Not a Death Sentence: Perspectives of African American Women Living With Lung Cancer
Purpose: To conduct a descriptive, qualitative study to describe the experience of female African American lung cancer survivors, their perception of living with lung cancer, and their desire and ability to adopt positive health-related behaviors.
Participants & Setting: The sample consisted of 18 African American women with a history of stages I–IIIa lung cancer. Three focus groups were conducted in a private conference center in two community hospitals in the southeastern United States.
Methodologic Approach: A 20-item questionnaire was used to collect demographic, health status, and behavior information. A trained moderator led the audio-recorded focus group discussions using a semistructured interview guide.
Findings: Thematic analysis of the professionally transcribed data resulted in identification of four major themes. In addition, participants experienced stigma that influenced their perspectives on living with lung cancer.
Implications for Nursing: Healthcare professionals should provide culturally tailored communication and support for female African American lung cancer survivors. Additional research is needed to inform the development of interventions focused on health behavior change to enhance lung cancer survivorship in this vulnerable and understudied group.
Jump to a section
Lung cancer is the second leading type of cancer among adults and accounts for 25% of all cancer deaths in the United States (American Cancer Society, 2017). In 2017, an estimated 225,000 new cases of lung cancer were diagnosed in the United States, and 155,000 people died as a result of that diagnosis (American Cancer Society, 2017). These lung cancer incidence and mortality rates are startling. Even more disconcerting are the health disparities experienced by African Americans diagnosed with lung cancer. Although early detection, screening practices, and improved treatment help increase survival rates, the overall five-year survival rate of African American patients with lung cancer (14%) is lower than that of Caucasian patients (18%) (American Cancer Society, 2016a). When cancer is diagnosed prior to metastasis, the disparity is even greater, with the five-year survival rates increasing to 47% for African Americans and 55% for Caucasians, respectively (American Cancer Society, 2016b; de Moor et al., 2013). Despite this notable disparity, knowledge is limited regarding the survivorship of African Americans, particularly African American women, with lung cancer. This knowledge gap translates to a lack of understanding of the experiences of this vulnerable and understudied population. Therefore, research that generates a deeper understanding of survivorship among African American women with lung cancer is imperative. To address this gap in the research, this study aims to describe the experiences of female African American lung cancer survivors regarding their perception of living with lung cancer and their desire and ability to adopt health-related behaviors.
Important factors related to survivorship in this population include investigation into reducing risk behaviors associated with cancer, such as tobacco use, poor nutrition, lack of exercise, and ineffective stress management. Reducing these behaviors improves overall quality of life (QOL) and survival rates among all cancer survivors (McDonnell, Bullock, Hollen, Heath, & Kozower, 2014; Parsons, Daley, Begh, & Aveyard, 2010). Evidence shows that a cancer diagnosis provides substantial motivation for some individuals to embrace behavioral changes (Campo et al., 2011; Hawkins et al., 2010). However, little is known about cancer-related risk behaviors among female African American lung cancer survivors.
Eighty percent of individuals with a lung cancer diagnosis are former or current smokers (Park et al., 2012). For lung cancer survivors, continuing to smoke cigarettes negatively affects QOL, decreases lung capacity, increases the risk for comorbid diseases, and increases the mortality rate (Garces et al., 2004; McDonnell et al., 2014). Other unhealthy behaviors often accompany smoking, including lower physical activity levels, poor nutrition, and ineffective skills for self-management (Noble, Paul, Turon, & Oldmeadow, 2015).
Adopting a physical activity regimen is challenging for individuals with lung cancer because of physical symptoms. Krebs et al. (2012) evaluated 183 early-stage lung cancer survivors (n = 171 White non-Hispanic) and found that 10 continued to smoke and about 83 engaged in moderate to strenuous activity, but 158 were unable to meet the American Cancer Society’s recommended 150 minutes of moderate exercise per week for cancer survivors. Forty-five members of this sample did not engage in any recommended physical activity.
The American Cancer Society’s dietary recommendations for cancer survivors include maintaining a healthy weight; consuming a diet high in fruits, vegetables, and whole grains; decreasing intake of processed meat and red meat; and maintaining a low-fat diet (Rock et al., 2012). Cooley et al. (2013), in a study of 37 individuals with lung cancer and their family members (5 African Americans), found that 34 patients had low fruit and vegetable intake and more than half were overweight.
Lung cancer survivors experience a higher level of psychological distress, such as depression and anxiety, compared to other cancer survivors (Brown Johnson, Brodsky, & Cataldo, 2014; Cataldo, Slaughter, Jahan, Pongquan, & Hwang, 2011; Chambers et al., 2012, 2015; Chapple, Ziebland, & McPherson, 2004; Gonzalez & Jacobsen, 2012; Hamann et al., 2014). Psychological distress is strongly associated with physical symptoms (e.g., fatigue, shortness of breath, pain) and social challenges (e.g., shame, guilt, blame). Managing these psychological distresses involves the ability to cope with physical and social challenges, which may improve QOL.
In the United States, African American women in general have a higher incidence of consuming diets high in fat and low in fruits and vegetables. They experience an increased prevalence of obesity and do not participate in regular exercise regimens compared to White women (National Center for Health Statistics, 2016). In addition, compared to White women, African American women are more vulnerable to the development of mental health issues, such as anxiety and depression, and lack access to effective treatment for these mental health issues (National Center for Health Statistics, 2016). These individual determinants affect overall health for African American women and may affect those living with lung cancer (Belgrave & Abrams, 2016; National Center for Health Statistics, 2016).
Although evidence related to QOL and health- related behaviors among lung cancer survivors exists, the current study provides a greater understanding of factors that influence African American women with lung cancer. This information is important because factors that hinder behavior change can negatively affect survival rates in this population.
Methods
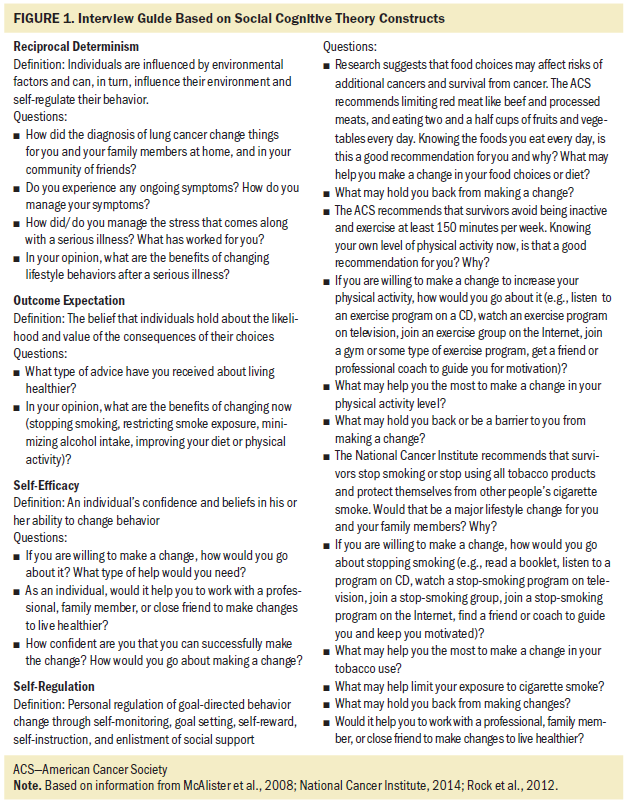
Principles of social cognitive theory (SCT) guided the study design. SCT seeks to explain why and how people change health behaviors and focuses on individuals’ potential to construct and alter their environment (McAlister, Perry, & Parcel, 2008). Key constructs explored were reciprocal determinism, outcome expectation, self-efficacy, and self-regulation (see Figure 1).
The focus group design was used to explore the broad topics of behavior change and living with lung cancer. The researchers chose focus group discussions instead of one-on-one interviews to enhance the participants’ ability to interact with one another and share their ideas. This group dynamic allowed participants to share ideas and respond to thoughts and comments, which fostered discussion and enrichment of data (Gray, 2009).
Three focus groups were conducted on three different dates in a private conference location at two large community hospitals in South Carolina. A convenience sample of 18 women was recruited. To be eligible for the study, participants had to be African American women with a documented lung cancer diagnosis (stages I–IIIa) within the past seven years (2008–2014). After obtaining approval from two institutional review boards affiliated with cancer programs approved by the American College of Surgeons, the researchers reviewed data from the programs’ cancer registries. A one-page, culturally sensitive, visually attractive recruitment flyer was mailed to 65 potential participants. This invitation included a toll-free number for participants to respond to or to request additional information. A research coordinator made follow-up calls and reminded interested participants about the dates for the focus group meeting.
After giving informed consent, potential participants completed a 20-item hard-copy questionnaire with pen and paper that included information about their demographics, household, and health status. Five questions from the Behavioral Risk Factor Surveillance System requested data about specific health behaviors. Each participant received $50 at the end of the focus group encounter.
A series of scripted, open-ended questions derived from SCT key constructs were used to probe participants about their experience of living with lung cancer and about health risk behaviors such as tobacco use, secondary smoke exposure, poor nutritional choices, lack of exercise, and ineffective stress management. Each session was facilitated by an experienced African American moderator, who used a semistructured interview guide to collect data. A research assistant made direct observations and took notes during each focus group to capture tone and nonverbal communication (Marshall & Rossman, 2011; Stewart & Shamdasani, 1990). All discussions were audio recorded and professionally transcribed.
Two researchers used a thematic analysis method developed by Braun and Clarke (2006) to review the transcripts. The researchers engaged in an iterative process of reading and analyzing the transcriptions. They coded the transcriptions line by line and grouped the data into specific categories. The categories were summarized and analyzed. The researchers identified themes independently. Then they collectively discussed the processes and interpretations and reconciled any differences until there was congruence of the identified categories. Upon data saturation, data analysis was considered complete and the themes were finalized. IBM SPSS Statistics, version 24.0, was used to analyze the questionnaire data and record the sample characteristics.
Results
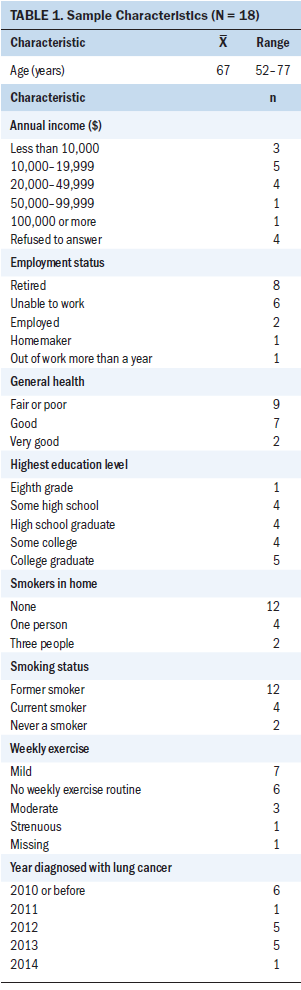
The study sample consisted of 18 African American women aged 52–77 years. Among the survivors, six were long-term survivors (diagnosed before 2010) and six were more recent survivors (diagnosed in 2013 or later). Most participants had at least a high school education. Of these, some had a college degree. Only a few of the 18 survivors were current smokers, lived with other smokers, and allowed smoking in their homes. Most participants stopped smoking either prior to their diagnosis or immediately following the lung cancer diagnosis. Two were never smokers (see Table 1). Fifteen people had one to three servings of beans per week; three did not. Two participants had five or more servings of fruit and vegetables per week, whereas 16 participants did not.
Qualitative data analysis resulted in the identification of four salient themes: (a) living proof that lung cancer is not an automatic death sentence, (b) learning to live with burdensome symptoms, (c) communication barriers affect self-care, and (d) African American women need to support one another.
Theme 1
Participants verbalized that a lung cancer diagnosis did not equate to imminent death. However, the response from friends, family, and healthcare professionals left survivors desperately wanting a more optimistic attitude and outlook regarding their disease state. Survivors perceived that others viewed their disease as debilitating and expected their physical appearance to reflect this. One participant commented, “When my doctor sees me, he says, ‘Oh, my God. You’re still alive? I can’t believe it!’ People expect me to look like I’m at death’s door. They ask, ‘Why do you look so good?’”
The survivors acknowledged that the diagnosis of lung cancer was difficult to accept and changed their lives. They expressed that family love and support were the most important factors in maintaining a positive outlook. One participant expressed the need to live her life the best she could: “I have a lot of living to do. And if the doctor told me I had six months, I’m gonna do five months’ worth of living.” Another participant stated, “I’m not going to let this hold me down.”
Beyond medical treatment, survivors needed more compassion, support, and understanding from their oncology care providers, family, and friends. Participants felt responsible for developing lung cancer. One participant expressed, “Lung cancer is, excuse me, the bastard of all cancers. You did it to yourself.” Participants expressed that some friends and family, as well as healthcare professionals, did not understand the strong addiction to tobacco, which affected the way they viewed the patients and their diagnosis. “We already know there is stigma on our disease because they say it’s the dirty disease, because we brought it on ourselves.” Another participant echoed the same thought: “When you tell someone you have lung cancer, they are like, ‘Did you smoke? Well, you brought this on yourself.’” Another participant stated, “My doctor [did] not understand how hard it is to quit smoking. He never offered me help to quit.” One participant refrained from sharing her diagnosis with close family and friends; she explained, “I never admit[ted] that I got lung cancer to my family or friends.”
Theme 2
Participants reported persistent burdensome symptoms that affected their daily lives. These symptoms stemmed from the disease process, treatment modalities, or other underlying disease processes. Symptoms reported included dyspnea, fatigue, and pain. Survivors expressed that they were unaware of and unprepared for some of the symptoms they endured after surgical, chemotherapeutic, and/or radiation treatments. Several participants commented on this matter as follows: “I’m short of breath all the time”; “I can’t put one foot in front of the other because it does take my energy away from me”; “The radiation left scar tissue. It’s painful all the time”; “The tiredness is unexplainable”; “The doctor did not tell me once . . . that I was going to have scar tissue [from the radiation].”
These symptoms not only altered participants’ daily lives, but also caused stress and influenced their ability to adopt healthy behaviors. The women wanted to know about exercises specifically tailored to those with lung cancer, including exercises that assist with daily living and that reduce stress and anxiety. They received no information or referrals to resources like palliative care and pulmonary rehabilitation to help them manage their burdensome symptoms.
Participants mentioned difficulty with physical activity, as evidenced by the following comments: “Well, I do walk, but I have to stop and rest”; “I have pain in my legs, and I get very tired”; “I walked around a little at the mall. I was so proud. The next morning, I could not get up. I had to go to the doctor.”
Theme 3
Participants expressed the need for better understanding about their disease process and expected outcomes of treatment. This lack of information negatively affected their ability to care for themselves. They conveyed that they desired to adopt healthy lifestyle changes. However, healthcare providers’ communication and services were incomplete, and the participants expressed disappointment that they had not been not given the tools or offered resources to adequately self-regulate their health. Participant comments included the following:
They should not write me off. Let me know [that] if I walk 10 steps, I’m going to have a hard time breathing.
My doctor did not send me to a nutritionist. When I asked, it was like, “Why do you want to know that?”
I think I need to learn more. I don’t think I’m getting what I need so that I can fight this battle. Right now, I’m fighting it alone.
Participants were vocal about their frustration with lack of understandable communication from healthcare professionals regarding their cancer diagnosis and symptom management. They felt that the lack of guidance for daily living led them to seek information from family and friends or attempt to solve issues on their own. The participants expressed a desire for clearer verbal and written communication from their encounters with their care providers, shown by the following comments:
Some of the words they use, medical terms—break it down a little bit so I can understand.
They just give you a pamphlet and send you on your way.
Doctors think that we’re not capable of comprehending what they’re talking about. Well, tell me anyways, and I will find somebody to explain it to me.
Theme 4
Study participants collectively expressed a need to learn from and support other female African American lung cancer survivors. They felt that peer support would help them cope with the physical, psychological, and social challenges. A collective effect would be to decrease their isolation and boost their self-efficacy and self-regulation regarding the adoption of healthy behaviors. Participants desired to share practical ideas to assist others with the adoption of the American Cancer Society recommended exercise and healthy diet options appropriate for those with a lung cancer diagnosis to improve their overall health and prevent cancer recurrence. They also thought that a support group would allow them to communicate their concerns, inquire about treatment options, and give them time to socialize and learn from one another. Participants’ comments included the following:
“I’m looking for a group of women of color who have lung cancer”; “If we are around one another, we are going to listen. Our ears are going to be open”; “I would like an exercise group for us, like cycling or tai chi, to help with stress”; “If we can just have a group where it’s just us.”
Discussion
Viewed from a SCT perspective, individual and environmental factors clearly influenced behavioral changes among these African American women living with lung cancer (McAlister et al., 2008). Their stories revealed ways in which they were deterred from healthy behavior change because of burdensome symptoms; communication barriers, which affected self-care and self-regulation; and lack of peer support. The diagnosis of lung cancer had altered their perspectives on life and their approaches to maintaining health, including behavioral modifications. The collective discussions that occurred in the three focus groups provided evidence of some degree of successful adoption of health behaviors and an openness to finding ways to improve their ability to conduct day-to-day activities and, ultimately, to prolong their lives. They were confident that behavior change could occur when needed resources were provided and available to assist with behavior change.
Participants believed that the lung cancer diagnosis was not an automatic death sentence, and they intended to live the best life possible. Some viewed it as a daily fight to survive; others viewed it as taking life one day at a time. These women assumed accountability and personal responsibility for the development of lung cancer, recognizing the behaviors that had contributed to their illness and consequently experiencing feelings of guilt, regret, and self-blame, as well as feeling they were being held responsible for their diagnosis by friends, family, healthcare professionals, and society. Although most acknowledged the importance of family assistance and support to assist with daily coping and maintaining a positive outlook, a few noted that the stigma led them to keep the diagnosis a secret. These women’s reports of stigma and its effect on their daily lives reflect findings from other research (Brown Johnson et al., 2014; Cataldo et al., 2011; Chambers et al., 2012, 2015; Chapple et al., 2004; Gonzalez & Jacobsen, 2012; Hamann et al., 2014).
Smoking cessation remains a tremendous challenge for some individuals with lung cancer (Cooley et al., 2009). Continued cigarette smoking and secondhand exposure complicate the recovery process and long-term QOL (McDonnell et al., 2014). Successful long-term smoking cessation is correlated with increased self-efficacy and improved symptom management, which may be achievable with behavioral intervention and pharmacotherapy (Cooley et al., 2012). In the current study, the women who continued to smoke recognized the consequences of their behavior and expressed guilt and self-blame. They desired to stop smoking but lacked the confidence and a strategy to self-regulate their smoking behaviors.
Physical symptoms greatly affected the survivors’ ability to incorporate exercise into their life. One-third of the participants were not engaged in any regular weekly exercise routine. Burdensome physical symptoms are common among lung cancer survivors, and self-care is the greatest challenge for many. Shortness of breath, pain, and fatigue, as single symptoms or a cluster, restrict the type and level of daily activity, which adversely affects QOL (Houlihan & Tyson, 2012). Other studies revealed similar results (Brown, Cooley, Chernecky, & Sarna, 2011; Coups et al., 2009; Krebs et al., 2012), although their samples lacked sufficient representation of African American women with lung cancer.
Survivors in the current study expressed interest in adopting a healthy diet. They voiced their desire to understand the recommended diet for cancer survivors for their overall health. However, the results from the questionnaire indicated that only a few ate five or more servings of fruits and/or vegetable per week. This is well below the American Cancer Society’s recommendation of five servings of fruit or vegetables daily or 35 servings or more per week (Rock et al., 2012). Written communications from healthcare providers regarding healthy dietary changes were ineffective according to the participants. A few participants reported not receiving any dietary information from their healthcare providers and, instead, were left on their own to decide what was appropriate for them to eat. Lack of guidance and education significantly influences the adoption of healthy dietary changes (Kenzik, Pisu, Fouad, & Martin, 2016). The participants voiced a need for consultation with a professional who could assist them with adopting dietary recommendations. They also expressed the need to elicit suggestions from other peers with lung cancer regarding healthy food options that were common in their culture and community, and regarding other topics to assist with necessary behavioral change.
Participants indicated a strong preference for developing peer-based support services for African American women with lung cancer. They desired to obtain support from similar women who would understand their experience living with this disease. They felt they could learn from one another, share information, and recommend resources. They noted that a peer support group would provide an opportunity to be honest and open about their concerns and challenges related to their health and could potentially help decrease their anxiety and promote healthy lifestyle options.
Physical symptoms, along with feelings of guilt, self-blame, and regret related to stigma, increase psychological distress, such as anxiety and depression (Brown Johnson et al., 2014; Cataldo et al., 2011; Chambers et al., 2012, 2015; Chapple et al., 2004; Gonzalez & Jacobsen, 2012; Hamann et al., 2014). The current group of women expressed frustration and disappointment because of the lack of helpful healthcare provider communication. Because their physical symptoms were the most challenging issues related to daily living, they were searching for education and resources regarding health behavior changes to assist them with self-regulation of the physical symptoms and stress.
Strengths and Limitations
The sample consisted of African American women with varying marital statuses, educational levels, and times since diagnosis. To the researchers’ knowledge, this is the first study to use a focus group methodology to better understand this population of survivors of lung cancer. This methodology revealed the factors that hinder health behavior changes in this population. Although these findings may not reflect the experiences of all lung cancer survivors, they provide a rich description of the lived experiences, efforts, challenges, frustrations, and hopes of some lung cancer survivors.
Implications for Nursing and Research
Making positive behavioral changes after a lung cancer diagnosis improves QOL and survival rates (Krebs et al., 2012). A clearer understanding of the experiences of African American women and the factors that influence their behavioral changes after a lung cancer diagnosis is essential. The current findings indicate that African American women are receptive and motivated to make health behavior changes, yet substantial challenges prevent successful change. Oncology nurses can identify challenges and help minimize the factors that hinder this change.
Survivors of lung cancer face physical and nonphysical challenges. Most importantly, the physical symptoms experienced by this population of patients—fatigue, shortness of breath, and pain— negatively affect QOL. Oncology nurses can advocate for strategies to consistently assess and palliate these common problems, as well as increase access to services that already exist, such as pulmonary rehabilitation and nutritional counseling. Incorporating strategies and interventions into a survivorship care plan may promote access and improve survivors’ QOL.
In addition, compassionate patient–provider communication is critical for understanding patients’ needs and preferences, enhancing self-care, and minimizing the effect of stigma. Culturally tailored communication should include resources for multiple behavior change and population-specific peer support groups and services.
[[{"type":"media","view_mode":"media_original","fid":"38111","attributes":{"alt":"","class":"media-image","height":"241","typeof":"foaf:Image","width":"317"}}]]
Conclusion
Future research should continue to explore vulnerable and understudied populations with lung cancer and health behavioral change. Evidence shows that multiple unhealthy behaviors tend to cluster together (Noble et al., 2015). Therefore, the development of multiple behavior change interventions is warranted. This study, and ongoing research, will move the science forward and, most importantly, positively influence the overall QOL of female African American lung cancer survivors.
The authors gratefully acknowledge DeAnne K. Hilfinger Messias, PhD, RN, FAAN, for reviewing this manuscript.
About the Author(s)
Lisa A. Webb, PhD, MSN, RN, CEN®, is a clinical instructor and PhD candidate and Karen Kane McDonnell, PhD, RN, OCN®, is an assistant professor, both in the College of Nursing at the University of South Carolina in Columbia. This research was funded by an American Cancer Society Institutional research grant from the University of South Carolina College of Pharmacy. McDonnell contributed to the conceptualization and design. Both authors completed the data collection, provided statistical support and the analysis, and contributed to the manuscript preparation. Webb can be reached at lwebb@mailbox.sc.edu, with copy to ONFEditor@ons.org. (Submitted December 2016. Accepted June 29, 2017.)
References
American Cancer Society. (2016a). Cancer facts and figures for African Americans, 2016–2018. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2016b). Cancer facts and figures, 2016. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2017). Cancer facts and figures, 2017. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Belgrave, F.Z., & Abrams, J.A. (2016). Reducing disparities and achieving equity in African American women’s health. American Psychologist, 71, 723–733. https://doi.org/10.1037/amp0000081
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101.
Brown, J.K., Cooley, M.E., Chernecky, C., & Sarna, L. (2011). A symptom cluster and sentinel symptom experienced by women with lung cancer [Online exclusive]. Oncology Nursing Forum, 38, E425–E435. https://doi.org/10.1188/11.ONF.E425-E435
Brown Johnson, C.G., Brodsky, J.L., & Cataldo, J.K. (2014). Lung cancer stigma, anxiety, depression, and quality of life. Journal of Psychosocial Oncology, 32, 59–73.
Campo, R.A., Rowland, J.H., Irwin, M.L., Nathan, P.C., Gritz, E.R., & Kinney, A.Y. (2011). Cancer prevention after cancer: Changing the paradigm—A report from the American Society of Preventive Oncology. Cancer Epidemiology, Biomarkers and Prevention, 20, 2317–2324.
Cataldo, J.K., Slaughter, R., Jahan, T.M., Pongquan, V.L., & Hwang, W.J. (2011). Measuring stigma in people with lung cancer: Psychometric testing of the Cataldo Lung Cancer Stigma Scale [Online exclusive]. Oncology Nursing Forum, 38, E46–E54. https://doi.org/10.1188/11.ONF.E46-E54
Chambers, S.K., Baade, P., Youl, P., Aitken, J., Occhipinti, S., Vinod, S., . . . O’Connell, D.L. (2015). Psychological distress and quality of life in lung cancer: The role of health-related stigma, illness appraisals and social constraints. Psycho-Oncology, 24, 1569–1577. https://doi.org/10.1002/pon.3829
Chambers, S.K., Dunn, J., Occhipinti, S., Hughes, S., Baade, P., Sinclair, S., . . . O’Connell, D.L. (2012). A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer, 12, 184. https://doi.org/10.1186/1471-2407-12-184
Chapple, A., Ziebland, S., & McPherson, A. (2004). Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ, 328, 1470. https://doi.org/10.1136/bmj.38111.639734.7C
Cooley, M.E., Finn, K.T., Wang, Q., Roper, K., Morones, S., Shi, L., . . . Hayman, L.L. (2013). Health behaviors, readiness to change, and interest in health promotion programs among smokers with lung cancer and their family members: A pilot study. Cancer Nursing, 36, 145–154. https://doi.org/10.1097/NCC.0b013e31825e4359
Cooley, M.E., Sarna, L., Kotlerman, J., Lukanich, J.M., Jaklitsch, M., Green, S.B., & Bueno, R. (2009). Smoking cessation is challenging even for patients recovering from lung cancer surgery with curative intent. Lung Cancer, 66, 218–225. https://doi.org/10.1016/j.lungcan.2009.01.021
Cooley, M.E., Wang, Q., Johnson, B.E., Catalano, P., Haddad R.I., Bueno, R., & Emmons, K.M. (2012). Factors associated with smoking abstinence among smokers and recent-quitters with lung and head and neck cancer. Lung Cancer, 76, 144–149.
Coups, E.J., Park, B.J., Feinstein, M.B., Steingart, R.M., Egleston, B.L., Wilson, D.J., & Ostroff, J.S. (2009). Correlates of physical activity among lung cancer survivors. Psycho-Oncology, 18, 395–404. https://doi.org/10.1002/pon.1520
de Moor, J.S., Mariotto, A.B., Parry, C., Alfano, C.M., Padgett, L., Kent, E.E., . . . Rowland, J.H. (2013). Cancer survivors in the United States: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiology, Biomarkers and Prevention, 22, 561–570. https://doi.org/10.1158/1055-9965.EPI-12-1356
Garces, Y.I., Yang, P., Parkinson, J., Zhao, X., Wampfler, J.A., Ebbert, J.O., & Sloan, J.A. (2004). The relationship between cigarette smoking and quality of life after lung cancer diagnosis. CHEST, 126, 1733–1741. https://doi.org/10.1378/chest.126.6.1733
Gonzalez, B.D., & Jacobsen, P.B. (2012). Depression in lung cancer patients: The role of perceived stigma. Psycho-Oncology, 21, 239–246. https://doi.org/10.1002/pon.1882
Gray, J. (2009). Rooms, recording, and responsibilities: The logistics of focus groups. Southern Online Journal of Nursing Research, 9(1). Retrieved from http://www.resourcenter.net/images/snrs/files/sojnr_articles2/Vol09Num0…
Hamann, H.A., Ostroff, J.S., Marks, E.G., Gerber, D.E., Schiller, J.H., & Lee, S.J.C. (2014). Stigma among patients with lung cancer: A patient-reported measurement model. Psycho-Oncology, 23, 81–92. https://doi.org/10.1002/pon.3371
Hawkins, N.A., Smith, T., Zhao, L., Rodriguez, J., Berkowitz, Z., & Stein, K.D. (2010). Health-related behavior change after cancer: Results of the American Cancer Society’s studies of cancer survivors (SCS). Journal of Cancer Survivorship, 4, 20–32. https://doi.org/10.1007/s11764-009-0104-3
Houlihan, N.G., & Tyson, L.B. (Eds.). (2012). Site-specific cancer series: Lung cancer (2nd ed.). Pittsburgh, PA: Oncology Nursing Society.
Kenzik, K., Pisu, M., Fouad, M.N., & Martin, M.Y. (2016). Are long-term cancer survivors and physicians discussing health promotion and healthy behaviors? Journal of Cancer Survivorship, 10, 271–279. https://doi.org/10.1007/s11764-015-0473-8
Krebs, P., Coups, E.J., Feinstein, M.B., Burkhalter, J.E., Steingart, R.M., Logue, A., . . . Ostroff, J.S. (2012). Health behaviors of early-stage non-small cell lung cancer survivors. Journal of Cancer Survivorship, 6, 37–44. https://doi.org/10.1007/s11764-011-0191-9
Marshall, C., & Rossman, G.B. (2011). Designing qualitative research (5th ed.). Thousand Oaks, CA: Sage.
McAlister, A.L., Perry, C.L., & Parcel, G.S. (2008). How individuals, environments, and health behaviors interact: Social cognitive theory. In K. Glanz, B.K. Rimer, & K. Viswanath (Eds.), Health behavior and health education: Theory, Research, and Practice (4th ed., pp. 169–188). San Francisco, CA: Jossey-Bass.
McDonnell, K.K., Bullock, L.F., Hollen, P.J., Heath, J., & Kozower, B.D. (2014). Emerging issues on the impact of smoking on health-related quality of life in patients with lung cancer and their families. Clinical Journal of Oncology Nursing, 18, 171–181. https://doi.org/10.1188/14.CJON.18-02AP
National Center for Health Statistics. (2016). National Health and Nutrition Examination Survey. Retrieved from https://www.cdc.gov/nchs/data/factsheets/factsheet_nhanes.pdf
Noble, N., Paul, C., Turon, H., & Oldmeadow, C. (2015). Which modifiable health risk behaviours are related? A systematic review of the clustering of smoking, nutrition, alcohol and physical activity (“SNAP”) health risk factors. Preventive Medicine, 81, 16–41. https://doi.org/10.1016/j.ypmed.2015.07.003
Park, E.R., Japuntich, S.J., Rigotti, N.A., Traeger, L., He, Y., Wallace, R.B., . . . Keating, N.L. (2012). A snapshot of smokers after lung and colorectal cancer diagnosis. Cancer, 118, 3153–3164. https://doi.org/10.1002/cncr.26545
Parsons, A., Daley, A., Begh, R., & Aveyard, P. (2010). Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: Systematic review of observational studies with meta-analysis. BMJ, 340, b5569. https://doi.org/10.1136/bmj.b5569
Rock, C.L., Doyle, C., Demark-Wahnefried, W., Meyerhardt, J., Courneya, K.S., Schwartz, A.L., . . . Gansler, T. (2012). Nutrition and physical activity guidelines for cancer survivors. CA: A Cancer Journal for Clinicians, 62, 242–274.
Stewart, D.W., & Shamdasani, P.N. (1990). Focus groups: Theory and practice (vol. 20). Newbury Park, CA: Sage.




