Feasibility Study of an Online Intervention to Support Male Spouses of Women With Breast Cancer
Purpose/Objectives: To evaluate the feasibility of a web-based psychosocial supportive intervention entitled Male Transition Toolkit (MaTT).
Design: Randomized, controlled trial, mixed methods, concurrent feasibility design.
Setting: Edmonton, a large metropolitan city in western Canada.
Sample: 40 dyads (women with breast cancer and their spouse).
Methods: Male spouse participants in the treatment group accessed MaTT for four weeks. Data on hope, quality of life, general self-efficacy, and caregiver guilt were collected at baseline and days 14, 28, and 56. Quality-of-life data were collected from the women with breast cancer at each time period. Qualitative data were collected from the usual care group in an open-ended interview and from the treatment group in an evaluation survey on days 14 and 28.
Main Research Variables: Feasibility, as measured by the MaTT questionnaire.
Findings: Evaluation survey scores indicated that MaTT was feasible, acceptable, and easy to use. Male spouse quality-of-life scores were not significantly different between groups. As guilt scores decreased, male spouses’ quality of life increased.
Conclusions: The findings provided useful information to strengthen MaTT and improve study design. Additional research is needed to determine its efficacy in improving male spouses’ quality of life.
Implications for Nursing: MaTT is a feasible intervention. Future research should evaluate MaTT with larger samples as well as determine the amount of time participants used MaTT.
Jump to a section
Male spouses of women with breast cancer undergo sudden changes as a result of their partner’s diagnosis (Duggleby, Bally, Cooper, Doell, & Thomas, 2012; Duggleby et al., 2015; Struthers-Montford et al., 2016), including changes in their roles, responsibilities, relationship to their partner, and mental health (Duggleby et al., 2015). They also can feel powerless, uncertain, and isolated (Duggleby, Bally, et al., 2012; Duggleby et al., 2015; Zahlis & Lewis, 2010). Male spouses require strategies and interventions that help them engage in hope, communicate with their partners, find support, and access information about breast cancer (Duggleby, Bally, et al., 2012; Duggleby et al., 2015). However, few resources and interventions are available to help them during this time of significant changes (Duggleby, Bally, et al., 2012; Duggleby et al., 2015).
Cochrane and Lewis’s (2005) systematic review of intervention studies for male spouses of women with breast cancer reported four studies published from 1966 to 2004. They found a consensus within the literature that interventions for male spouses are needed, with research in this area lagging “far behind descriptive work” (p. 331). The four interventions discussed by Cochrane and Lewis (2005) were group therapy, individual or couple’s therapy, couples’ counseling, and a men’s discussion group. None of the interventions were self-administered.
Since Cochrane and Lewis’s (2005) review, three research studies focusing on interventions for male spouses of women with breast cancer have been published. All three focused on the Helping Her Heal (HHH) program, with two of the studies (published in one article) describing an individual counseling intervention (Lewis et al., 2008) and one describing a group intervention for male spouses (Jones et al., 2013). The studies with individual counseling suggest the HHH program has the potential to (a) help spouses adjust to their wives’ illness, (b) improve their skills in caring for their spouse, (c) increase their feelings of self-efficacy, and (d) partake in their own self-care (Lewis et al., 2008). The group intervention (HHH-G) was reported to improve men’s ability to (a) care for their spouses, (b) increase their self-efficacy, and (c) increase their ability to employ self-care during their wives’ illness (Jones et al., 2013).
Although these interventions make an important contribution to the quality of life (QOL) of male spouses of women with breast cancer, they require face-to-face meetings with trained experts (e.g., counselors, psychologists) and a predetermined session limit. In contrast, web-based interventions can be self-administered and may be more acceptable by enabling caregivers of patients with cancer to access the tool when it is convenient (Kaltenbaugh et al., 2015). Web-based interventions have been found to have a positive influence on caregivers’ social and psychological outcomes (Kaltenbaugh et al., 2015). A systematic review of web-based interventions for caregivers of patients with cancer (Kaltenbaugh et al., 2015) described (a) one intervention for caregivers of patients with cancers involving the blood (Farnham et al., 2002), (b) two tailored for caregivers of patients with lung cancer (DuBenske, Gustafson, Shaw, & Cleary, 2010; Namkoong et al., 2012), and (c) three for caregivers of patients with a variety of cancers, including breast cancer (Chih et al., 2013; Scott & Beatty, 2013; Zulman et al., 2012). The authors concluded that caregivers benefited from web-based interventions; however, none of these web-based interventions were specifically tailored for male spouses of women with breast cancer. Therefore, a web-based psychosocial supportive intervention focused on supporting male spouses of women with breast cancer may benefit this population.
Intervention Framework
The intervention framework (see Figure 1) for the study was based on transition theory (Meilis, 2010), a study of factors influencing male spouse QOL (Duggleby et al., 2015), and a qualitative study of transitions (Struthers-Montford et al., 2016). Transition theory suggests that significant changes result in disruptions in the lives of the male spouses of women with breast cancer. To adapt to these changes, male spouses go through three processes: (a) becoming aware of the changes in their situation, (b) fostering a positive approach, and (c) becoming involved with the care of their spouse with breast cancer (Struthers-Montford et al., 2016). These three processes were the foundation for the intervention components. A self-administered online intervention tailored to support male spouses of women with breast cancer, the Male Transition Toolkit (MaTT), was developed based on the intervention framework and using a four-phase delphi approach with an expert panel.
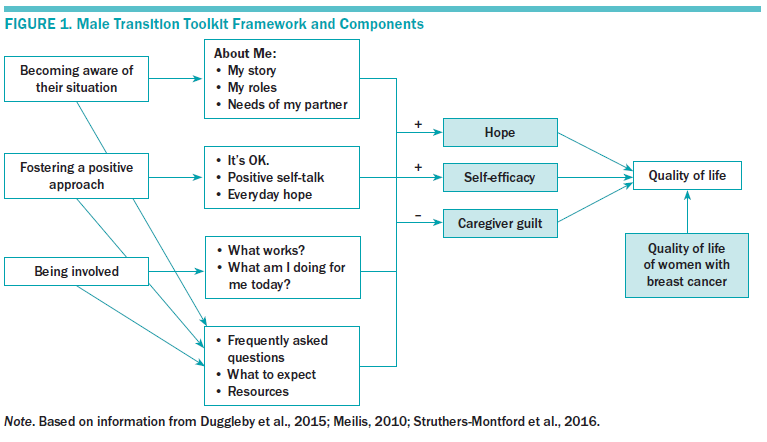
Hope, general self-efficacy, caregiver guilt, and the QOL of women with breast cancer have been noted as significant variables influencing the QOL of male spouses (Duggleby, Bally, et al., 2012; Duggleby et al., 2015). In addition, as the hope of male spouses and their general self-efficacy increased, feelings of guilt decreased and their QOL increased. In addition, the QOL of the women with breast cancer was significantly and positively related to that of their male partners. Hope, general self-efficacy, and perceptions of guilt were hypothesized as potential mechanisms through which male spouses’ QOL would increase. The QOL of women with breast cancer is hypothesized to be a moderating variable for male spouse QOL.
Purpose
The purpose of this study was to evaluate the feasibility of MaTT. The specific aims were to evaluate MaTT for ease of use, acceptability, and feasibility, and to collect preliminary data to determine the potential efficacy of MaTT with respect to increasing the QOL of male partners of women with stages I–III breast cancer compared to a usual care group.
Methods
A randomized, controlled trial, mixed methods, concurrent feasibility study was used (Creswell & Plano Clark, 2011). Participants were randomly assigned to a treatment or usual care group. Those in the treatment group were able to access MaTT during a four-week timeframe. Quantitative and qualitative data were collected concurrently and integrated in the results phase of the study. Baseline and post measures (days 14, 28, and 56) of quantitative data (hope, QOL, general self-efficacy, and caregiver guilt) were collected from the treatment and usual care groups. QOL data from the male participants’ spouses (women with breast cancer) were collected in both groups. At days 14 and 28, a MaTT evaluation survey (which included quantitative and qualitative data) was completed by those in the treatment group. Qualitative data collected through the usual care control group open-ended interviews provided an understanding of the experience of usual care in this group.
The University of Alberta Health Research Ethics Board–Cancer Care committee approved this study. Operational approval was granted by Covenant Health Research Center and the Cross Cancer Institute. Informed consent was obtained for all study participants, and confidentiality was maintained by removing all identifying information and assigning study ID numbers.
Male Transition Toolkit
The web-based intervention (MaTT) consisted of six sections (a) about me, (b) common changes to expect, (c) frequently asked questions, (d) resources, (e) calendar, and (f) important health information (see Figure 2). The about me section was iterative, and participants could add information and upload pictures, for example.
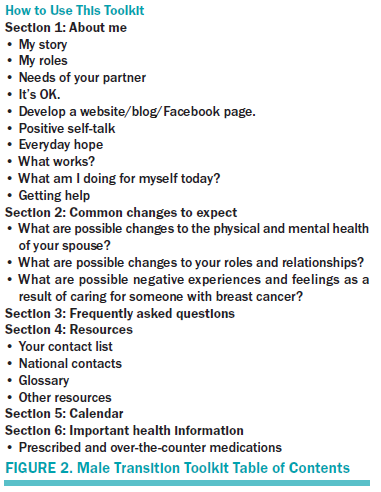
Participants in the treatment group were instructed on how to access MaTT and use it during a four-week time period. This time period was based on the research team’s previous evaluation of the feasibility of an online toolkit for people who were deemed palliative and their family caregivers (Duggleby, Cooper, et al., 2012). Participants in the treatment group were also instructed to use whatever part of MaTT they wished. At the conclusion of the study (day 56), the usual care group was given access to MaTT.
Main Research Variables
Demographic form: Male spouse participant information such as age, number of years married, occupation, ethnicity, income, religious affiliation, any medical conditions, and education levels was collected. Information about their partners (women with breast cancer), such as age and diagnosis, was also collected.
Functional Assessment of Cancer–Breast: QOL of the women with breast cancer was measured using the Functional Assessment of Cancer–Breast (FACT-B) questionnaire (Brady et al., 1997). The FACT-B is a 44-item, five-point scale (0 “not at all” to 4 “very much”) consisting of four well-being subscales (physical, social, emotional, and functional), as well as a fifth subscale on breast cancer–related concerns. The total score is a sum of five subscale scores with a maximum score of 148. A higher score indicates higher QOL. An internal consistency of r = 0.93 was reported in a study of male spouses of women with breast cancer (Duggleby, Doell, Cooper, Thomas, & Ghosh, 2014).
Herth Hope Index: The Herth Hope Index (HHI) is a 12-item, four-point Likert-type scale that delineates three factors of hope: (a) temporality and future, (b) positive readiness and expectancy, and (c) interconnectedness (Herth, 1992). A higher score denotes higher hope, with a maximum score of 48. The HHI takes about five minutes to complete and has been demonstrated to have good reliabilty (test-retest r = 0.91, p < 0.05) and validity (concurrent validity, r = 0.84, p < 0.05; criterion, r = 0.092, p < 0.05; divergent, r = –0.73, p < 0.05) in patients with cancer (Herth, 1992). It has been used successfully in studies with family caregivers (Borneman, Stahl, Ferrell, & Smith, 2002; Duggleby et al., 2007).
General Self-Efficacy Scale: The General Self-Efficacy Scale (GSES) is a 10-item, four-point Likert-type scale that produces a total perceived self-efficacy score (Luszcynska, Mohamed, & Schwarzer, 2005). Higher scores on the GSES indicate a higher self-efficacy or the personal confidence to deal with adverse situations. The GSES has a maximum score of 40 and was chosen as a measure for this study because it has good reliability and validity evidence (internal consistency alpha = 0.91, test-retest reliability r = 0.82) in many populations and countries (Luszcynska, Gutiérrez-Doña, & Schwarzer, 2005). It has also been used in studies with male spouses of women with breast cancer (Duggleby et al., 2014, 2015).
Caregiver Guilt Questionnaire: The Caregiver Guilt Questionnaire (CGQ) was used to measure perceptions of guilt using a 22-item, five-point scale with a maximum total score of 88 (Losada, Márquez-González, Peñacoba, & Romero-Moreno, 2010). It has been used in a study of male spouses of women with breast cancer with reported internal consistency of r = 0.93 (Duggleby et al., 2015).
Caregiver Quality of Life Index–Cancer: The Caregiver Quality of Life Index–Cancer (CQOL-C) scale was developed specifically for family caregivers of patients with cancer (Weitzner, Jacobson, Wagner, Friedland, & Cox, 1999). It consists of 35 items using a five-point Likert-type scale with a maximum score of 130. It has four subscales: burden (physical and emotional), disruptiveness, positive adaptation, and financial concerns. Higher scores reflect higher QOL. Reported test-retest reliability is r = 0.95 and an internal consistency of r = 0.91 (Weitzner et al., 1999). It was appropriate for this study because it is easy to use and was developed based on QOL studies of caregivers of patients with cancer.
Male Transition Tookit evaluation questionnaire: The MaTT evaluation questionnaire was previously used in the evaluation of a similar intervention (Changes Toolkit) (Duggleby, Cooper, et al., 2012) to assess ease of use, acceptability, and feasibility based on the program evaluation frameworks of McKenzie and Smelzer (1997) and Timmreck (1995). The first part of the evaluation asked participants to indicate if they used specific sections of the MaTT (yes or no). The second part featured nine questions focusing on ease of use, acceptability, feasibility, and effectiveness using, with 0 indicating no agreement and 5 indicating strong agreement. The qualitative questions asked were:
• What worked well with MaTT?
• What would you suggest to improve MaTT?
• Any other comments?
Usual care interview guide: Participants in the usual care group were asked the following open-ended questions:
• Can you describe your typical day now that your partner has breast cancer?
• What are some changes to your life as a result of the diagnosis?
• Is there anything you have found that helps you deal with these changes?
v What services and resources have you accessed because of your partner’s diagnosis?
• Is there anything else you would like to add?
Sample and Setting
The setting for the study was Edmonton, a large metropolitan city and its surrounding area in Western Canada. A sample size of 40 (20 per group) was the target, based on Birkett and Day’s (1994) recommendations for sample sizes in feasibility studies.
Participant dyads were recruited using a variety of strategies, such as (a) nurses at the Cross Cancer Institute outpatient clinics, (b) the breast cancer nurse navigator at the Misercordia Community Hospital, (c) posters at pharmacies and medical supply stores, and (d) social media postings from the Canadian Breast Cancer Foundation. Nurses approached potential participants who met the inclusion criteria and asked if they would be willing to speak with a research assistant (RA) about the study. The posters guided potential participants to call a toll-free 800 number or email if they were interested. Inclusion criteria for male participants were aged 18 years and older, English speaking, and currently living with and who have a legal relationship with a women with breast cancer (stages I–III). A legal relationship is defined as married or as cohabiting for a minimum of one year. Inclusion criteria for their partners with breast cancer were being female, aged 18 years and older, English speaking, and diagnosed with breast cancer (stages I–III). If either partner declined to participate, the dyad was deemed ineligible.
Data Collection Procedure
The data collection procedure is presented in Figure 3. If potential participants agreed to be contacted or contacted the principal investigator (PI), a trained RA contacted them by telephone, explained the study, and obtained verbal informed consent.
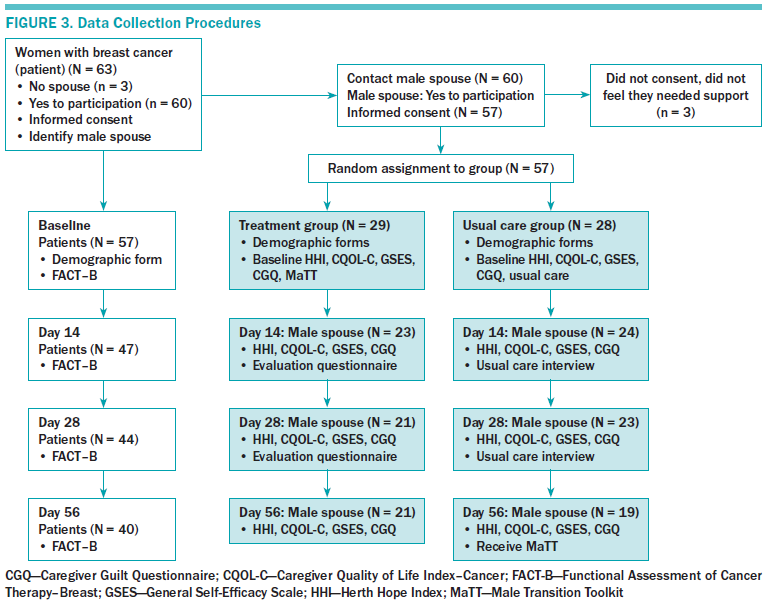
Data collection at each time point ranged from 30–90 minutes in duration for each participant. At intake, the RA collected demographic information and baseline measures (HHI, GSES, CGQ, and CQOL-C) from the male spouse participants. Female participants were asked to complete a demographic form and the FACT-B. Male spouse participants were then randomly assigned to either a treatment or usual care group. At days 14 and 28, the male participants in the treatment group were asked to complete the MaTT evaluation questionnaire and the usual care group participants were interviewed using the usual care interview guide. At days 14, 28, and 56, male spouse participants in both groups completed the HHI, GSES, CGQ, and CQOL-C questionnaires. Female participants in both groups were asked to complete the FACT-B at days 14, 28, and 56.
All data were collected over the phone, and the calls were audio recorded. Verification was completed by a random check of the audio recordings. Quantitative data were entered into forms on a protected laptop and then downloaded onto a secure shared drive. Qualitative interview audio files were downloaded onto a secure shared drive and were transcribed by an experienced transcriptionist. All files were anonymized.
Data Analysis
Quantitative data were entered by a trained RA into SPSS®, version 18, and checked for accuracy by a different RA. Descriptive statistics were used to summarize data and analyze responses to MaTT quantitative evaluation questions. The association between continuous demographic variables and dichotomous outcome variables was detected using an independent t test. Chi-square tests were used to compare categorical variables. Generalized estimating equations (GEEs) were used to determine differences in CQOL-C scores between the groups over time. GEE has several advantages: it effectively increases the sample size (increasing power) and estimates robust standard errors by taking into account the repeated measures and adjusting for covariates (Ghisletta & Spini, 2004). The covariates for this study were based on the intervention framework (HHI, GSES, CGQ, and FACT-B). GEE can be used with non-normally distributed data and with small sample sizes of 20 (Ballinger, 2004). In addition, as the data were missing at random, all participants were retained in the analysis without imputation of missing data (Liu, Dixon, Qui, Tian, & McCorkle, 2009).
The qualitative data from the MaTT evaluation questionnaire and the usual care control group interviews were transcribed, cleaned, checked, and then analyzed using Krippendorff’s (2012) content analysis. Categories were developed and then collapsed into themes representing patterns in the data. Trustworthiness of the data was maintained using the words of the participants as much as possible and by keeping an audit trail of decisions. The qualitative findings from the evaluation survey were integrated with quantitative data during the results phase. The qualitative findings from the usual care interview guide were reported separately to provide an understanding of what constitutes usual care for male spouses of women with breast cancer.
Results
Participants
Fifty-seven dyads (women with breast cancer and their spouses) participated in this feasibility study with 29 male spouses in the MaTT treatment group and 28 in the usual care group. Forty participant dyads (30% attrition) completed all data collection. At day 56, the attrition rate was higher in the usual care group (9 of 28, 31%) than in the treatment group (8 of 29, 28%). Participant dyads withdrew themselves from the study for a variety of reasons, including (a) the breast cancer’s diagnosis changed to stage IV (n = 7), (b) the partner with breast cancer was diagnosed with a second cancer (n = 1), and (c) for unknown reasons/did not respond to contact attempts (n = 9).
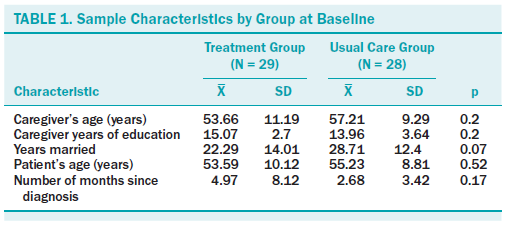
The mean age of male spouses was 55.4 years (SD = 10.37). They had an average of 14.53 (SD = 3.21) years of education and had been married an average of 25.45 years (SD = 13.52). The mean age of the women with breast cancer was 54.39 years (SD = 9.45) with a mean length of time since initial diagnoses, with breast cancer and study entry of 3.84 months (SD = 6.32). The majority of male spouse participants were Caucasian (n = 51), with a small contingent identifying as First Nations (n = 2), Middle Eastern (n = 1), Asian (n = 1), and Chilean (n = 1). Most women with breast cancer (n = 38) were undergoing treatment when they began participating in the study. The treatment and usual care groups were not significantly different in regard to demographic variables (see Table 1).
Ease of Use, Feasibility, Acceptability, and Efficacy
The findings from the MaTT evaluation survey are presented in Table 2, which reports the numbers of participants and their response to the evaluation.
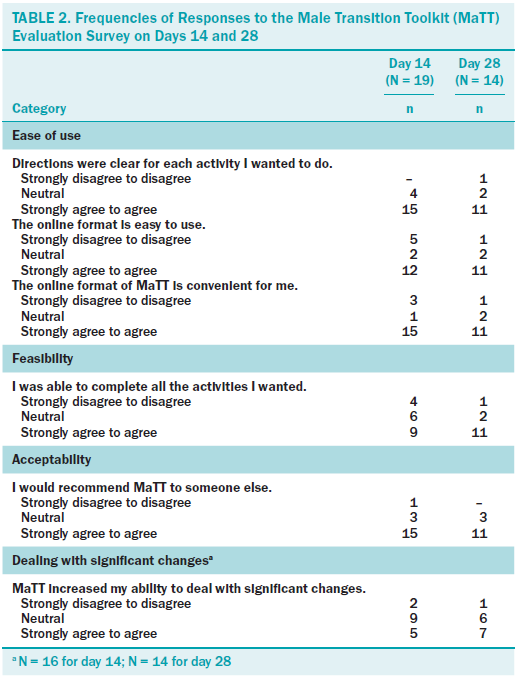
Ease of use: Most participants in the treatment group who completed the evaluation at days 14 (79%) and 28 (85%) reported that they agreed and/or strongly agreed with the statement that directions were clear. The majority also agreed or strongly agreed that the online format was easy to use (day 14, 63%; day 28, 79%). By day 28, most participants agreed (85%) that they were “sure about what to do with each activity.” This was supported by the qualitative data. For example, one participant noted that MaTT was “laid out clearly and chronologically.” Another participant said, “easy to use and navigate through the site.”
However, other participants found the online format difficult to use and would have preferred a hard copy. As one participant suggested, “Some people, depending on age and circumstance or keyboard skills, wouldn’t be great, so maybe paper-based would be more appropriate.”
Feasibility: Most participants in the treatment group agreed or strongly agreed that the online format was convenient (day 14, 79%; day 28, 85%) and they had enough time and energy to complete the activities they wanted (day 14, 56%; day 28, 85%). Fifty percent of participants agreed or strongly agreed that they were able to complete the activities they wanted at day 14; this value increased to 85% at day 28.
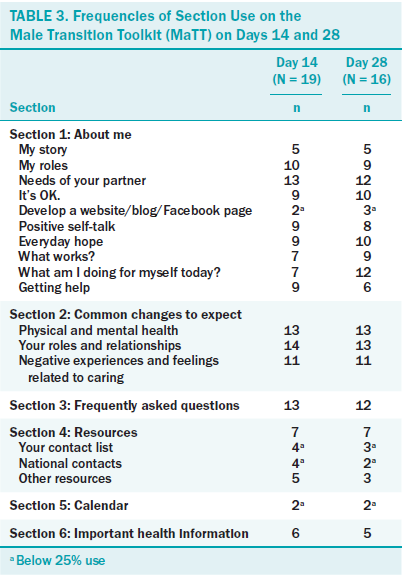
Acceptability: The majority of participants on day 14 (79%) and on day 28 (79%) agreed they would recommend MaTT to another person. The participants did use different parts of MaTT (see Table 3). The most frequently used sections on days 14 and 28 were the activities entitled “my roles” (56% both days) and “needs of my partner” (68% and 75%, respectively). The sections used by fewer than 25% of the participants were “developing a website/blog,” “contact lists,” and the “calendar.” Participants suggested the following changes to MaTT: (a) expand the “needs of your partner section,” (b) remove the “calendar,” (c) remove the “how to create a website/blog/Facebook” section, and (d) remove the “important health information” section.
Efficacy: Sixty-one percent of participants on day 14 and 46% on day 28 were neutral in regard to whether MaTT helped them deal with significant changes. However, the percentage of participants who agreed and strongly agreed that MaTT helped them deal with significant changes increased from 28% on day 14 to 46% on day 28. The qualitative data suggested that the activities in MaTT helped some participants cope with transitions. For example, a participant relayed that the positive self-talk exercise in MaTT was beneficial. “Positive self-talk . . . I think sometimes when we get overwhelmed, we’ve got to step back and say, ‘OK,’ you know, ‘let’s just do one step at a time.’ I think that’s a good lesson for everybody, not just people, you know, who are dealing with cancer.” Participants also found MaTT helpful in providing information. A participant said, “MATT has now become my best tool for resources and help.”
Potential Efficacy of Male Transition Toolkit Compared to the Usual Care Group
Mean scores for the main variables are presented in Table 4. No significant differences were noted between the groups for CQOL-C scores (p = 0.22). Effect sizes were calculated for the primary outcome variable, CQOL-C using Cohen’s d statistical analysis for days 14 (d = 0.09), 28 (d = 0.39), and 56 (d = 0.19). Based on the effect size from day 28 (immediately post-treatment) of 0.39 (moderate effect size), alpha of 0.05, and a power of 0.8, and Munro’s (2005) tables for power analysis, an adequate sample size would be 45 per group with a total of 90 participants.
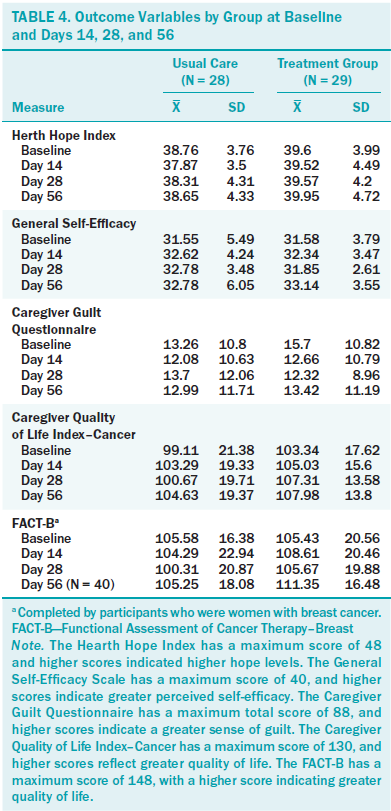
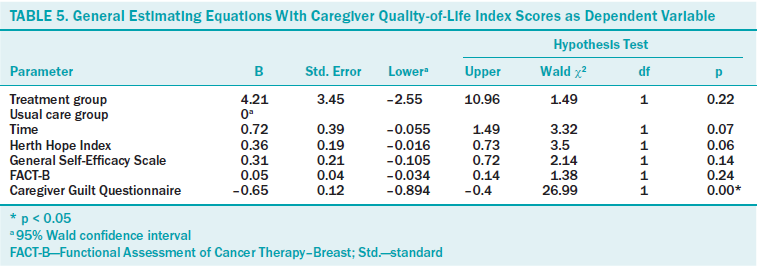
A significant predictor of male spouses’ CQOL-C scores was their perception of guilt (CGQ) (p < 0.01) (see Table 5). As male spouse participants’ feelings of guilt decreased (B = –0.65), their QOL increased. Other variables in the model that were not significant were time (p = 0.07), hope (p = 0.06), general self-efficacy (p = 0.14), and FACT-B (p = 0.24).
Usual Care Qualitative Data
The usual care group described the services they used to obtain information and healthcare services for their partners. They reported gathering information through seminars and workshops most often, but some mentioned looking online. One participant said, “I’ve done a bunch of research on the Internet on the disease and, you know, on the various, um, you know, treatments and why and where, and . . . and on the various comments.” Other participants said the only services they used were to support their partner. “So, we’ve been to the emergency hospital, and, uh, we’ve registered for home care.” Family and friends were important resources to some. “I’ve talked to a few people who have gone through this, um, so a lot of family and friends come over and they sit with us.” Others stated they did not access any additional services or resources. Overall, the data from the male spouse participants in the usual care group indicated they were not receiving services that would support them during their transitions.
Discussion
The quantitative and qualitative data from the MaTT evaluation questionnaire suggested that male spouse participants in the treatment group found MaTT was easy to use, acceptable, and feasible. The online format was helpful to participants because of its flexibility. This is similar to the findings of a review of web-based interventions to support caregivers of patients with cancer that suggested web-based interventions were feasible and acceptable to caregivers (Kaltenbaugh et al., 2015).
The critical sections of MaTT appeared to be the about me section and, within that section, the activities regarding the male caregivers’ roles and how they address the needs of their partner was the most frequently used. Correspondingly, in the changes to expect section, male spouse participants most frequently accessed information about their changing roles and relationships. This suggested that what to expect in terms of changes in roles and relationships was important information for the participants. Other sections of MaTT could potentially be removed based on participant comments or data regarding their use. However, whether the frequency of use of different sections of the MaTT is significantly related to the participants’ QOL is unclear.
MaTT is a multicomponent and flexible intervention which, as Kaltenbaugh et al. (2015) suggested, is an important characteristic of effective web-based interventions. However, this characteristic makes determining the amount of the intervention (dosage) needed for effectiveness challenging. Dosage of web-based interventions is unclear in the literature, and additional research is needed to determine ways to capture dosage (Kaltenbaugh et al., 2015), such as using web-based analytic tools to track individual participant’s access to the website, including which sections were accessed and for how long.
In terms of potential efficacy, the qualitative data suggest that MaTT does show promise in helping male spouses deal with transitions. The small sample size may be the reason for the nonsignificant treatment effect on male spouses’ QOL, hope, general self-efficacy, and guilt. It was appropriate for a feasibility study; however, the sample size required to determine a significant difference between the groups on day 28, based on study data, is estimated at 90 (45 per group).
Hope, general self-efficacy, and perceptions of guilt of the male spouse participants were hypothesized, based on the intervention model, to have a significant relationship to their QOL. Changes in these variables were considered to be the mechanisms through which QOL would increase in the treatment group. Only male spouse participants’ perceptions of guilt were a significant predictor of their QOL. Hope and guilt have been found in other studies with male spouses of women with breast cancer to have a significant relationship with their QOL (Duggleby, Bally, et al., 2012; Duggleby et al., 2015) and, therefore, should be maintained in the model. However, additional studies with larger sample sizes are needed to determine if the model should be revised.
Overall, participants in the intervention group found MaTT to be feasible and easy to use. The suggested changes for improving MaTT may increase its potential effectiveness. In addition, it was evident from the qualitative data that male spouses in the usual care group were receiving little to no services, thereby reinforcing the need for interventions, such as MaTT.
Limitations
Limitations to this study include the sample and study methods. The majority of the participants were Caucasian and English speaking. Because MaTT is a self-administered online intervention, the male spouses’ ability to read and understand the instructions would be an important aspect of its feasibility, ease of use, and acceptability. Given the participants were well educated (some post-secondary education, on average), they would likely not have found understanding the instructions difficult. The sample size was small and, by day 56, there were 21 in the treatment and 19 in the usual care group, making it difficult to determine a significant treatment effect. Future studies should include a more diverse and larger sample, including those with lower education levels and couples who had been married for shorter periods of time.
Because MaTT is a flexible intervention, the amount of time participants were to use it was not prescribed, and how frequently it was used was not captured. How frequently and for how long participants used MaTT may have influenced the impact of the intervention and should be captured in future research. Participants were instructed to use MaTT for four weeks. More participants agreed they were able to complete the activities they wanted to by day 28 versus day 14, and data from the latter time point indicated moderate effect sizes. This suggests that four weeks is a better time period for which to evaluate MaTT. However, it is possible that using it for even a longer period of time may increase its impact on male spouses’ QOL. Additional research is needed to determine the optimal length of time to obtain a significant benefit for male spouses.
Implications for Nursing Practice
Based on the findings, several changes in study design are suggested for future research. These changes include using individualized tracking of the use of MaTT through analytic tools, having a larger sample to determine the potential efficacy of MaTT for improving male spouses’ QOL, and enhancing study retention strategies to reduce study attrition. Potential ways to strengthen MaTT were also identified.
The male spouses’ perceptions of guilt had a significant influence on their QOL, suggesting that nurses should be aware of the potential impact of guilt on the health of male spouses of women with breast cancer. This awareness could lead to the nurses’ assessment and referral to resources and services for some male spouses.
The interviews with the usual care group highlighted the overall lack of support for male spouses of women with breast cancer, as echoed in other literature (Jones et al., 2013, Lewis et al., 2008). The development and evaluation of online interventions, like MaTT, are important because the interventions may be a feasible and acceptable way for nurses to share with and help support male spouses of women with breast cancer.
Conclusion
MaTT was found to be feasible and acceptable to male spouses of women with breast cancer and has the potential to help male spouses deal with the transitions they experience. However, additional studies with larger sample sizes is needed to determine its efficacy. The findings and limitations of this feasibility study will assist in the revision of MaTT and planning for future research.
About the Author(s)
Duggleby is a professor and research chair in aging and quality of life in the Faculty of Nursing at the University of Alberta in Edmonton; Ghosh is a research scientist for Alberta Health Services in Edmonton; Struthers-Montford is a PhD candidate in the Department of Sociology and Nekolaichuk is a professor in the Division of Palliative Care Medicine, both at the University of Alberta; Cumming is a psychologist at the Cross Cancer Institute in Edmonton; Thomas is a professor and Canada research chair in qualitative health research with marginalized populations in the School of Rehabilitation Sciences at the University of Ottawa in Ontario; Tonkin is a medical oncologist at the Cross Cancer Institute; and Swindle is a research coordinator in the Faculty of Nursing at the University of Alberta, all in Canada. This research was funded by the Canadian Breast Cancer Foundation, Alberta/Northwest Territories. Duggleby, Ghosh, Nekolaichuk, Cumming, Thomas, Tonkin, and Swindle contributed to the conceptualization and design. Duggleby, Struthers-Montford, Nekolaichuk, Cumming, Tonkin, and Swindle completed the data collection. Duggleby and Ghosh provided statistical support. All authors provided analysis and contributed to the manuscript preparation. Duggleby can be reached at wendy.duggleby@ualberta.ca, with copy to editor at ONFEditor@ons.org. Submitted December 2016. Accepted for publication June 27, 2017.
References
Ballinger, G.A. (2004). Using generalized estimating equations for longitudinal data analysis. Organizational Research Methods, 7(2), 127–150.
Birkett, M.A., & Day, S.J. (1994). Internal pilot studies for estimating sample size. Statistics in Medicine, 13, 2455–2463.
Borneman, T., Stahl, C., Ferrell, B.R., & Smith, D. (2002). The concept of hope in family caregivers of cancer patients at home. Journal of Hospice and Palliative Nursing, 4, 21–33.
Brady, M.J., Cella, D.F., Mo, F., Bonomi, A.E., Tulsky, D.S., Lloyd, S.R., . . . Shiomoto, G. (1997). Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. Journal of Clinical Oncology, 15, 974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Chih, M.Y., DuBenske, L.L., Hawkins, R.P., Brown, R.L., Dinauer, S.K., Cleary, J.F., & Gustafson, D.H. (2013). Communicating advanced cancer patients’ symptoms via the internet: A pooled analysis of two randomized trials examining caregiver preparedness, physical burden and negative mood. Palliative Medicine, 27, 533–543. https://doi.org/10.1177/0269216312457213
Cochrane, B.B., & Lewis, F.M. (2005). A partner’s adjustment to breast cancer: A critical analysis of intervention studies. Health Psychology, 24, 327–332. https://doi.org/10.1037/0278-6133.24.3 .327
Creswell, J.W., & Plano Clark, V.L. (2011). Designing and conducting mixed methods research. London, UK: Sage.
DuBenske, L.L., Gustafson, D.H., Shaw, B.R., & Cleary, J.F. (2010). Web-based cancer communication and decision making systems: Connecting patients, caregivers, and clinicans for improved health outcomes. Medical Decision Making, 30, 732–744. https://doi.org/10.1177/0272989X10386382
Duggleby, W., Bally, J., Cooper, D., Doell, H., & Thomas, R. (2012). Engaging hope: The experiences of male spouses of women with breast cancer. Oncology Nursing Forum, 39, 400–406. https://doi.org/10.1188/12.ONF.400-406
Duggleby, W., Doell, H., Cooper, D., Thomas, R., & Ghosh, S. (2014). The quality of life of male spouses of women with breast cancer: Hope, self-efficacy and perceptions of guilt. Cancer Nursing, 37(1), E28–E35. https://doi.org/10.1097/NCC.0b013e31827ca807
Duggleby, W., Thomas, J., Montford, K., Thomas, R., Nekolaichuk, C., Ghosh, S., . . . Tonkin, K. (2015). Transitions of male partners of women with breast cancer: Hope, guilt, and quality of life. Oncology Nursing Forum, 42, 134–141.
Duggleby, W., Wright, K., Williams, A., Degner, L., Cammer, A., & Holtslander, L. (2007). Developing a living with hope program for caregivers of family members with advanced cancer. Journal of Palliative Care, 23, 24–31.
Duggleby, W.D., Cooper, L.J., Leipert, B.D., Wilson, D.M., Williams, A., Marshall, D., . . . Taniguichi, A. (2012). Development of a “changes toolkit” for rural older palliative patients and their family caregivers. Journal of Rural and Community Development, 7(4), 62–75.
Farnham, S., Cheng, L., Stone, L., Zaner-Godsey, M., Hibbeln, C., Syrjala, K., & Abrams, J. (2002). HutchWorld: Clinical study of computer-mediated social support for cancer patients and their caregivers. Paper presented at the SIGCHI Conference on Human Factors in Computing Systems: Changing Our World Changing Ourselves, Minneapolis, MN.
Ghisletta, P., & Spini, D. (2004). An introduction to generalized estimating equations and an application to assess selectivity effects in a longitudinal study on very old individuals. Journal of Educational and Behavioral Statistics, 29, 421–437. https://doi.org/10.3102/10769986029004421
Herth, K. (1992). Abbreviated instrument to measure hope: Development and psychometric evaluation. Journal of Advanced Nursing, 17, 1251–1259.
Jones, J.M., Lewis, F.M., Griffith, K., Cheng, T., Secord, S., Walton, T., . . . Catton, P. (2013). Helping Her Heal–group: A pilot study to evaluate a group delivered educational intervention for male spouses of women with breast cancer. Psycho-Oncology, 22, 2102–2109. https://doi.org/10.1002/pon.3263
Kaltenbaugh, D.J., Klem, M.L., Hu, L., Turi, E., Hains, A.J., & Hagerty Lingler, J. (2015). Using web-based interventions to support caregivers of patients with cancer: A systematic review. Oncology Nursing Forum, 42, 156–164. https://doi.org/10.1188/15.ONF.156-164
Krippendorff, K. (2012). Content analysis: An introduction to its methodology (3rd ed.). Los Angeles, CA: Sage.
Lewis, F.M., Cochrane, B.B., Fletcher, K.A., Zahlis, E.H., Shands, M.E., Gralow, J.R., . . . Schmitz, K. (2008). Helping Her Heal: A pilot study of an educational counseling intervention for spouses of women with breast cancer. Psycho-Oncology, 17, 131–137. https://doi.org/10.1002/pon.1203
Liu, S., Dixon, J., Qui, G., Tian, Y., & McCorkle, R. (2009). Using generalized estimating equations to analyze longitudinal data in nursing research. Western Journal of Nursing Research, 31, 948–964. https://doi.org/10.1177/0193945909336931
Losada, A., Márquez-González, M., Peñacoba, C., & Romero-Moreno, R. (2010). Development and validation of the caregiver guilt questionnaire. International Psychogeriatrics, 22, 650–660.
Luszczynska, A., Gutiérrez-Doña, B., & Schwarzer, R. (2005). General self-efficacy in various domains of human functioning: Evidence from five countries. International Journal of Psychology, 40(2), 80–89. https://doi.org/10.1080/00207590444000041
Luszczynska, A., Mohamed, N.E., & Schwarzer, R. (2005). Self-efficacy and social support predict benefit finding 12 months after cancer surgery: The mediating role of coping strategies. Psychology, Health and Medicine, 10, 365–375. https://doi.org/10 .1080/13548500500093738
McKenzie, J., & Smelzer, J. (1997). Planning, implementing and evaluating health promotion programs: A primer (2nd ed.). Boston, MA: Allyn and Bacon.
Meilis, A.I. (Ed.). (2010). Transitions theory: Middle range and situation-specific theories in nursing research and practice. New York, NY: Springer.
Munro, B.H. (2005). Statistical methods for health care research. Philadelphia, PA: Lippincott Williams & Wilkins.
Namkoong, K., DuBenske, L.L., Shaw, B.R., Gustafson, D.H., Hawkins, R.P., Shah, D.V., . . . Cleary, J.F. (2012). Creating a bond between caregivers online: Effect on caregivers’ coping strategies. Journal of Health Communication, 17, 125–140. https://doi.org/10.1080/10810730.2011.585687.
Scott, K., & Beatty, L. (2013). Feasibility study of a self-guided cognitive behaviour therapy internet intervention for cancer carers. Australian Journal of Primary Health, 19(4), 270–274. https://doi.org/10.1071/PY13025
Struthers-Montford, K., Duggleby, W., Cumming, C., Thomas, R., Nekolaichuk, C., Ghosh, S., & Tonkin, K. (2016). ‘All I can do is help’: Transition experiences of male spouse caregivers of women with breast cancer. Canadian Oncology Nursing Journal, 26, 312–317.
Timmreck, T.C. (1995). Planning, program development, and evaluation: A handbook for health promotion, aging, and health sciences. Boston, MA: Jones and Bartlett.
Weitzner, M.A., Jacobson, P.B., Wagner, H., Jr., Friedland, J., & Cox, C. (1999). The Caregiver Quality of Life Index–Cancer (CQOL-C) scale: Development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality Life Research, 8, 55–63.
Zahlis, E.H., & Lewis, F.M. (2010). Coming to grips with breast cancer: The spouse’s experience with his wife’s first six months. Journal of Psychosocial Oncology, 28, 79–97. https://doi.org/10.1080/07347330903438974
Zulman, D.M., Schafenacker, A., Barr, K.L., Moore, I.T., Fisher, J., McCurdy, K., . . . Northouse, L. (2012). Adapting an in-person patient-caregiver communication intervention to a tailored web-based format. Psycho-Oncology, 21, 336–341.

