Uncertainty in Illness: Theory Review, Application, and Extension
Mishel’s uncertainty in illness theory provides a conceptual framework to explain how uncertainty is generated and how it affects psychological adjustment to the cancer experience. Since 1981, when it was created, researchers have used the theory to develop and test uncertainty management interventions in multiple populations of patients with cancer. This article reviews the theory’s concepts and propositions, summarizes supporting evidence, and discusses extension of the theory, clinical implications, and future directions for research.
Jump to a section
Uncertainty is a common psychological reaction to the experience of cancer. It is defined as “the inability to determine the meaning of illness-related events” and accurately anticipate or predict health outcomes (Mishel, 1988, p. 225). Uncertainty may be present at any point in the cancer trajectory but is common at diagnosis, initiation of new treatments, and transitions of care, when patients must cope with unfamiliar, complex, and potentially threatening experiences. Uncertainty in patients with cancer is correlated with several negative physical and psychological consequences, including symptom severity and interference in daily life, fear, emotional distress, reduced resourcefulness, a sense of losing control, and diminished quality of life (Germino et al., 2013; Hsu, Lu, Tsou, & Lin, 2003; Kazer, Bailey, Sanda, Colberg, & Kelly, 2011; Kim, Lee, & Lee, 2012; Mishel et al., 2005, 2009). Consequently, oncology nurses must be able to recognize and facilitate management of uncertainty among patients during their care. The purpose of this article is to provide an overview of Mishel’s uncertainty in illness theory, summarize current literature in patients with cancer, and discuss extension of the theory to include uncertainty in partners of patients with cancer.
Uncertainty in Illness Theory
Mishel (1981, 1988, 1990) introduced the concept of uncertainty in illness to nursing scholarship in 1981, developing her uncertainty in illness theory and designing and testing relevant instruments. Mishel’s theory builds on Lazarus and Folkman’s (1984) stress-appraisal-coping framework and focuses on describing individuals’ cognitive processes when coping with stress in the midst of ambiguous, inconsistent, or complex situations. Mishel’s uncertainty in illness theory consists of four major components: (a) antecedents generating uncertainty, (b) appraisal of uncertainty, (c) coping with uncertainty, and (d) adaptation to the illness (Mishel, 1988) (see Figure 1). 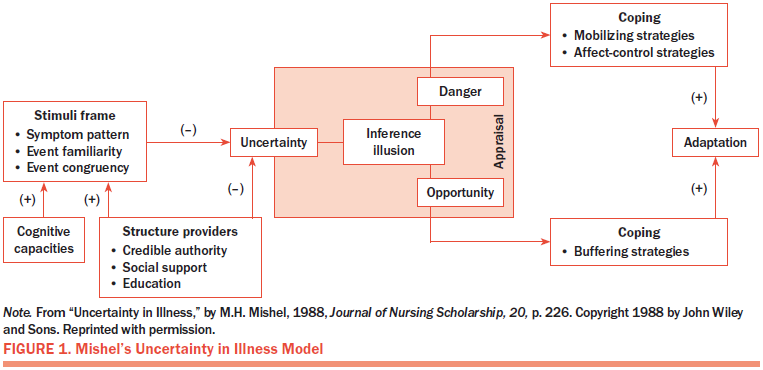
Antecedents generating uncertainty: According to Mishel (1988, 1990), antecedents of uncertainty include the stimuli frame (symptom pattern, event familiarity, event congruency), cognitive capacities, and structure providers (information from healthcare providers and other credible authorities, social support, education). New illness-related stimuli lead to uncertainty when patients are not familiar with the experience (e.g., symptoms, healthcare environment, treatment activities) or when their expectations are inconsistent with their experiences. Interpretation of the illness-related stimuli is moderated by an individual’s cognitive capacity and by structure providers. A patient’s cognitive capacity influences how he or she interprets illness-related stimuli to form a cognitive structure and indirectly affects the generation of uncertainty. Stronger cognitive capacity facilitates the patient’s understanding of stimuli, which reduces his or her uncertainty. Structure providers also influence how the patient interprets illness-related stimuli. Patients can more accurately predict and understand their experiences with appropriate education, social support, and support from healthcare providers, resulting in reduced uncertainty.
Appraisal of uncertainty: Appraisal is a cognitive process used to determine whether a stressor is a danger (threat) or opportunity (challenge) and to evaluate the availability of coping resources to respond to the stressor (Franks & Roesch, 2006; Mishel, 1981). If the stressor of uncertainty is appraised as a danger, potentially resulting in a negative outcome, then patients will attempt to use coping strategies to reduce their uncertainty. However, if uncertainty is appraised as an opportunity, potentially resulting in a positive outcome, patients will attempt to use coping strategies that maintain uncertainty (Mishel, 1981). For example, uncertainty about illness prognosis may be preferential to knowing a particularly poor prognosis among some patients. In this case, uncertainty provides the positive outcome of preserving hope (Mishel, 1988).
Coping with uncertainty: Coping is the mental and physical effort used to manage the stressor of uncertainty. Mishel’s uncertainty in illness theory postulates that different types of coping strategies are used, based on an individual’s appraisal of uncertainty. When uncertainty is appraised as a danger, patients will use mobilizing strategies to do something to eliminate the source of uncertainty (e.g., take direct action, seek information, maintain vigilance), and/or they will use affect-control strategies (e.g., faith, emotional disengagement, emotional support) to minimize the emotional distress associated with uncertainty. When uncertainty is appraised as opportunity, patients aim to use buffering strategies (e.g., avoidance, selective ignoring, neutralization of threatening information) to maintain the situation and continue the uncertainty. These buffering strategies act to block input of new stimuli, which may change an individual’s appraisal of uncertainty from an opportunity to a danger (Mishel, 1981, 1988). The theory does not suggest that one type of coping results in better outcomes than the other, but, rather, focuses on an appropriate match of effective coping strategies to an individual’s appraisal of uncertainty.
Adaptation to the illness: Adaptation is characterized as achieving new balance and adjusting to the new illness-related experience that triggered uncertainty (Mishel, 1988). If coping strategies are effective, adaptation to the illness is achieved (Mishel, 1981).
Theory Application in Patients With Cancer
Numerous studies have applied Mishel’s uncertainty in illness theory to patients with cancer, such as adults with lung, prostate, gynecologic, and breast cancers across all stages of disease and throughout the illness trajectory (Kurita, Garon, Stanton, & Meyerowitz, 2013; Liao, Chen, Chen, & Chen, 2008; Mishel & Braden, 1987, 1988; Mishel & Sorenson, 1991). Researchers have demonstrated that illness-related events trigger uncertainty in patients with cancer (Mast, 1998; Mishel, 1988; Shaha, Cox, Talman, & Kelly, 2008; Wong & Bramwell, 1992). Patients who were receiving active cancer treatment and patients with increased physical symptoms reported higher levels of uncertainty than those who were receiving surveillance and those who had fewer physical symptoms (Kim et al., 2012; Wong & Bramwell, 1992). In a systematic review of the literature, Shaha et al. (2008) identified multiple causes of uncertainty, including a lack of medical information, incomplete understanding of treatment choices or the typical course of disease, and difficulty coping with the precariousness of daily life. High levels of uncertainty were found in patients with poor cognitive ability, low levels of education, and limited social support (Liao et al., 2008; Lien, Lin, Kuo, & Chen, 2009; Mast, 1998).
Based on Mishel’s theory, researchers developed uncertainty management interventions that featured four components to target the antecedents and appraisal of uncertainty, along with coping strategies. The first two components (information provision and communication strategies) target the antecedent variables of stimuli frame and structure providers. Stimuli frame was addressed by providing information regarding treatment, symptoms, and support resources to improve cancer knowledge. Structure providers were addressed through instruction in communication strategies to promote patient–provider communication (Mishel et al., 2009). The third component targeted appraisal by encouraging reframing of uncertainty in a positive light and incorporating uncertainty into patients’ daily lives (Kazer et al., 2011; Mishel et al., 2005). The fourth component targeted coping by providing training in cognitive behavioral coping strategies, such as relaxation, pleasant imagery, calming self-talk, distraction, self-monitoring, and self-care management (Germino et al, 2013; Gil et al., 2006; Kazer et al., 2011; Mishel et al., 2005). Overall, previous studies demonstrated improvements in process variables (cancer knowledge, positive thinking, problem solving, patient–provider communication, access to information resources, use of coping strategies, social support), reduced uncertainty, and improved quality of life (Bailey, Mishel, Belyea, Stewart, & Mohler, 2004; Germino et al., 2013; Gil et al., 2006; Kazer et al., 2011; Liu, Li, Tang, Huang, & Chiou, 2006; Mishel et al., 2005, 2009).
The Patient–Partner Dyad Experiencing Uncertainty
As the clinical practice paradigm shifts from patient- to family-centered care, more research is beginning to focus on the dyad consisting of the patient with cancer and his or her partner (Berg & Upchurch, 2007; Northouse et al., 2007; Rottmann et al., 2015; Traa, De Vries, Bodenmann, & Den Oudsten, 2015). Although Mishel’s uncertainty in illness theory addresses patients’ experiences of uncertainty, the reality is that both patients and their partners experience uncertainty pertaining to the cancer diagnosis, treatment, and prognosis. Partners act as a major source of social support, often providing daily and tangible assistance that may reduce patients’ uncertainty (Mishel, 1988). For example, partners may take on the caregiving role (Hilton, Crawford, & Tarko, 2000), providing transportation between the home and treatment appointments, coordinating with clinicians, and helping with medication and side effect management. In addition, partners may need to fulfill more family responsibilities that had previously been carried out by patients, such as child care and housework (Hilton et al., 2000). Using uncertainty measures for patients and their family members that were developed by Mishel, investigators have demonstrated that partners report slightly more uncertainty and less support than patients with cancer, which may be attributable to a lack of information about the patient’s illness or to their concerns or questions that are directly addressed by healthcare professionals (Northouse, Laten, & Reddy, 1995; Senatore, 2013).
Patients and their partners need to cope with illness-related uncertainty. Dyadic coping is a common endeavor to manage stress faced by the patient–partner dyad and involves strategies such as stress communication, supportive exchanges between patients and their partners, joint problem solving, and emotion-focused coping (Rottmann et al., 2015; Traa et al., 2015). Research has shown that, as couples’ dyadic communication increased, their uncertainty decreased and their quality of life was improved (Song et al., 2011, 2012).
The diagnosis of cancer and its treatment can change dynamics between patients and their partners, which may negatively affect dyadic coping. Although couples share a similar experience of living with the diagnosis of cancer, they may employ different coping strategies and appraise stressors differently. Koop (1994) reported that patients tended to be more likely to appraise cancer as an opportunity and reported more distancing, accepting of responsibility, and seeking of social support than did their partners.
Attention to the concept of uncertainty may facilitate coping in patient–partner dyads facing cancer. For example, Northouse, Kershaw, Mood, and Schafenacker (2005) and Northouse et al. (2007, 2013) developed a cancer coping intervention program for patients and their caregivers (mostly partners) that included an uncertainty management component. In addition to offering standardized information and strategies to support family involvement in coping, the intervention provided family training in uncertainty management via obtaining information, increasing assertiveness, and learning to live with uncertainty (Northouse et al., 2005). Investigators observed some improvement in patients’ and partners’ uncertainty (Northouse et al., 2007). These findings suggest that a dyad-focused uncertainty management intervention, guided by Mishel’s uncertainty in illness theory, may be useful in research and practice.
Conclusion
Mishel’s uncertainty in illness theory provides a framework for clinicians to understand the generation and control of uncertainty among individuals facing cancer. The theory can assist oncology nurses in anticipating uncertainty in practice situations, such as unexplained symptom change, a pending biopsy result, limited social support, and other contexts in which patients and families have insufficient information. Oncology nurses can evaluate sources of uncertainty and identify relevant coping strategies to manage uncertainty, as well as play an important role in providing education, helping patients and their families to understand the cancer experience, and addressing their questions.
For cancer survivors and their partners, living with uncertainty is a long-term challenge. Nurse researchers must answer the need for uncertainty management interventions that facilitate dyadic coping and adjustment throughout the cancer trajectory. Continued research in this area will equip clinicians with evidence-based interventions to assist patient–partner dyads confronting uncertainty in illness.
The author gratefully acknowledges Kristine Kwekkeboom, PhD, RN, FAAN, and Marie Flannery, PhD, RN, AOCN®, for their helpful comments on earlier versions of this article.
About the Author(s)
Zhang is a distinguished graduate fellow and doctoral student in the School of Nursing at the University of Wisconsin in Madison. No financial relationships to disclose. Zhang can be reached at yzhang456@wisc.edu, with copy to editor at ONFEditor@ons.org.
References
Bailey, D.E., Mishel, M.H., Belyea, M., Stewart, J.L., & Mohler, J. (2004). Uncertainty intervention for watchful waiting in prostate cancer. Cancer Nursing, 27, 339–346.
Berg, C.A., & Upchurch, R. (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133, 920–954. https://doi.org/10.1037/0033-2909.133.6.920
Franks, H.M., & Roesch, S.C. (2006). Appraisals and coping in people living with cancer: A meta-analysis. Psycho-Oncology, 15, 1027–1037. https://doi.org/10.1002/pon.1043
Germino, B.B., Mishel, M.H., Crandell, J., Porter, L., Blyler, D., Jenerette, C., & Gil, K.M. (2013). Outcomes of an uncertainty management intervention in younger African American and Caucasian breast cancer survivors. Oncology Nursing Forum, 40, 82–92. https://doi.org/10.1188/13.ONF.82-92
Gil, K.M., Mishel, M.H., Belyea, M., Germino, B., Porter, L.S., & Clayton, M. (2006). Benefits of the uncertainty management intervention for African American and white older breast cancer survivors: 20-month outcomes. International Journal of Behavioral Medicine, 13, 286–294. https://doi.org/10.1207/s15327558ijbm1304_3
Hilton, B.A., Crawford, J.A., & Tarko, M.A. (2000). Men’s perspectives on individual and family coping with their wives’ breast cancer and chemotherapy. Western Journal of Nursing Research, 22, 438–459. https://doi.org/10.1177/019394590002200405
Hsu, T.-H., Lu, M.-S., Tsou, T.-S., & Lin, C.-C. (2003). The relationship of pain, uncertainty, and hope in Taiwanese lung cancer patients. Journal of Pain and Symptom Management, 26, 835–842. https://doi.org/10.1016/S0885-3924(03)00257-4
Kazer, M.W., Bailey, D.E., Jr., Sanda, M., Colberg, J., & Kelly, W.K. (2011). An internet intervention for management of uncertainty during active surveillance for prostate cancer. Oncology Nursing Forum, 38, 561–568. https://doi.org/10.1188/11.ONF.561-568
Kim, S.H., Lee, R., & Lee, K.S. (2012). Symptoms and uncertainty in breast cancer survivors in Korea: Differences by treatment trajectory. Journal of Clinical Nursing, 21, 1014–1023. https://doi.org/10.1111/j.1365-2702.2011.03896.x
Koop, P.M. (1994). Stress, appraisal and coping with cancer [Doctoral dissertation]. Retrieved from ProQuest Dissertations and Theses database. (UMI No. 275929600)
Kurita, K., Garon, E.B., Stanton, A.L., & Meyerowitz, B.E. (2013). Uncertainty and psychological adjustment in patients with lung cancer. Psycho-Oncology, 22, 1396–1401. https://doi.org/10.1002/pon.3155
Lazarus, R.S., & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer.
Liao, M.-N., Chen, M.-F., Chen, S.-C., & Chen, P.-L. (2008). Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nursing, 31, 274–283. https://doi.org/10.1097/01.NCC.0000305744.64452.fe
Lien, C.-Y., Lin, H.-R., Kuo, I.-T., & Chen, M.-L. (2009). Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. Journal of Clinical Nursing, 18, 2311–2319. https://doi.org/10.1111/j.1365-2702.2008.02549.x
Liu, L.N., Li, C.Y., Tang, S.T., Huang, C.S., & Chiou, A.F. (2006). Role of continuing supportive cares in increasing social support and reducing perceived uncertainty among women with newly diagnosed breast cancer in Taiwan. Cancer Nursing, 29, 273–282.
Mast, M.E. (1998). Survivors of breast cancer: Illness uncertainty, positive reappraisal, and emotional distress. Oncology Nursing Forum, 25, 555–562.
Mishel, M.H. (1981). The measurement of uncertainty in illness. Nursing Research, 30, 258–263.
Mishel, M.H. (1988). Uncertainty in illness. Journal of Nursing Scholarship, 20, 225–232. https://doi.org/10.1111/j.1547-5069.1988.tb00082.x
Mishel, M.H. (1990). Reconceptualization of the uncertainty in illness theory. Journal of Nursing Scholarship, 22, 256–262. https://doi.org/10.1111/j.1547-5069.1990.tb00225.x
Mishel, M.H., & Braden, C.J. (1987). Uncertainty. A mediator between support and adjustment. Western Journal of Nursing Research, 9, 43–57.
Mishel, M.H., & Braden, C.J. (1988). Finding meaning: Antecedents of uncertainty in illness. Nursing Research, 37, 98–103.
Mishel, M.H., Germino, B.B., Gil, K.M., Belyea, M., LaNey, I.C., Stewart, J., . . . Clayton, M. (2005). Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psycho-Oncology, 14, 962–978. https://doi.org/10.1002/pon.909
Mishel, M.H., Germino, B.B., Lin, L., Pruthi, R.S., Wallen, E.M., Crandell, J., & Blyler, D. (2009). Managing uncertainty about treatment decision making in early stage prostate cancer: A randomized clinical trial. Patient Education and Counseling, 77, 349–359. https://doi.org/10.1016/j.pec.2009.09.009
Mishel, M.H., & Sorenson, D.S. (1991). Uncertainty in gynecological cancer: A test of the mediating functions of mastery and coping. Nursing Research, 40, 167–171.
Northouse, L., Kershaw, T., Mood, D., & Schafenacker, A. (2005). Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psycho-Oncology, 14, 478–491. https://doi.org/10.1002/pon.871
Northouse, L.L., Laten, D., & Reddy, P. (1995). Adjustment of women and their husbands to recurrent breast cancer. Research in Nursing and Health, 18, 515–524.
Northouse, L.L., Mood, D.W., Schafenacker, A., Kalemkerian, G., Zalupski, M., LoRusso, P., . . . Kershaw, T. (2013). Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncology, 22, 555–563. https://doi.org/10.1002/pon.3036
Northouse, L.L., Mood, D.W., Schafenacker, A., Montie, J.E., Sandler, H.M., Forman, J.D., . . . Kershaw, T. (2007). Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer, 110, 2809–2818. https://doi.org/10.1002/cncr.23114
Rottmann, N., Hansen, D.G., Larsen, P.V., Nicolaisen, A., Flyger, H., Johansen, C., & Hagedoorn, M. (2015). Dyadic coping within couples dealing with breast cancer: A longitudinal, population-based study. Health Psychology, 34, 486–495. https://doi.org/10.1037/hea0000218
Senatore, N. (2013). The effects of uncertainty for couples in cancer survivorship [Doctoral dissertation]. Retrieved from ProQuest Dissertation and Theses database. (UMI No. 3612497)
Shaha, M., Cox, C.L., Talman, K., & Kelly, D. (2008). Uncertainty in breast, prostate, and colorectal cancer: Implications for supportive care. Journal of Nursing Scholarship, 40, 60–67. https://doi.org/10.1111/j.1547-5069.2007.00207.x
Song, L., Northouse, L.L., Braun, T.M., Zhang, L., Cimprich, B., Ronis, D.L., & Mood, D.W. (2011). Assessing longitudinal quality of life in prostate cancer patients and their spouses: A multilevel modeling approach. Quality of Life Research, 20, 371–381. https://doi.org/10.1007/s11136-010-9753-y
Song, L., Northouse, L.L., Zhang, L., Braun, T.M., Cimprich, B., Ronis, D.L., & Mood, D.W. (2012). Study of dyadic communication in couples managing prostate cancer: A longitudinal perspective. Psycho-Oncology, 21, 72–81. https://doi.org/10.1002/pon.1861
Traa, M.J., De Vries, J., Bodenmann, G., & Den Oudsten, B.L. (2015). Dyadic coping and relationship functioning in couples coping with cancer: A systematic review. British Journal of Health Psychology, 20, 85–114. https://doi.org/10.1111/bjhp.12094
Wong, C.A., & Bramwell, L. (1992). Uncertainty and anxiety after mastectomy for breast cancer. Cancer Nursing, 15, 363–371.

