Understanding Distress in the Hospital: A Qualitative Study Examining Adults With Cancer
Purpose: To measure the distress of hospitalized adults with cancer and identify strategies and behaviors to manage distress.
Participants & Setting: 185 adults with cancer hospitalized in a large tertiary hospital in the Midwest.
Methodologic Approach: This study involved a one-time assessment using the National Comprehensive Cancer Network’s (NCCN’s) Distress Thermometer and two open-ended questions. Demographic data were reviewed, and responses to open-ended questions were analyzed by content analysis. A team approach was used to develop and validate themes.
Findings: Strategies used by patients to manage distress were categorized as taking charge and embracing help. Helpful strategies were related to quality of life and relationship with care teams.
Implications for Nursing: Understanding of distress in hospitalized adults with cancer is limited, which warrants the attention of healthcare professionals. Study results have implications to enhance patient care and to address nationally established psychosocial care objectives and NCCN distress screening standards.
Jump to a section
Cancer presents a serious burden to society and is a life-changing diagnosis for millions of people in the United States. According to the U.S. Department of Health and Human Services, cancer is the second leading cause of death in the United States, exceeded only by heart disease (National Center for Health Statistics, 2016). The American Cancer Society (2017) reported that more than 15.5 million people were living with a cancer diagnosis in 2016.
Distress has been defined as “a multifactorial, unpleasant, emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment. Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears, to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis” (National Comprehensive Cancer Network [NCCN], 2016, p. DIS-2).
The assessment and treatment of distress as related to the patient with cancer are well represented in the literature and recognized by the professional cancer community. The NCCN (2016) maintains guidelines for distress management, and since 2015, the American College of Surgeons ([ACOS], 2012) Commission on Cancer has required cancer centers to screen for psychosocial distress as a requisite for accreditation. The American Psychosocial Oncology Society also values and promotes the comprehensive care of individuals with cancer.
The issue of distress has attracted serious attention for good reason. In a sample of 4,496 individuals with various cancers, overall prevalence of distress was 35% (Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001). Higher levels of distress have been correlated with clinical depression (Akizuki et al., 2003; Hegel et al., 2008). Increased distress and depression can lead to unfavorable outcomes, such as decreased medical adherence, reduced quality of life, increased length of hospital stay, higher healthcare costs, greater desire for death, and shortened survival (Bevans et al., 2011; Grassi, Caruso, Sabato, Massarenti, & Nanni, 2015; Han et al., 2015; Mergenthaler et al., 2011; Mitchell, 2007). The ACOS (2012, 2015) Commission on Cancer’s requirement for distress screening underscores the value and need for assessing the psychosocial health of people with cancer.
Although research aimed at understanding distress in patients with cancer is growing, most studies have been completed in the ambulatory setting (Agarwal et al., 2013; Blenkiron, Brooks, Dearden, & McVey, 2014; Jacobsen et al., 2005; Loquai et al., 2013). Information is limited regarding the distress of hospitalized patients with cancer (Bužgová, Hajnová, Sikorová, & Jarošová, 2014; Clark, 2010; Rosselli et al., 2015; Swanson & Koch, 2010). The purpose of the current study is to measure the distress levels of hospitalized adults with cancer, to identify the categories of distress they have, and to explore strategies and behaviors they use to manage distress. The long-term goals are to raise awareness by providing education to hospitals and inpatient healthcare staff about perspectives of distress among patients with cancer during hospitalization, to show the effect a provider’s interactions can have on a patient’s distress level, and to further explore and identify interventions to help patients manage distress during hospitalization.
Methods
This cross-sectional descriptive study was approved by the Mayo Clinic Institutional Review Board. The authors used qualitative and quantitative methods to address self-reported distress of hospitalized adults with cancer. Data were collected for seven months (from November 2013 to June 2014) from 185 hospitalized patients with cancer. Participants completed the NCCN’s Distress Thermometer and a visual analog scale, and they answered two additional open-ended questions once during hospitalization.
The convenience sample consisted of adults aged 18 years or older with cancer who were admitted to two inpatient oncology-hematology units at Mayo Clinic Hospital, Methodist Campus, in Rochester, Minnesota. Eligible participants were alert and oriented to person, place, and time and could read and write in English. Participants were surveyed once during a single hospitalization; readmitted patients were ineligible to participate. Because they were a convenience sample, patients were not approached at a set time during hospitalization but rather when staff and participants were available to meet.
A member of the research team approached eligible patients during their hospitalization. Patients provided verbal consent and demographic information before study participation. They were asked to rate their level of distress in the past seven days with the Distress Thermometer on a scale from 0 (no distress) to 10 (extreme distress). The Distress Thermometer has a sensitivity of 77% and a specificity of 66% when used as a single tool to evaluate psychosocial distress (Mitchell, 2007).
Two open-ended questions were asked of participants: “What are you currently doing to decrease your level of distress?” and “What would you find helpful during your hospitalization to decrease your level of distress?” Participants provided handwritten responses to each question, and responses were assigned to categories of strategies and behaviors used or preferred to manage distress. The current study focuses on the qualitative analysis of patient responses to these open-ended questions. The goal was to describe the patient perspective regarding current behaviors intended to alleviate distress and to identify opportunities for healthcare providers to improve distress management during hospitalization. All data were collected in the patients’ rooms during their hospital stay. On the rare occasion when a patient was too ill to independently complete the survey or requested otherwise, study team members scribed the answers, striving to keep responses as close to verbatim as possible.
All responses to the open-ended questions were transcribed and entered into a Microsoft Excel® spreadsheet. Principles of content analysis (Graneheim & Lundman, 2004) were used to guide qualitative analysis. Two independent groups of two team members each provided preliminary coding lists, with all codes emerging from participant data. The coding lists were discussed with the entire research team, who achieved consensus with initial coding categories. Each item described by participants was assigned a specific code by each team. Some participants described one item for each of the open-ended questions; some responded with several items. Only one code was assigned to each item. The research team placed all items into existing codes when logical but created new codes as needed. Overall categories for each open-ended question were then determined. Any discrepancies were decided on by group consensus.
The authors achieved credibility by sampling a wide range of patients to reflect depth and breadth in final themes and by engaging in rich discussions within the research team to achieve consensus. Findings are dependable in that data were extensive and analysis was discussed fully and openly among all team members. Data are transferrable to the extent of the authors’ full description of the culture and context for the study—namely, these data represent hospitalized adults receiving hematology-oncology care in the Midwest.
Findings
In total, 255 patients were assessed for study eligibility, and 59 patients were excluded for various reasons (see Figure 1). Completion of all study procedures was accomplished by 185 participants.

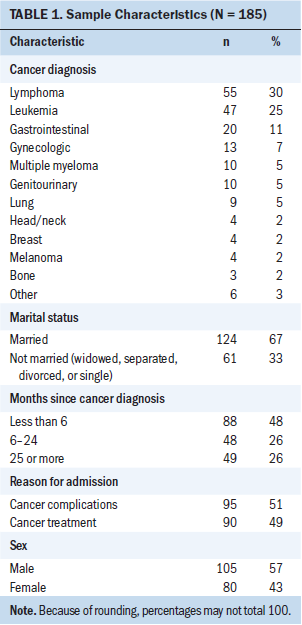
Participants were predominantly male and married (see Table 1). The mean age was 60.6 years (range = 19–95 years). About two-thirds of the patients had a hematologic malignancy; the others had solid tumors. Almost half of the patients had a diagnosis of cancer less than six months prior to their participation in the study. Participants were categorized into two groups based on their reason for hospital admission: a cancer complication (e.g., symptom management) or cancer treatment (e.g., scheduled chemotherapy).
Of the study participants, 52 completed the survey during the first day of their hospitalization and 83 completed it during the last day of their hospitalization. The other 50 participants completed the survey between the first and last day of hospitalization. Of note, as another descriptor of the sample, the mean distress score was 4.6, and the median was 5.
Various themes were determined by analyzing responses to the two questions: “What are you currently doing to decrease your level of distress?” and “What would you find helpful during your hospitalization to decrease your level of distress?” Some participants reported multiple strategies for both categories.
Question 1
Responses to “What are you currently doing to decrease your level of distress?” were represented in two categories: taking charge (n = 214) and embracing help (n = 101) (see Table 2). Of the 185 participants, 168 offered a response assignable to at least one category; some participants provided more than one answer to this question. Of note, 17 participants were categorized as responding “nothing” to this question. Responses in this category were “nothing,” no response, or a report of no distress.
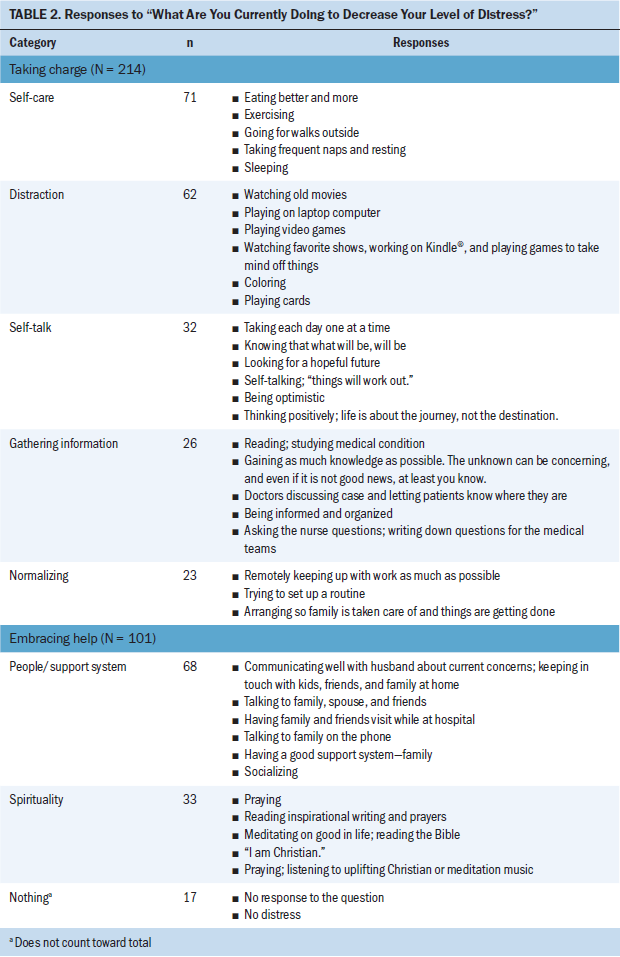
Taking charge: An overarching category, taking charge, emerged from the data as self-initiated and self-directed strategies by patients to manage their distress. Responses in this category encompassed activities the patients initiated rather than depending on others to do the activities for them.
Subcategories of taking charge were self-care, distraction, self-talk, gathering information, and normalizing. Self-care encompassed activities that patients did for their own well-being and health promotion and focused on nutrition, activity, and rest. Distraction included activities intended to take the focus off their illness. Self-talk was defined as positive reinforcement or encouragement to oneself, reflecting attitudes participants had adopted. Gathering information consisted of collecting knowledge or resources related to disease or treatment with the intent of being prepared. Normalizing was never explicitly noted by respondents but was classified by the research team as engaging in typical activities of daily life not related to hospitalization, such as work-related activities.
Embracing help: The embracing help category encompassed willingness of the patient to accept support from others and to look beyond him- or herself for help. This concept was reflected by interactions with others and included mutually beneficial activities that engaged and maintained relationships. Spirituality was included in this category as another means of support.
The subcategory of people/support system was defined as allowing others to assist with physical or emotional needs. This category was composed primarily of relationships with friends and family and of fostering communication necessary to maintain those relationships. Spirituality included activities intended to nurture the spirit. Reponses in this category were not exclusive to religious activities but included a broad range of activities related to an overall concept of spirituality.
Question 2
Responses to “What would you find helpful during your hospitalization to decrease your level of distress?” were assigned to the categories quality of life (n = 102) and relationship with care team (n = 105) (see Table 3). Among the 185 participants, 144 offered a response that could be placed in at least one of these categories. As with the first question, some participants provided more than one answer. Forty-one patient responses were assigned to the category “nothing.” Responses in that category included “nothing,” remarks specifying nothing beyond what is already being done, comments indicating that the patient did not know what would be helpful, the statement “can’t think of anything,” or no response at all.
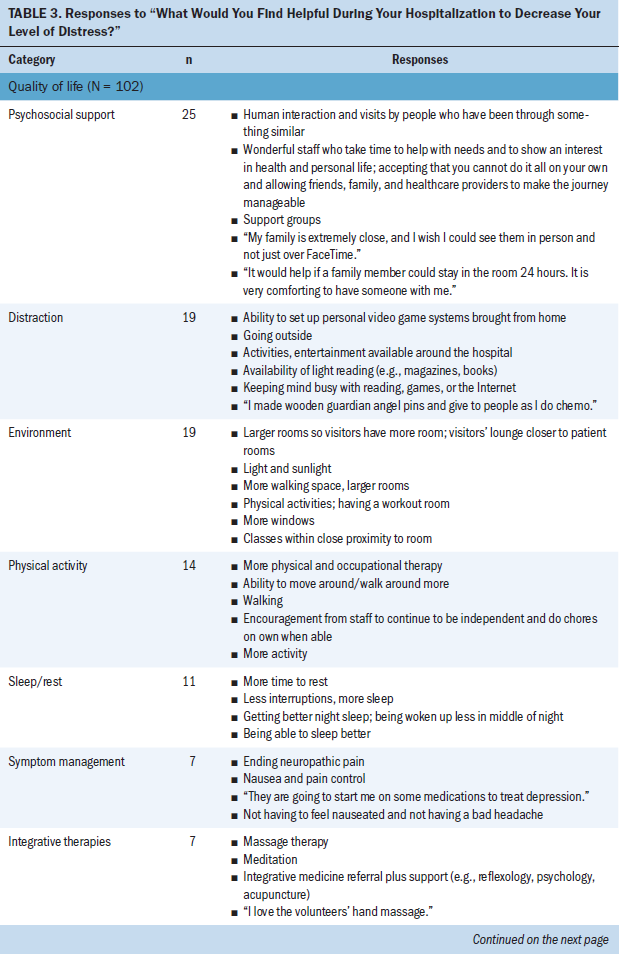
Quality of life: Quality of life included responses that fit domains common to quality of life—physical, psychological, social, and spiritual well-being. Sub-categories of quality of life were psychosocial support, distraction, environment, physical activity, sleep/rest, symptom management, and integrative therapies. Psychosocial support involved any comments directed at engagement in relationships with family and friends, with the engagement most often provided in person and intended to support the patient. Distraction included activities intended toshift patients’ attention away from their illness and were not hospital- or treatment-focused. Environment centered on the hospital setting and what patients could change or would like to change within their room or patient care unit to alleviate distress. Physical activity went beyond the immediate environment to include a space to mobilize, as well as the ability to do so. Sleep/rest entailed any strategy intended to promote rest, such as fewer interruptions by staff. Symptom management was defined as interventions aimed at alleviating symptoms like pain and nausea. Integrative or complementary therapies included treatments addressing overall well-being, such as massage and meditation.
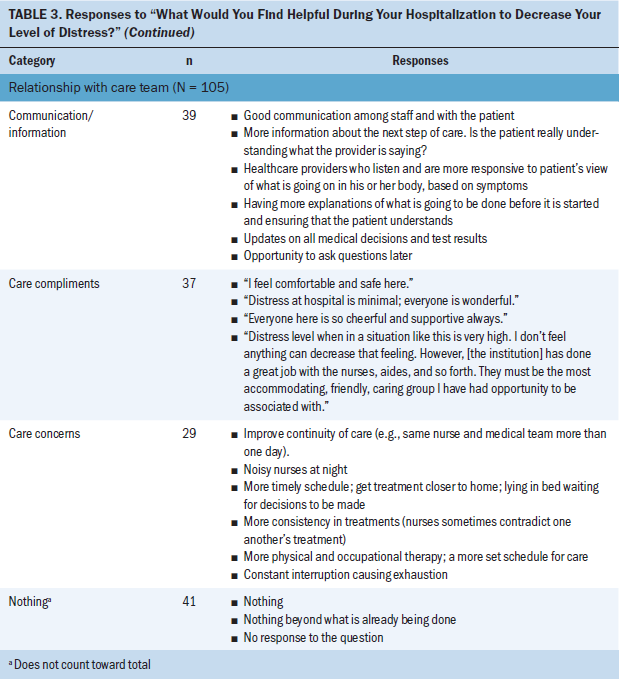
Relationship with care team: Relationship with care team was defined as the interaction or connection between the patients and the healthcare providers involved in their care during hospitalization. It did not single out any one discipline. Subcategories included communication/information, care compliments, care concerns, and nothing.
Communication/information included verbal and nonverbal information exchanged between the patient and the healthcare team; generally, more effective communication was desired. Care compliments included praise or positive feedback from patients about care, caregivers, or overall satisfaction with their hospital stay and included concepts like safety, kindness, and caring. Care concerns encompassed patient feedback, such as complaints and recommendations for improvement (e.g., the desire for better coordination, continuity of care, and rest by way of less noise).
Discussion
In this cross-sectional descriptive study, the authors examined self-reported distress in hospitalized adults with cancer (N = 185) and identified overall levels of distress at one time point during the hospital stay. With a mean distress score of 4.6, and a distress score of more than 4 as a criterion for intervention, most responses met the threshold for further assessment to identify specific needs (National Cancer Institute, 2015). In the current study, 115 of 185 participants (62%) reported a distress score of 4 or greater, compared with 275 of 1,205 participants (23%) (VanHoose et al., 2015) and 163 of 380 participants (43%) (Jacobsen et al., 2005) in studies conducted in the outpatient setting. This outcome suggests that hospitalization and increased acuity may be associated with a higher level of distress experienced by patients with cancer.
Although the hospital environment appears to contribute to elevated distress, understanding patient perspectives can help with identifying global patient preferences and the role of healthcare providers as it relates to managing distress in the hospital. The authors not only measured the distress level of adults hospitalized with cancer, but also explored strategies and behaviors they used to manage their distress and interventions they desired.
Patient responses were the foundation for this qualitative analysis and were represented in two categories for each question. Assigning individual responses to categories provides an opportunity for closer examination while patient behavior and preferences, as they relate to alleviating distress during hospitalization, are explored.
In response to the question “What are you currently doing to decrease your level of distress?” participants most frequently identified activities categorized as taking charge. These included activities that participants initiated themselves rather than depended on others to do for them. Kreitler, Peleg, and Ehrenfeld (2007) found that self-efficacy affects perceived stress, and when perceived stress is lower, quality of life improves for individuals with cancer. In the current study, participants specifically indicated that they were taking charge to decrease their level of distress.
The concept of embracing help, which included engagement in relationships and spirituality, also emerged as an important strategy for participants to decrease distress. Participants knew they could not always manage distress themselves, and they turned to others for help. Faller et al. (2016) cited the role of psychosocial support among patients with cancer in relation to emotional distress. In addition, the role of spirituality as a mitigating factor in the experience of cancer-related distress has been explored in the literature (Alcorn et al., 2010; Piderman et al., 2014).
Participant responses to the question “What would you find helpful during your hospitalization to decrease your level of distress?” have implications for even more direct influence by the healthcare team. Psychosocial support, distraction, environment, physical activity, sleep/rest, symptom management, and complementary and integrative therapies were identified as being important to quality of life. Managing pain, fatigue, and depression, as well as meeting psychological and spiritual needs, are important to address multiple domains of quality of life for hospitalized patients with cancer (Bužgová et al., 2014). The physical hospital environment, the social interactions between patients and staff, and the ability of family members to be present can also affect patients’ hospital experience (Robinson, Gott, Gardiner, & Ingleton, 2015) and is reflected by similar suggestions of participants in the current study.
A second category, relationship with care team, was predominantly represented by responses pertaining to communication and information. Swanson and Koch (2010) found that distress scores were lower at hospital dismissal when an oncology nurse navigator facilitated communication and understanding among patients, families, and the interprofessional team, providing a consistent message from the healthcare team—a strategy that participants in the current study would likely endorse. This relationship with the care team also can be enhanced by genuine face-to-face contact. The quality of connection with staff could “make or break a patient’s stay” (Shattell, Hogan, & Thomas, 2005, p. 161).
One unanticipated subcategory that emerged was care compliments. The authors speculated that participants may have seen the survey as an opportunity to compliment the care team. Other participants took the opportunity to voice appropriate care concerns.
In addition, the authors noted several interesting connections between categories and subcategories for the two questions. For example, the distraction subcategory emerged as important for current and desired strategies to decrease levels of distress. This finding demonstrated the importance of access to and availability of resources and entertainment strategies, such as watching television, playing video games, reading, and having Internet access, which nonhospitalized people may take for granted. The authors also noted that the relationship with the care team can affect a person’s ability to take charge; basic human contact with the healthcare team can increase personal security and power for patients in an environment that often can seem uncaring, confusing, and not to be trusted (Shattell et al., 2005). Although similarities were observed between categories and subcategories for the two questions, the category names emerged from the responses given by participants. Therefore, they differ slightly, which is congruent with qualitative methods, in which data analysis uses language provided by the respondent.
Strengths and Limitations
This study adds actionable findings to the literature that address distress in hospitalized patients with cancer. The authors not only obtained a numerical reading of distress and sought to understand the patient perspective and actionable items to manage distress, but also identified categories of distress management strategies used by patients, as well as opportunities for the inpatient healthcare team to support management of distress, through data collected directly from patients in the hospital environment. Patients with various hematologic and oncologic diagnoses were included in this study, adding to the generalizability of the findings.
The current authors assessed distress at a single time point during a patient’s hospital stay. Because distress can occur at any point during the cancer trajectory, screening should be conducted at more than one time point (Institute of Medicine, 2008). However, it can be argued that the current hospitalization encompassed one episode of care in the entire continuum of cancer care. In addition, distress was assessed without correlation to length of stay. For example, an assessment of distress on day 3 of a hospital stay could reveal different results than an assessment on day 30, and individuals could identify different distress management strategies depending on how long they had been in the hospital. The sample in the current study was drawn from one Midwest hospital, which may limit the generalizability of the results to other geographic areas. A cross-cultural understanding of distress could be facilitated by associating scores with various racial and ethnic backgrounds and including patients who do not speak English.
Implications for Nursing
Findings in this study suggest that adults with cancer have higher levels of distress during hospitalization than in the ambulatory setting. These levels warrant further attention. Nurses are vital in the coordination of patient care and are positioned to identify and assess patient distress early and often. Nurses can directly provide support to help patients manage distress while hospitalized (Swanson & Koch, 2010). Practical applications from this study suggest that cultivation of an environment where patients are empowered to take charge can be meaningful, particularly in a setting with frequent interruptions, inflexible schedules, limited space, and diminished patient independence. Nursing staff can also be instrumental in facilitating communication to identify specific patient needs and elicit the support of the most appropriate member of the healthcare team. The role of the inpatient nurse to assess and respond to the distress of individuals with cancer presents an opportunity for further examination and research.
A healthcare team that empathizes with patients regarding the challenges of the hospital setting allows for an opportunity to intentionally engage patients in identifying meaningful ways to maintain a sense of autonomy within the hospital setting. Taking charge can be empowering for patients during the cancer experience, when personal control is limited. This opportunity may translate to providers simply communicating that they have time for the patient to ask questions or arranging protected time for the patient to rest during the day after a sleepless night. The taking charge category may be represented in behaviors independent from the healthcare team. Healthcare professionals can support and help facilitate patients’ ability to influence their environment and care, which can be personally empowering and affirming of the specific needs of patients.
The embracing help category also may be independent of the healthcare team. Assistance for patients to navigate potential barriers to stay connected with other people while hospitalized should not be underestimated. From a practical standpoint, this assistance may translate to helping patients access technology to stay in electronic or video contact with family, making accommodations for a loved one to spend the night, or helping to celebrate a special day. The many benefits of responding to the spiritual needs of patients affected by cancer are well documented (Alcorn et al., 2010; Piderman et al., 2014) and should entail an interprofessional effort among nurses, social workers, chaplains, physicians, and other members of the healthcare team to meet patients’ spiritual needs.
[[{"type":"media","view_mode":"media_original","fid":"39971","attributes":{"alt":"","class":"media-image","height":"183","typeof":"foaf:Image","width":"314"}}]]
Conclusion
Healthcare professionals care for people with cancer in the acute hospital setting (when distress levels may be higher than in the ambulatory setting) during a distinct and often pivotal time of illness. In a managed healthcare system that increasingly promotes brief hospital stays, the need to quickly identify distress and use a focused treatment approach is more important than ever.
In the current study, hospitalized adults with cancer told the authors about the strategies they were using and the strategies they would find helpful to decrease distress. Results may assist healthcare professionals in helping patients target effective strategies to manage distress in the hospital. Understanding distress and its management may help guide future psychosocial needs assessments and interventions to improve patient satisfaction during hospitalization, as well as promote patient quality of life.
About the Author(s)
Heather Stonelake-French, MS, APRN, CNS, is a clinical nurse specialist, Brent E. Moos, MSW, LICSW, is a hospice social worker, Carol M. Brueggen, MS, APRN, CNS, is a clinical nurse specialist, Erin L. Gravemann, MSW, LICSW, is a medical social worker, Amy L. Hansen, MS, APRN, CNS, and Jeanne M. Voll, MS, APRN, CNS, are clinical nurse specialists, and Ann M. Dose, PhD, APRN, CNS, is a nurse scientist, all in the Department of Nursing at the Mayo Clinic in Rochester, MN. Stonelake-French, Moos, Brueggen, Gravemann, Hansen, and Voll contributed to the conceptualization and design and completed the data collection. Stonelake-French, Moos, Brueggen, Hansen, Voll, and Dose contributed to the manuscript preparation. All authors provided the analysis. Writing and editorial support were provided by the Section of Scientific Publications through support from Mayo Clinic. Stonelake-French can be reached at stonelake.heather@mayo.edu, with copy to ONFEditor@ons.org. (Submitted July 2017. Accepted September 22, 2017.)
References
Agarwal, J., Powers, K., Pappas, L., Buchmann, L., Anderson, L., Gauchay, L., & Rich, A. (2013). Correlates of elevated Distress Thermometer scores in breast cancer patients. Supportive Care in Cancer, 21, 2125–2136. https://doi.org/10.1007/s00520-013-1773-z
Akizuki, N., Akechi, T., Nakanishi, T., Yoshikawa, E., Okamura, M., Nakano, T., . . . Uchitomi, Y. (2003). Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer, 97, 2605–2613. https://doi.org/10.1002/cncr.11358
Alcorn, S.R., Balboni, M.J., Prigerson, H.G., Reynolds, A., Phelps, A.C., Wright, A.A., . . . Balboni, T.A. (2010). “If God wanted me yesterday, I wouldn’t be here today”: Religious and spiritual themes in patients’ experiences of advanced cancer. Journal of Palliative Medicine, 13, 581–588. https://doi.org/10.1089/jpm.2009.0343
American Cancer Society. (2017). Cancer facts and figures, 2017. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American College of Surgeons. (2012). Cancer program standards 2012: Ensuring patient-centered care. Retrieved from https://www.facs.org/~/media/files/quality%20programs/cancer/coc/progra…
American College of Surgeons. (2015). Cancer program standards: Ensuring patient-centered care. Retrieved from https://www.facs.org/~/media/files/quality%20programs/cancer/coc/2016%2…
Bevans, M., Wehrlen, L., Prachenko, O., Soeken, K., Zabora, J., & Wallen, G.R. (2011). Distress screening in allogeneic hematopoietic stem cell (HSCT) caregivers and patients. Psycho-Oncology, 20, 615–622. https://doi.org/10.1002/pon.1906
Blenkiron, P., Brooks, A., Dearden, R., & McVey, J. (2014). Use of the Distress Thermometer to evaluate symptoms, outcome and satisfaction in a specialist psycho-oncology service. General Hospital Psychiatry, 36, 607–612. https://doi.org/10.1016/j.genhosppsych.2014.06.003
Bužgová, R., Hajnová, E., Sikorová, L., & Jarošová, D. (2014). Association between unmet needs and quality of life in hospitalised cancer patients no longer receiving anti-cancer treatment. European Journal of Cancer Care, 23, 685–694. https://doi.org/10.1111/ecc.12181
Clark, P.G. (2010). Decreasing psychological distress in cancer inpatients using FLEX Care®: A pilot study. Social Work in Health Care, 49, 872–890. https://doi.org/10.1080/00981389.2010.499826
Faller, H., Koch, U., Brähler, E., Härter, M., Keller, M., Schulz, H.,. . . Mehnert, A. (2016). Satisfaction with information and unmet information needs in men and women with cancer. Journal of Cancer Survivorship, 10, 62–70. https://doi.org/10.1007/s11764-015-0451-1
Graneheim, U.H., & Lundman, B. (2004). Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24, 105–112. https://doi.org/10.1016/j.nedt.2003.10.001
Grassi, L., Caruso, R., Sabato, S., Massarenti, S., & Nanni, M.G. (2015). Psychosocial screening and assessment in oncology and palliative care settings. Frontiers in Psychology, 5, 1485. https://doi.org/10.3389/fpsyg.2014.01485
Han, X., Lin, C.C., Li, C., de Moor, J.S., Rodriguez, J.L., Kent, E.E., & Forsythe, L.P. (2015). Association between serious psychological distress and health care use and expenditures by cancer history. Cancer, 121, 614–622. https://doi.org/10.1002/cncr.29102
Hegel, M.T., Collins, E.D., Kearing, S., Gillock, K.L., Moore, C.P., & Ahles, T.A. (2008). Sensitivity and specificity of the Distress Thermometer for depression in newly diagnosed breast cancer patients. Psycho-Oncology, 17, 556–560. https://doi.org/10.1002/pon.1289
Institute of Medicine. (2008). Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: National Academies Press.
Jacobsen, P.B., Donovan, K.A., Trask, P.C., Fleishman, S.B., Zabora, J., Baker, F., & Holland, J.C. (2005). Screening for psychologic distress in ambulatory cancer patients. Cancer, 103, 1494–1502. https://doi.org/10.1002/cncr.20940
Kreitler, S., Peleg, D., & Ehrenfeld, M. (2007). Stress, self-efficacy and quality of life in cancer patients. Psycho-Oncology, 16, 329–341. https://doi.org/10.1002/pon.1063
Loquai, C., Scheurich, V., Syring, N., Schmidtmann, I., Rietz, S., Werner, A., . . . Beutel, M.E. (2013). Screening for distress in routine oncological care—A survey in 520 melanoma patients. PLOS ONE, 8(7), e66800. https://doi.org/10.1371/journal.pone.0066800
Mergenthaler, U., Heymanns, J., Köppler, H., Thomalla, J., van Roye, C., Schenk, J., & Weide, R. (2011). Evaluation of psychosocial distress in patients treated in a community-based oncology group practice in Germany. Annals of Oncology, 22, 931–938. https://doi.org/10.1093/annonc/mdq455
Mitchell, A.J. (2007). Pooled results from 38 analyses of the accuracy of Distress Thermometer and other ultra-short methods of detecting cancer-related mood disorders. Journal of Clinical Oncology, 25, 4670–4681.
National Cancer Institute. (2015). What is cancer? Retrieved from https://www.cancer.gov/about-cancer/understanding/what-is-cancer
National Center for Health Statistics. (2016). Health, United States, 2015: With special feature on racial and ethnic health disparities. Retrieved from https://www.cdc.gov/nchs/data/hus/hus15.pdf
National Comprehensive Cancer Network. (2016). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Distress management [v.2.2016]. Retrieved from http://oncolife.com.ua/doc/nccn/NCCN_Distress_Management.pdf
Piderman, K.M., Johnson, M.E., Frost, M.H., Atherton, P.J., Satele, D.V., Clark, M.M., . . . Rummans, T.A. (2014). Spiritual quality of life in advanced cancer patients receiving radiation therapy. Psycho-Oncology, 23, 216–221. https://doi.org/10.1002/pon.3390
Robinson, J., Gott, M., Gardiner, C., & Ingleton, C. (2015). The impact of the environment on patient experiences of hospital admissions in palliative care. BMJ Supportive and Palliative Care. Advance online publication. https://doi.org/10.1136/bmjspcare-2015-000891
Rosselli, M., Salimbeni, M.V., Bessi, C., Nesi, E., Caruso, S., Arboretti, D., . . . Stasi, C. (2015). Screening of distress among hospitalized patients in a department of internal medicine. Asian Journal of Psychiatry, 18, 91–96. https://doi.org/10.1016/j.ajp.2015.08.003
Shattell, M., Hogan, B., & Thomas, S.P. (2005). “It’s the people that make the environment good or bad”: The patient’s experience of the acute care hospital environment. AACN Clinical Issues, 16, 159–169.
Swanson, J., & Koch, L. (2010). The role of the oncology nurse navigator in distress management of adult inpatients with cancer: A retrospective study. Oncology Nursing Forum, 37, 69–76. https://doi.org/10.1188/10.ONF.69-76
VanHoose, L., Black, L.L., Doty, K., Sabata, D., Twumasi-Ankrah, P., Taylor, S., & Johnson, R. (2015). An analysis of the Distress Thermometer problem list and distress in patients with cancer. Supportive Care in Cancer, 23, 1225–1232. https://doi.org/10.1007/s00520-014-2471-1
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C., & Piantadosi, S. (2001). The prevalence of psychological distress by cancer site. Psycho-Oncology, 10, 19–28.




