Oncology Nursing Perceptions of Patient Electronic Portal Use: A Qualitative Analysis
Purpose/Objectives: To identify nursing staff reactions to and perceptions of electronic portal use in a cancer setting.
Research Approach: Qualitative.
Setting: Outpatient clinic at the Harold C. Simmons Comprehensive Cancer Center of the University of Texas Southwestern Medical Center in Dallas.
Participants: 13 nurses with a range of credentials and experience, representing infusion, medical oncology, and bone marrow transplantation clinics.
Methodologic Approach: Two focus groups were conducted. Theoretical thematic content analysis of data was performed.
Findings: Key themes that emerged for consideration of electronic portals included work volume and flow, patient expectations and safety, variation in use of communication technologies, and education and management.
Interpretation: The current study provides insight into the implications of electronic portals by identifying nursing staff reactions to this technology. These reactions are predominantly related to the impact on clinical workload and patient safety and expectations.
Implications for Nursing: As clinical cancer facilities incorporate electronic portal technology into their operations, attention to the impact on staff workload, division of labor, patient safety, and patient expectations should be considered.
Jump to a section
The electronic health record (EHR) is widely implemented in clinical practices (Fernald, Wearner, & Dickinson, 2013; Jain, Seidman, & Blumenthal, 2010; Krist et al., 2014). Bolstered by government prioritization and support, the EHR has seen uptake in primary care and specialty practices, emergency departments, and inpatient facilities (Office of the National Coordinator for Health Information Technology, 2010). Within the EHR, electronic portals have been designed to enhance the timeliness, efficiency, transparency, and patient-centeredness of care (Feeley & Shine, 2011). Electronic portals provide patients with real-time access to their personal patient health records (PHRs) and communication with healthcare providers (Fisher, Bhavnani, & Winfield, 2009). Patients who opt to use the electronic portal may view upcoming appointments; personal health information, such as allergies, medications, social history, family history, and medical history; and laboratory and radiology results. In addition, portals may allow patients to communicate electronically with clinic staff members and medical providers (Hassol et al., 2004; Ralston, Coleman, Reid, Handley, & Larson, 2010). Such communication can include making appointment and medication refill requests, asking clinical questions, and reporting symptom development or changes.
As access to personal computers and mobile devices expands, so have availability and use of electronic portals. Research to understand the implications of these new tools on clinical practice and patient care is growing (Kaelber, Jha, Johnston, Middleton, & Bates, 2008; Kruse, Bolton, & Freriks, 2015; Liss et al., 2014; Murphy et al., 2016; Nazi et al., 2010). Implementation and uptake of this technology in oncology may introduce particular considerations (Beard, Schein, Morra, Wilson, & Keelan, 2012; Honeyman, Cox, & Fisher, 2005). With close clinic follow-up, frequent laboratory testing, and multiple imaging, the longitudinal outpatient care of individuals with cancer is more intensive than that of many other specialties, possibly leading to increased EHR and PHR data flow (Feldman & Rodriguez, 2012). Laboratory and radiology results could represent important clinical developments, such as disease progression. Alternatively, abnormalities that have no clinical significance may still result in anxiety and confusion when viewed outside of clinical visits without concurrent provider interpretation and explanation (Ward, 2012). In addition, because of the potentially aggressive nature of the underlying cancer, symptoms reported electronically by patients with cancer may be more likely to represent medical urgencies than symptoms reported by non-oncology populations. How these text messages are handled by clinical practices and providers raises important questions about patient safety and satisfaction (Rodriguez, 2010; Wiljer et al., 2010).
In an earlier study, Gerber et al. (2014) confirmed that PHR portal use by patients with cancer is frequent and increasing. A subsequent analysis demonstrated that, among healthcare professionals, nonphysician clinical personnel, particularly nurses, are handling the majority of this communication (Laccetti et al., 2015). Because nursing perception of the impact of electronic patient portal use has not been extensively studied, the authors conducted focus groups with nurses in their cancer center to explore this.
Methods
The current study was conducted in the outpatient clinics of the National Cancer Institute (NCI)–designated Harold C. Simmons Comprehensive Cancer Center at University of Texas (UT) Southwestern Medical Center in Dallas. The study team worked with clinic nursing managers to invite nurses to participate in focus group sessions by group email, with follow-up invitations issued at staff meetings by nurse managers (eligible: n = 47). To limit the possibility of recruiting a study sample inherently biased toward or against the electronic patient portal paradigm, the authors described the topic of the planned focus groups as a general examination of various means of communication between clinical staff, patients, and physicians within the cancer center. To limit bias among potential participants in the second group, participants from the first session were specifically instructed not to discuss the content of the group or the identities of participants with other nurses. Sessions were conducted in a small conference room adjacent to the clinics; snacks and beverages were provided as an acknowledgement of participant time and engagement. No direct incentives were offered. The study was approved by the UT Southwestern Institutional Review Board.
Focus Group Conduct
To explore implications of patient health portals on clinical care and nursing activities, the investigator team generated a discussion guide (see Figure 1) covering a range of issues related to electronic patient portal use within the cancer center. The focus groups were moderated by a senior qualitative scientist. Physician members of the research team and nursing supervisors did not attend the focus groups to limit observer effects on participant responses and discussion. The authors provided information sheets to participants and solicited informed oral consent per protocol. Using the discussion guide to initiate conversation, the moderator posed a question to the group, then elicited comments from participants through prompts and follow-up queries, allowing unstructured time for participants to compare and contrast their experiences and opinions with one another. As the second session proceeded through the discussion guide, the moderator presented initial comments from the first session to check credibility and confirmability. Each focus group was audio recorded and subsequently transcribed verbatim by a professional contractor.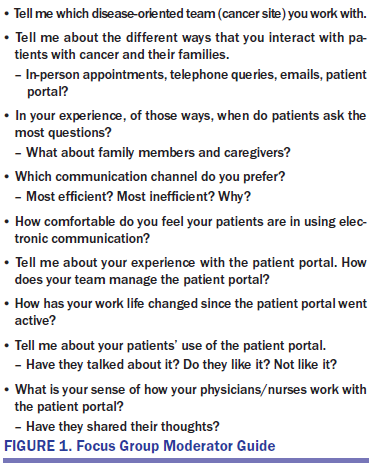
Analysis
After both focus groups were completed, the research team sequentially reviewed transcripts and assessed issues raised using an inductive, text-driven approach to thematic content analysis (Creswell, 1988; Miles & Huberman, 1994). The investigators collectively identified preliminary themes, leading to theme consolidation and extraction, with subsequent iterative discussion and analysis by the entire team; this also allowed them to address discrepancies by consensus (Cohen & Crabtree, 2008; Mays & Pope, 1995). To explicitly address issues of credibility and confirmability, the two nursing supervisor investigators reviewed identified themes against transcript excerpts.
Results
Thirteen outpatient nurses agreed to participate (28% response rate) in two sessions (n = 6, n = 7) conducted on two sequential days. Five participants represented the infusion clinic, and eight represented medical oncology, two of whom represented additional service in bone marrow transplantation clinics. Overall credentials included RN, BSN, CCRN, and OCN®; cancer-related clinical experience ranged from one month to 10 years at the Harold C. Simmons Comprehensive Cancer Center and 1–24 years overall.
Participants reported a number of factors that they described as advantages and disadvantages of the electronic patient portal. The author consolidated these issues to identify four major themes that classify nurses’ reasoning (see Figure 2).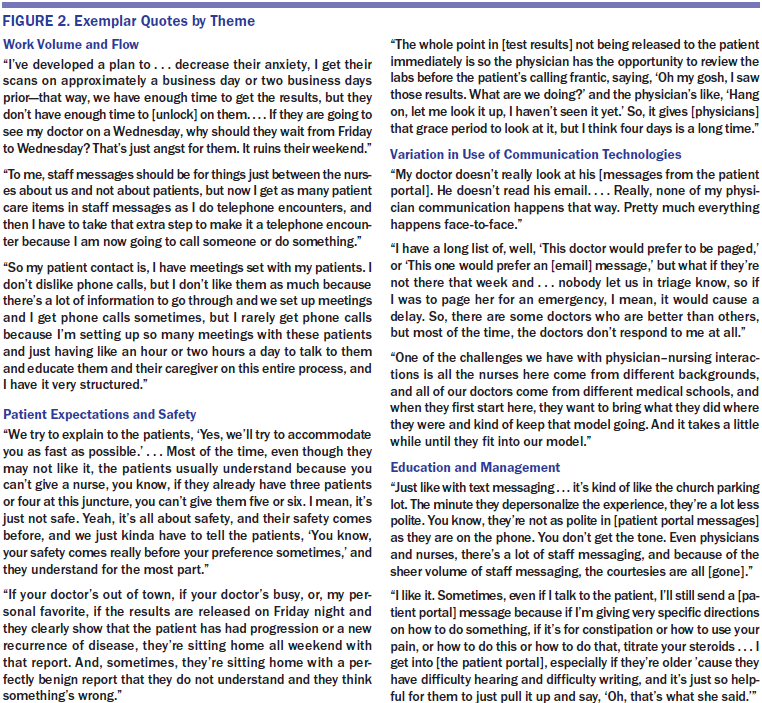
Work Volume and Flow
The primary consideration of this technology was its impact on work volume and flow. Nurses raised concerns about the perceived substantial increase in the volume of electronic communications, burden of documentation, potential for multiple exchanges between patients and staff members (contrasted to a single telephone or in-person exchange), and increase in the number of steps and staff members involved in a given communication thread. To improve efficiency, participants raised the possibility of a central triage system for electronic communication, drawing analogy to the telephone call triage program in place at the authors’ center. Others described using a communication function that prevented patients from replying within the portal, only to find that patients would instead initiate a new message thread.
Patient Expectations and Safety
Patient expectations and safety also emerged as central concerns. In an era when text messaging has become standard communication practice across society, nurses reported that many patients appear to expect immediate responses to their inquiries or status updates. Nurses described numerous examples of patients or caregivers using the portal to report medical emergencies and expressed concern when patients reacted adversely to electronic communication with unedited medical or technical language, with particular reference to automated release of laboratory results (Cahill, Gilbert, & Armstrong, 2014).
Variation in Use of Communication Technologies
Nurses reported notable differences in the workflow of how patient portal communications were handled between physicians in the same clinic. Physician seniority, behavior traits, and clinical expertise (clinician versus researcher) were cited as potential factors affecting this workflow. Impact of electronic portals on other aspects of clinical practice was also noted. For instance, nurses described the challenges and stresses of staying abreast of portal upkeep (i.e., managing their inboxes) while simultaneously seeing patients in the clinic. Others described altering the scheduling of key diagnostic tests, such as radiology studies, and provider clinic appointments to ensure that test results were not released electronically to the patient prior to the office visit.
Education and Management
Nursing staff members provided numerous suggestions for streamlining workflow and improving patient and staff experience. Increasing patient and caregiver education regarding appropriate use and expectations was a widely agreed upon approach. However, a number of participants felt that no amount of counseling would prevent all patients from using the portal to report medical emergencies or matters irrelevant to their clinical care.
Nursing staff members also cited a number of benefits of portals for patient care and clinic workflow. In some situations, nurses preferred the slower timeline of electronic communication to the immediacy of telephone conversations, allowing nurses to discuss and research their responses before answering questions. The written format, as opposed to telephone speech, was also described as advantageous for some patients because instructions regarding medication usage or future appointments could be reviewed by the patient or caregiver at home, whereas directions received by telephone may be forgotten or not understood.
Discussion
Focus group methodology has been applied extensively in health care and medical research (Gerber, Hamann, Rasco, Woodruff, & Lee, 2012; Ritchie, Herscovitch, & Norfor, 1994). Focus groups provide a means to solicit patient and provider opinions of clinical issues (Barbour, 2005; Krueger & Casey, 2000). They have the added value of group dynamics, as participants are free to react to others’ comments and further develop discussion beyond that initially anticipated by the investigators. Given the potential reluctance for nurses to discuss personal opinions and concerns with physicians or practice administrators, focus groups may yield particular insight into these reactions.
To the authors’ knowledge, this is the first qualitative study of nurse attitudes and beliefs assessing the impact of PHR portal technology in an oncology setting. Results from the two focus groups suggest that electronic patient portals represent an area of considerable significance to nursing staff within a regional cancer center, supporting early implementation reports of PHR prototypes in cancer care (Rodriguez, Thom, & Schneider, 2011) and emerging studies conducted among primary care physicians in Veterans Health Administration health systems (Nazi, 2013).
Although multiple members of the healthcare team, including clerical staff, nurses, midlevel providers, and physicians, interface with the patient portal, the authors elected to focus on nursing staff because their preliminary research demonstrated that they carry out the majority of tasks related to portal activities (Laccetti et al., 2015). Prior studies have suggested that physician awareness of PHR and their engagement with the technology may be low (Fuji, Galt, & Serocca, 2008). In contrast, nurses are able to provide a unique, multidirectional perspective, as they carry out portal activities themselves and also communicate with patients in a variety of settings (portal, telephone, in-person encounters), allowing them to provide insight not only into their own reactions to portal technology, but also into their perceptions of patient experience. In contrast to a prior survey, the current findings suggest that oncology nursing staff members have real concerns about increasing workload as patient portal use rises (Rodriguez et al., 2011). In this regard, the current findings reflect the organizing framework advocated by Veterans Health Administration research emphasizing PHR adoption (Nazi et al., 2010). By elucidating actual communication and process strategies within oncology clinical practice, the current study advances understanding of the dynamics of PHR integration beyond studies of initial uptake (Nazi, 2013).
Patients with cancer frequently develop networks of family members and advocates who may be deeply involved with day-to-day activities and treatment decisions. Family members and other caregivers are increasingly granted access by patients to their electronic portal to organize aspects of clinical care, such as office appointments. Communication initiated by patient advocates using the patient portal provides an extra layer of nonconventional communication, with implications for patient autonomy, privacy, and flow of personal health information that warrant additional study.
Limitations
Limitations of the current study include the single-center setting, relatively small number of participants, and factors inherent to the focus group design. As an NCI–designated comprehensive cancer center located in a major metropolitan area, the patient population may not be representative of the broader oncology population and may be potentially more educated and motivated regarding their cancer diagnoses and treatment (Ballard et al., 1994; Onega, Duell, Shi, Demidenko, & Goodman, 2009). In turn, these characteristics may result in distinct patterns of portal use and reactions (Goel et al., 2011), affecting the nursing experience and perceptions. The authors are also aware that workflow of patient portal communications may vary between outpatient oncology practices, as participants themselves noted. Although the findings come from a single academic cancer center, these themes can be broadly applied across practice types with respect to staff and patient communications and workflow. Despite the relatively small number of participants, the study sample constitutes a broad range of nursing credentialing and clinical experience at the authors’ site and elsewhere. The analysis revealed sufficient thematic repetition to suggest saturation whereby major nursing experiences and perceptions were identified across the two focus groups. Inherent to focus group design, potential exists for group dynamics to suppress objections or disagreements. However, moderator tactics may be employed to establish group rapport through experiential commonalities, particularly in small group settings. In the current study, the moderator deliberately prepared participants for contrasting answers and encouraged participants to compare their own and patients’ experiences among one another. A risk also exists of employees behaving in a manner they believe is desired by their supervisors. To minimize this effect, the authors explicitly excluded nursing supervisors and physicians from focus group discussions.
[[{"type":"media","view_mode":"media_original","fid":"30146","attributes":{"alt":"","class":"media-image","height":"263","typeof":"foaf:Image","width":"367"}}]]
Conclusion
Electronic patient portals appear to have had a major impact on outpatient oncology nursing in the authors’ setting. The current study demonstrates that nurses devote considerable effort to portal activities. Key nursing themes that emerged include work volume and flow, patient expectations and safety, variation in use of communication technologies, and education and management. Although a study of this nature is not definitive, the findings suggest that oncology practices and cancer centers may wish to address portal implementation and function among clinical staff on a regular basis to deal with emerging concerns. Such an approach will become increasingly important as the number of patients with cancer grows nationwide, these patients live longer, treatment regimens become more complex, and a greater proportion of the population embraces electronic communication.
The authors gratefully acknowledge Dru Gray for assistance with manuscript preparation.
About the Author(s)
Gerber is an associate professor and Beg is an assistant professor, both in the Division of Hematology-Oncology; Duncan is an infusion room supervisor; Gill is a nursing supervisor of hematology-oncology; and Lee is an associate professor in the Department of Clinical Sciences, all at the Harold C. Simmons Comprehensive Cancer Center of the University of Texas Southwestern Medical Center in Dallas. This research was supported by a National Cancer Institute (NCI) Midcareer Investigator Award in Patient-Oriented Research (1K24CA201543-01; principal investigator: Gerber) and by the University of Texas Southwestern Center for Patient-Centered Outcomes Research through a grant from the Agency for Healthcare Research and Quality (R24 HS022418; co-investigator: Lee). Additional support was provided by the NCI Cancer Center Support Grant (2P30 CA142543-06). Beg is supported by the Dedman Family Endowed Program for Scholars in Clinical Care. Gerber, Beg, and Lee contributed to the conceptualization and design and the manuscript preparation. Gerber and Lee provided the analysis. All of the authors completed the data collection. Gerber can be reached at david.gerber@utsouthwestern.edu, with copy to editor at ONFEditor@ons.org. Submitted April 2016. Accepted for publication June 20, 2016.

