2017.09.022
Crane-Okada, R., Kiger, H., Sugerman, F., Uman, G.C., Shapiro, S.L., Wyman-McGinty, W., & Anderson, N.L. (2012). Mindful movement program for older breast cancer survivors: A pilot study. Cancer Nursing, 35(4), E1–E13. https://doi.org/10.1097/NCC.0b013e3182280f73
Custers, J.A., van den Berg, S.W., van Laarhoven, H.W., Bleiker, E.M., Gielissen, M.F., & Prins, J.B. (2014). The Cancer Worry Scale: Detecting fear of recurrence in breast cancer survivors. Cancer Nursing, 37, E44–E50. https://doi.org/10.1097/NCC.0b013e3182813a17
Dawson, G., Madsen, L.T., & Dains, J.E. (2016). Interventions to manage uncertainty and fear of recurrence in female breast cancer survivors: A review of the literature [Online exclusive]. Clinical Journal of Oncology Nursing, 20, E155–E161. https://doi.org/10.1188/16.CJON.E155-E161
DiBonaventura, M.D., Erblich, J., Sloan, R.P., & Bovbjerg, D.H. (2010). A computerized Stroop task to assess cancer-related cognitive biases. Behavioral Medicine, 36(2), 37–43. https://doi.org/10.1080/08964280903521321
Dieng, M., Butow, P.N., Costa, D.S.J., Morton, R.L., Menzies, S.W., Mireskandari, S., . . . Kasparian, N.A. (2016). Psychoeducational intervention to reduce fear of cancer recurrence in people at high risk of developing another primary melanoma: Results of a randomized controlled trial. Journal of Clinical Oncology, 34, 4405–4414. https://doi.org/10.1200/JCO.2016.68.2278
Dodds, S.E., Pace, T.W.W., Bell, M.L., Fiero, M., Negi, L.T., Raison, C.L., & Weihs, K.L. (2015). Feasibility of cognitively-based compassion training (CBCT) for breast cancer survivors: A randomized, wait list controlled pilot study. Supportive Care in Cancer, 23, 3599–3608. https://doi.org/10.1007/s00520-015-2888-1
Fang, S.-Y., Fetzer, S.J., Lee, K.-T., & Kuo, Y.-L. (2018). Fear of recurrence as a predictor of care needs for long-term breast cancer survivors. Cancer Nursing, 41, 69–76. https://doi.org/10.1097/NCC.0000000000000455
Ferlay, J., Soerjomataram, I., Dikshit, R., Eser, S., Mathers, C., Rebelo, M., . . . Bray, F. (2015). Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer, 136, E359–E386. https://doi.org/10.1002/ijc.29210
Frewen, P.A., Evans, E.M., Maraj, N., Dozois, D.J.A., & Partridge, K. (2008). Letting go: Mindfulness and negative automatic thinking. Cognitive Therapy and Research, 32, 758–774. https://doi.org/10.1007/s10608-007-9142-1
Galla, B.M., Wood, J.J., Chiu, A.W., Langer, D.A., Jacobs, J., Ifekwunigwe, M., & Larkins, C. (2012). One year follow-up to modular cognitive behavioral therapy for the treatment of pediatric anxiety disorders in an elementary school setting. Child Psychiatry and Human Development, 43, 219–226. https://doi.org/10.1007/s10578-011-0258-x
Greer, J.A., Traeger, L., Bemis, H., Solis, J., Hendriksen, E.S., Park, E.R., . . . Safren, S.A. (2012). A pilot randomized controlled trial of brief cognitive-behavioral therapy for anxiety in patients with terminal cancer. Oncologist, 17, 1337–1345. https://doi.org/10.1634/theoncologist.2012-0041
Hart, S.L., Latini, D.M., Cowan, J.E., & Carroll, P.R. (2008). Fear of recurrence, treatment satisfaction, and quality of life after radical prostatectomy for prostate cancer. Supportive Care in Cancer, 16, 161–169. https://doi.org/10.1007/s00520-007-0296-x
Heinrichs, N., Zimmermann, T., Huber, B., Herschbach, P., Russell, D.W., & Baucom, D.H. (2012). Cancer distress reduction with a couple-based skills training: A randomized controlled trial. Annals of Behavioral Medicine, 43, 239–252. https://doi.org/10.1007/s12160-011-9314-9
Herschbach, P., Book, K., Dinkel, A., Berg, P., Waadt, S., Duran, G., . . . Henrich, G. (2010). Evaluation of two group therapies to reduce fear of progression in cancer patients. Supportive Care in Cancer, 18, 471–479. https://doi.org/10.1007/s00520-009-0696-1
Higgins, J.P.T., Altman, D.G., & Sterne, J.A.C. (Eds.). (2011). Assessing risk of bias in included studies. In J.P.T. Higgins & S. Green (Eds.), Cochrane handbook for systematic reviews of interventions [v.5.1.0]. The Cochrane Collaboration. Retrieved from www.handbook.cochrane.org
Hortobagyi, G.N., de la Garza Salazar, J., Pritchard, K., Amadori, D., Haidinger, R., Hudis, C.A., . . . Albain, K.S. (2005). The global breast cancer burden: Variations in epidemiology and survival. Clinical Breast Cancer, 6, 391–401.
Koch, L., Bertram, H., Eberle, A., Holleczek, B., Schmid-Höpfner, S., Waldmann, A., . . . Arndt, V. (2014). Fear of recurrence in long-term breast cancer survivors—Still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship—A multi-regional population-based study. Psycho-Oncology, 23, 547–554. https://doi.org/10.1002/pon.3452
Lasry, J.C., & Margolese, R.G. (1992). Fear of recurrence, breast-conserving surgery, and the trade-off hypothesis. Cancer, 69, 2111–2115.
Lebel, S., Ozakinci, G., Humphris, G., Mutsaers, B., Thewes, B., Prins, J., . . . Butow, P. (2016). From normal response to clinical problem: Definition and clinical features of fear of cancer recurrence. Supportive Care in Cancer, 24, 3265–3268. https://doi.org/10.1007/s00520-016-3272-5
Lebel, S., Tomei, C., Feldstain, A., Beattie, S., & McCallum, M. (2013). Does fear of cancer recurrence predict cancer survivors’ health care use? Supportive Care in Cancer, 21, 901–906. https://doi.org/10.1007/s00520-012-1685-3
Lengacher, C.A., Reich, R.R., Paterson, C.L., Ramesar, S., Park, J.Y., Alinat, C., . . . Kip, K.E. (2016). Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: A randomized controlled trial. Journal of Clinical Oncology, 34, 2827–2834. https://doi.org/10.1200/JCO.2015.65.7874
Lengacher, C.A., Shelton, M.M., Reich, R.R., Barta, M.K., Johnson-Mallard, V., Moscoso, M.S., . . . Kip, K.E. (2014). Mindfulness based stress reduction (MBSR[BC]) in breast cancer: Evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). Journal of Behavioral Medicine, 37, 185–195. https://doi.org/10.1007/s10865-012-9473-6
Lichtenthal, W.G., Corner, G.W., Slivjak, E.T., Roberts, K.E., Li, Y., Breitbart, W., . . . Beard, C. (2017). A pilot randomized controlled trial of cognitive bias modification to reduce fear of breast cancer recurrence. Cancer, 123, 1424–1433. https://doi.org/10.1002/cncr.30478
Lopez, C., Antoni, M., Penedo, F., Weiss, D., Cruess, S., Segotas, M.-C., . . . Fletcher, M.A. (2011). A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. Journal of Psychosomatic Research, 70, 328–334. https://doi.org/10.1016/j.jpsychores.2010.11.010
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D.G. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. BMJ, 339, b2535. https://doi.org/10.1136/bmj.b2535
Otto, A.K., Szczesny, E.C., Soriano, E.C., Laurenceau, J.-P., & Siegel, S.D. (2016). Effects of a randomized gratitude intervention on death-related fear of recurrence in breast cancer survivors. Health Psychology, 35, 1320–1328.
Peterson, C., Ruch, W., Beermann, U., Park, N., & Seligman, M.E.P. (2007). Strengths of character, orientations to happiness, and life satisfaction. Journal of Positive Psychology, 2, 149–156.
Sheldon, K.M., & Lyubomirsky, S. (2006). How to increase and sustain positive emotion: The effects of expressing gratitude and visualizing best possible selves. Journal of Positive Psychology, 1, 73–82. https://doi.org/10.1080/17439760500510676
Shi, Z., & MacBeth, A. (2017). The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: A systematic review. Mindfulness, 8, 823–847. https://doi.org/10.1007/s12671-016-0673-y
Shields, C.G., Ziner, K.W., Bourff, S.A., Schilling, K., Zhao, Q., Monahan, P., . . . Champion, V. (2010). An intervention to improve communication between breast cancer survivors and their physicians. Journal of Psychosocial Oncology, 28, 610–629. https://doi.org/10.1080/07347332.2010.516811
Siegel, R.L., Ma, J., Zou, Z., & Jemal, A. (2015). Cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 65, 9–29. https://doi.org/10.3322/caac.21208
Simard, S., Savard, J., & Ivers, H. (2010). Fear of cancer recurrence: Specific profiles and nature of intrusive thoughts. Journal of Cancer Survivorship, 4, 361–371. https://doi.org/10.1007/s11764-010-0136-8
Thewes, B., Bell, M.L., Butow, P., Beith, J., Boyle, F., Friedlander, M., & Mclachlan, S.A. (2013). Psychological morbidity and stress but not social factors influence level of fear of cancer recurrence in young women with early breast cancer: Results of a cross-sectional study. Psycho-Oncology, 22, 2797–2806. https://doi.org/10.1002/pon.3348
Turner, J., Zapart, S., Pedersen, K., Rankin, N., Luxford, K., & Fletcher, J. (2005). Clinical practice guidelines for the psychosocial care of adults with cancer. Psycho-Oncology, 14, 159–173. https://doi.org/10.1002/pon.897
van de Wal, M., Thewes, B., Gielissen, M., Speckens, A., & Prins, J. (2017). Efficacy of blended cognitive behavior therapy for high fear of recurrence in breast, prostate, and colorectal cancer survivors: The SWORD study, a randomized controlled trial. Journal of Clinical Oncology, 35, 2173–2183. https://doi.org/10.1200/JCO.2016.70.5301
Wagner, L.I., Duffecy, J., Lehman, K.A., Sanford, S.D., Begale, M., Nawacki, E., . . . Mohr, D.C. (2011, June). Randomized clinical trial to evaluate an e-health intervention for fear of cancer recurrence, anxiety, and depression among cancer survivors. Poster presented at the American Society of Clinical Oncology Annual Meeting.
Wolin, K.Y., & Colditz, G.A. (2011). Design and conduct of intervention-based research among cancer survivors. Cancer Epidemiology, Biomarkers and Prevention, 20, 2078–2084. https://doi.org/10.1158/1055-9965.EPI-11-0605
Zhang, J., Xu, R., Wang, B., & Wang, J. (2016). Effects of mindfulness-based therapy for patients with breast cancer: A systematic review and meta-analysis. Complementary Therapies in Medicine, 26, 1–10. https://doi.org/10.1016/j.ctim.2016.02.012

