Establishing Priorities for Oncology Nursing Research: Nurse and Patient Collaboration
Purpose/Objectives: To obtain consensus on priorities for oncology nursing research in the United Kingdom.
Design: A three-round online Delphi survey.
Setting: Oncology nurses were invited via the United Kingdom Oncology Nursing Society (UKONS) database. Patient participation was invited through patient organizations.
Sample: 50 oncology nurses and 18 patients.
Methods: Eligible and consenting individuals reported five priorities for oncology nursing research (round 1), rated their level of agreement with them (round 2), and restated and revised their responses in light of the group’s responses (round 3). Consensus was defined as 80% agreement.
Main Research Variables: Research priorities for oncology nursing as reported by oncology nurses and patients.
Findings: Consensus was reached on 50 of 107 research priorities. These priorities reflected the entire cancer pathway, from diagnosis to palliative care. Highest agreement was reached within and across groups on the need for research relating to prevention, screening, early diagnosis, and psychological care across the cancer trajectory. Little consensus was reached regarding symptoms and side effects. Some evident divergence existed: Only patients reached consensus regarding palliative care research, and only nurses reached consensus regarding eHealth and technology research.
Conclusions: Oncology nurses and patients do not necessarily prioritize the same research areas. Prevention, screening, and early diagnosis are of the highest priority for future research among oncology nurses and patients.
Implications for Nursing: Patients usually play little part in priority setting for research. This study provided the opportunity for meaningful patient and nurse involvement in setting a research agenda for oncology nursing that is relevant and beneficial to oncology nurses and patients.
Jump to a section
Cancer care is in continual flux, driven by advances in science, technology, and treatment. Improvements have been made across cancer services, including in the areas of prevention, screening (e.g., home testing kits for colorectal cancer), surgery (e.g., robotic surgical systems), chemotherapy (e.g., cancer immunotherapy), and enhanced recovery and survivorship programs. Many innovations have enabled care to be delivered closer to people’s homes with benefits in terms of patient convenience and cost savings for service providers. However, innovations in cancer care alter patients’ interactions with cancer services, as well as the care they require. Nursing care needs to be responsive to service changes and patient outcomes, and it should be underpinned by contemporary and rigorous evidence addressing key challenges for nurses and patients. Because finite resources are available, research needs to be strategic and directed in such a way to ensure an appropriate evidence base that is fit for purpose and targeted at key priorities. Consequently, nurses and other health professionals in cancer care must periodically reflect on and seek consensus regarding priorities for future research—the focus of this article.
Background
Research priorities have been surveyed and reported within oncology nursing since the 1970s (Oberst, 1978). More recently, consensus-building exercises have been undertaken in the United States, United Kingdom, Northern Ireland, Norway, Australia, and across Europe (Barrett, Kristjanson, Sinclair, & Hyde, 2001; Browne, Robinson, & Richardson, 2002; Cohen, Harle, Woll, Despa, & Munsell, 2004; Grundy & Ghazi, 2009; McIlfatrick & Keeney, 2003; Rustøen & Schjølberg, 2000; Soanes, Gibson, Bayliss, & Hannan, 2000; Soanes, Gibson, Hannan, & Bayliss, 2003; Wright, Corner, Hopkinson, & Foster, 2006). Typically, a Delphi survey design—a validated consensus method—has been used. Delphi surveys seek to identify and attain consensus on priorities through an iterative process of about three questionnaire rounds. The Delphi process usually begins with open questions requiring participants to make recommendations. Subsequent rounds are more focused and request participants to rate their agreement with proposed recommendations. Participants are provided with results from previous rounds, allowing them to re-rate their agreement until consensus is reached.
Participants in expert panels for consensus studies related to oncology nursing have typically been oncology nurses, although some researchers—having established nurses’ priorities—have sought to validate findings from the user perspective (Soanes et al., 2003). A similar trend is evident in other healthcare disciplines. A systematic mapping exercise of research prioritization in healthcare by the James Lind Alliance (Stewart & Oliver, 2008) determined that research priorities are driven more frequently by clinicians than by patients. Only 18% of the 258 studies included in the James Lind Alliance mapping exercise elicited patients’ views on research; the remainder solely sought those of clinicians. In addition, clinicians and patients were determined to identify research topics in isolation. Few studies (19%) incorporated perspectives of both groups. This has shortcomings because research priorities perceived as important by patients may be omitted.
The importance of increasing opportunity for patients and the public to participate in and benefit from research is evident in the formation of national advisory groups that support active public involvement in health and social care research (e.g., INVOLVE in the United Kingdom, National Institutes of Health Director’s Council of Public Representatives in the United States, European Cancer Patient Coalition in Europe).
Patient involvement in priority setting for nursing research has been recognized as valuable (Soanes et al., 2000). Having completed a Delphi survey of nurses’ priorities for nursing research across various pediatric settings (i.e., hematology, oncology, immunology, and infectious diseases), Soanes et al. (2000) then consulted with doctors and parents of children who were receiving treatment for mainly hematologic or oncologic conditions on the priorities identified (Soanes et al., 2003). The majority of parents confidently proposed priorities without assistance and only occasionally needed clarification of terms. In addition, general agreement on the ranking of top priorities existed among nurses, doctors, and parents. However, although Soanes et al. (2003) sought to validate their prioritization of nursing research with stakeholders, including parents, their work was not strongly collaborative; users were not involved in initial rounds of the Delphi survey. This may have narrowed topics promoted for consideration and omitted those of importance to parents.
Corner et al. (2007) conducted a consultation with people living with cancer in the United Kingdom concerning future research. An exploratory, qualitative approach, which combined focus groups with an adapted nominal group technique to structure discussion and achieve consensus, was used to elicit patients’ views (Corner et al., 2007). This study demonstrated that people living with cancer “are able to engage with a broad range of issues relating to science, medicine, health and social care, the purpose and value of cancer research and can identify and agree on priorities” (Corner et al., 2007, p. 878). Importantly, a mismatch was reported between patient-identified research priorities that attained consensus and the U.K. research portfolio.
Until the current study, oncology nursing had not provided an example of collective priority setting by nurses and patients. However, examples of such collaboration exist in the U.K. physiotherapy (Rankin, Rushton, Olver, & Moore, 2012) and osteopathic professions (Rushton, Fawkes, Carnes, & Moore, 2014). Rankin et al. (2012) and Rushton et al. (2014) concluded that inclusion of multiple stakeholders in consensus seeking increased saliency of the priorities identified.
The aim of the current study was to establish priorities for U.K. oncology nursing research through nurses’ and patients’ collaboration in a Delphi survey. The intention was that identified priorities would underpin a research agenda that (a) is relevant and beneficial to oncology nurses and patients, (b) is widely implemented, and (c) has the capacity to drive forward the discipline of oncology nursing for the benefit of patients. The survey sought to answer the following questions:
• What are U.K. oncology nurses’ research priorities?
• What are the research priorities of people living with cancer in the United Kingdom?
• Do oncology nurses and people living with cancer in the United Kingdom have similar priorities for oncology nursing research?
• Are oncology nurses and people living with cancer in the United Kingdom able to reach consensus on priorities for oncology nursing research?
Methods
A three-round online Delphi survey was undertaken and was facilitated through SmartSurvey, a U.K.-based provider of digital survey solutions. The Delphi technique is a process of structured group communication designed to reach consensus among a panel of experts; it is an iterative process of two or more rounds where selected experts are asked to generate and then prioritize research topics. This approach enables experts who are geographically dispersed to participate in the process with relatively little inconvenience and expense in terms of time and finance. The semi-anonymity and remoteness provided by the Delphi approach allows individual opinions to be expressed without the influence of dominant fellow experts, facilitating progression from individual opinion to group consensus.
Sample
Nurse participants: A panel of oncology nursing experts was purposively selected from the United Kingdom Oncology Nursing Society (UKONS) database by a medical communications agency that acts as UKONS’s secretariat. UKONS is an organization run by oncology nurses, with more than 3,400 registered members from across the United Kingdom. UKONS’s members were eligible for invitation to the expert panel if they were a resident of England, Northern Ireland, Scotland, or Wales; held the job title of clinical nurse specialist, advanced practitioner, or nurse consultant, or were a university academic; had conducted most of their current work within the area of adult oncology; and had at least five years’ experience in cancer care. The medical communications agency selected a purposively diverse sample (in regard to geographic location and speciality [oncology versus hematology]) from those potentially eligible and invited them, via email, to participate in the survey.
Patient participants: Patient experts were sought through five patient organizations: (a) Independent Cancer Patients’ Voice, a patient advocate group that aims to bring patients’ voices into clinical research (www.independentcancerpatientsvoice.org.uk); (b) The Rarer Cancers Foundation, an organization that raised awareness about less common cancers and acted as a gateway, directing patients to additional avenues of support and information; (c) Kidney Cancer Support Network, a patient-led network of people living with kidney cancer, as well as caregivers and families affected by kidney cancer (www.kcsn.org.uk); (d) Cancer Partnership Research Group in the Kent Surrey and Sussex Clinical Research Network, a partnership group whose main aim was to involve patients and caregivers in cancer research; and (e) North Trent Cancer Research Network Consumer Research Panel, a consumer research panel whose purpose is to engage consumers, including people living with cancer and caregivers, in the process of research (www.ntcrp.org.uk/page3.html). Eligible patients were aged older than 18 years; resided in England, Northern Ireland, Scotland, or Wales; and had received a diagnosis of cancer. These patient organizations promoted the study through social media and online patients’ forums, as well as via email invitations. Potentially eligible participants (nurses and patients) emailed the research team to express their interest in participating. They provided written consent and completed a screening questionnaire to confirm eligibility.
Fifty nurses agreed to participate from the 707 UKONS nurses who were purposefully sampled. Many (n = 32) had earned a master’s degree or higher, and most (n = 47) identified as White (see Table 1). Eighteen patients agreed to participate; of these, 8 had a diagnosis of breast cancer, and 16 identified as White. All patients lived in England (see Table 2). 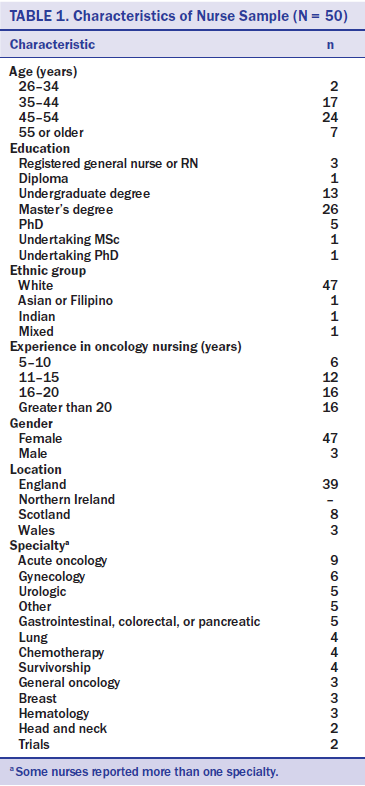
Instrument
Round 1: The first round of the Delphi survey asked participants to record five important issues or problems in oncology nursing that they felt should be researched in the United Kingdom. It also asked them to confirm whether they knew of the study through either nursing or patient organizations and to provide some basic demographic information. Patient participants were offered the option to complete the initial survey by telephone if they preferred to allow clarification of meaning for patient and interviewer. However, survey administration by telephone was neither requested nor used. 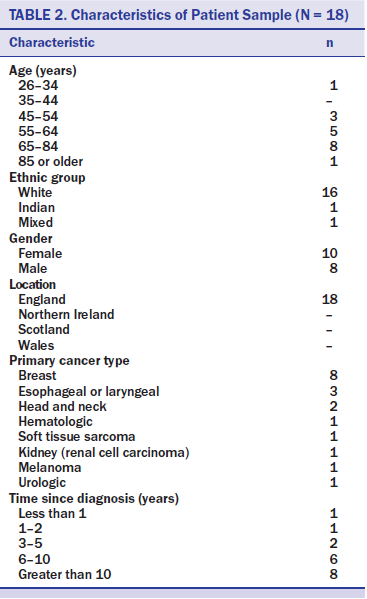
Round 2: Two members of the research team aggregated participants’ priorities—recorded in response to the round 1 survey—through content analysis. They coded data independently, then compared and discussed their coding until agreement was reached regarding the statements of research priorities to be included in the round 2 questionnaire. Other members of the team reviewed this process to ensure that identified research priorities accurately incorporated and reflected responses to round 1.
Participants were asked to indicate how strongly they agreed with each listed research priority on a five-point Likert-type scale ranging from 1 (strongly agree) to 5 (strongly disagree). Priorities were grouped in themes for ease of organization. A free text box was available at the end of each theme for participants to add comments or propose additional questions or priorities for that particular theme.
Round 3: In round 3, the survey comprised all research priorities from round 2 with the addition of new items raised by participants. In this final round, participants were also sent their own response to each research priority from round 2, as well as the average group response to each. This offered an opportunity for participants to restate or change their response from round 2 in light of the group response.
Agreement has not been reached over the appropriate level of consensus to adopt in Delphi studies, although 75% has been proposed as the minimum (Keeney, Hasson, & McKenna, 2006). In the current study, consensus was defined as 80% or more respondents rating an item as “agree” or “strongly agree.”
Procedures
The medical communications agency that acts as UKONS’s secretariat emailed consenting eligible participants the link to each of the three online survey questionnaires in turn, alongside their unique participant number. Three reminder emails were sent over three weeks to nonresponders, unless they requested not to be contacted again. Only an authorized member of the medical communications agency and study researchers had access to respondents’ data.
The Delphi survey in round 1 was emailed to 70 participants and generated a response from 68 of them (97% response rate). Respondents listed their top five priorities for nursing research; analysis of these data generated 95 statements that fell within 12 themes. These comprised the statements incorporated within the round 2 questionnaire. The round 2 questionnaire was mailed to the 68 responders to round 1 and generated a 91% response rate (n = 62). Responses to the free text questions generated an additional 12 priorities; these were incorporated within the final (round 3) questionnaire. The round 3 questionnaire was mailed to the 68 responders to round 1 and generated 60 responses (88% response rate). All 18 patients responded to each of the questionnaires. The research proposal and accompanying documents were submitted to the University of Surrey Ethics Committee for ethical scrutiny, and approval was obtained before recruitment commenced (UEC/2015/059/FHMS).
Analysis
Responses to the first Delphi survey questionnaire were analyzed thematically. Thereafter, in rounds 2 and 3, responses to items (research priorities) were coded (1 = strongly agree, 2 = agree, 3 = no opinion, 4 = disagree, 5 = strongly disagree). These data were analyzed descriptively to generate percentage agreement with, as well as mean values and standard deviations for, each priority.
Results
The 107 priorities for oncology nursing research—proposed by participants during the Delphi survey process—fell within 12 broad themes: prevention, screening, and diagnosis; treatment decision making; symptoms and side effects; psychosocial care needs; communication; survivorship and rehabilitation; palliative and end-of-life care; the cancer workforce; service models; diversity and inequality; family and carers; and dissemination and implementation.
Nurses proposed 71 of the research priorities, patients proposed 14, and 22 were proposed by both groups. Priorities that were promoted only by patients—that would have been omitted had nurses been the only contributors—fell within four broad areas: (a) management of symptoms where little is known either about mechanisms responsible for their onset or their pharmacologic management (fatigue and peripheral neuropathy); (b) role of patient-led factors (diet and faith) in patient well-being; (c) interface with palliative care services; and (d) rehabilitation (including return to work) and follow-up.
Consensus Across Nurses and Patients
Consensus was reached on 47% (n = 50) of the 107 research priorities (see Table 3). Of the 14 proposed only by patients, 7 reached consensus across patients and nurses. These related to (a) management of peripheral neuropathy, (b) impact of diet on cancer treatment and outcomes, (c) when and how palliative care services are introduced, (d) integration of palliative care within oncology services, (e) structured rehabilitation and support programs for patients living with or after cancer, (f) interventions to facilitate return to work following treatment, and (g) patients’ experiences of acute oncology services. All priorities relating to prevention, screening, and early diagnosis (seven items) and dissemination and implementation (one item) gained consensus. This was in marked contrast to themes related to symptoms and side effects and service models; few research priorities within these achieved consensus (27% and 18%, respectively).
Nurses and patients agreed that factors affecting patients’ early presentation with cancer symptoms (97%), followed by factors affecting early diagnosis of cancer (93%), were top research priorities. The availability of psychosocial support services across the cancer trajectory, particularly recurrence, was a priority (93%), as was management of anxiety and uncertainty following cancer treatment (93%). The role of primary care in managing post-treatment side effects and concerns was also listed as a priority (93%), along with priorities related to family-centered care, notably how to help parents with cancer to support their children (93%) and factors influencing cancer survivors’ integration back into family life following cancer and its treatment (90%).
[[{"type":"media","view_mode":"media_original","fid":"30171","attributes":{"alt":"","class":"media-image","height":"942","typeof":"foaf:Image","width":"674"}}]]
[[{"type":"media","view_mode":"media_original","fid":"30176","attributes":{"alt":"","class":"media-image","height":"944","typeof":"foaf:Image","width":"677"}}]]
[[{"type":"media","view_mode":"media_original","fid":"30181","attributes":{"alt":"","class":"media-image","height":"942","typeof":"foaf:Image","width":"676"}}]]
[[{"type":"media","view_mode":"media_original","fid":"30186","attributes":{"alt":"","class":"media-image","height":"447","typeof":"foaf:Image","width":"760"}}]]
Consensus Among Nurse Participants
Top priorities for research reaching high consensus within the body of nurse participants include factors affecting patients’ early presentation with cancer symptoms (95%); factors affecting early diagnosis of cancer (93%); availability of psychological support services across the cancer trajectory, particularly recurrence (93%); management of anxiety and uncertainty following cancer treatment (93%); ways to evidence the cost effectiveness of clinical nurse specialists (93%); and factors influencing cancer survivors’ integration back into family life following cancer and its treatment (93%). The use of eHealth and technology to manage symptoms at home was identified as a top priority by nurses (91%) but not by patients (72%).
Consensus Among Patient Participants
The top priorities for research among patient participants reflect four priorities related to palliative and end-of-life care that were not scored as top priorities for nurses: prognostication and timing of referral to palliative care (100% agreement by patients and 71% agreement by nurses); models of end-of-life care in the community (100% agreement by patients and 67% agreement by nurses), access to specialist and palliative care services at the end of life (100% agreement by patients and 69% agreement by nurses), and integration of palliative care within oncology services (94% agreement by patients and 74% agreement by nurses).
Other top research priorities identified by patient participants that did not reach high consenus within the body of nurse participants include benefits versus risks of adjuvant treatment in patients with moderate risk of recurrence (100% agreement by patients and 79% agreement by nurses); cognitive changes associated with cancer treatment recurrence (100% agreement by patients and 79% agreement by nurses); when and how palliative care services are introduced (100% agreement by patients and 76% agreement by nurses); and patient experience and quality of life across the cancer pathway (100% agreement by patients and 79% agreement by nurses).
Discussion
Corner et al. (2007) questioned who should be at the table when decisions are made about expenditures for future cancer research. The current authors’ research strongly supports the imperative for patients’ presence during such decision making. In addition, this work suggests that, when undertaking a Delphi survey, patients should be included throughout the process—not merely drawn on to validate priorities previously identified by health professionals. Had nurses in this study identified priorities that patients solely validated later, seven items that reached consensus would have been omitted. These seven items related to symptoms and side effects (n = 2), survivorship and rehabilitation (n = 2), service models (n = 2), and communication (n = 1).
Some of the top priorities for oncology nursing research identified in this study have been previously noted. Prevention, screening, and early diagnosis of cancer have been prioritized by Oncology Nursing Society members (LoBiondo-Wood et al., 2014), U.S. oncology nurses (Ropka et al., 2002), people living with cancer in the United Kingdom (Corner et al., 2007), and U.K. oncology nurses (Grundy & Ghazi, 2009). Likewise, the need for research into optimal management of patients’ psychological responses to cancer and its treatment has been stressed before in consensus-building exercises in the United Kingdom, Norway, the United States, and across Europe (Browne et al., 2002; Corner et al., 2007; Ropka et al., 2002; Rustøen & Schjølberg, 2000). That some of these areas had been identified years ago and remain a priority in the present day could reflect the research community’s lack of responsiveness to prioritization exercises, poor implementation of research findings in practice, or challenges encountered by cancer services in meeting the needs of the public and patients.
Although research into cancer screening and early diagnosis may have been neglected in the early 2000s, this is not the case now. In the United Kingdom, Cancer Research U.K. has funded a program of research into early diagnosis through its National Awareness and Early Diagnosis Initiative. Likewise, in the United States, a parallel program of research has been funded by the National Institutes of Health through its Early Detection Research Network. Knowledge of these initiatives could have raised professional and public understanding of the importance of research in these areas and prompted participants in this study to voice support for its continuance.
Conversely, psychological responses to cancer have been the target of psychosocial research for decades (Galway et al., 2012). Consequently, that research in psychosocial care remains of such high priority is, to some extent, surprising, begging the question of how well research evidence in this field is being implemented in practice, or whether patients have timely access to psychological support services according to need across the cancer pathway.
The results of this Delphi survey suggest that a change in focus is needed regarding research into symptom management. In addition to more traditionally researched symptoms such as pain, cognitive changes and neuropathy were also recognized as requiring prioritization. This may reflect that management of other symptoms has been sufficiently invested in. These results support a previous priority-setting exercise in which oncology nurses identified neuropathy and cognitive impairment as two of the five most difficult symptoms to manage, and neuropathy as one of the most distressing symptoms for patients (LoBiondo-Wood et al., 2014).
Novel priorities arising from the current authors’ research and not emphasized in previous consensus-building exercises include the need for research to help patients with cancer support their children, clarify what services patients would like from nurse specialists, and identify cancer therapies with identical benefit but lower side effect profiles. The effect of cancer on the entire family is increasingly recognized and reflected in publications addressing the needs of family caregivers (Waldron, Janke, Bechtel, Ramirez, & Cohen, 2013). However, little of this research has focused on the needs of children, despite recognition that, without intervention, cancer treatment and/or the death of a parent can have lifelong consequences for children (Ellis, Dowrick, & Lloyd-Williams, 2013). Consequently, this being a research priority for oncology nursing would be entirely appropriate.
Articulation of the role provided by and the cost effectiveness of clinical nurse specialists is another research priority that has not been highlighted before. That it has now been identified, in a time of austerity, is not of particular surprise. Clinical nurse specialists’ contribution tends to come under scrutiny when healthcare resources are scarce (Tarrant, Sinfield, Agarwal, & Baker, 2008).
Participants in this study are likely aware of new treatments (surgical and pharmaceutical) that are available. These open up the possibility for differing and more personalized treatments that can potentially enhance outcome while minimizing side effects. This may explain the expert panel’s prioritization of research into therapies with equivocal outcome yet reduced side effect profiles.
In this study, patients (unlike nurses) placed particular emphasis on the need for research into the interface between cancer and palliative care services, with 4 of patients’ top 12 priorities achieving 100% consensus relating to when and how palliative care services are introduced, prognostication and timing of referral to palliative care, access to specialist and palliative care services at the end of life, and models of end-of-life care in the community that integrate health and social care. This indicates that patients believe improvements are possible regarding how and when palliative care services are introduced. Nurses may not have emphasized palliative care in the same way because the exercise aimed to prioritize research areas for oncology rather than palliative care nursing.
In contrast to patients, nurses reached consensus on the need for research to highlight the role of eHealth and technology in remote symptom monitoring. Nurses may have emphasized this area knowing that technology will increasingly be used to promote health across the lifespan and to enable supported self-management during treatment for cancer. This is an area that patients may be unaware of. However, this may change as people integrate technology more into everyday life.
Limitations
While the current study was strengthened by having contributions from nurses and patients and a high response rate across the survey rounds (88%–97%), its limitations must be acknowledged. Although patients participated in the Delphi survey, fewer did so than nurses (18 versus 50, respectively). In addition, these patients, like the nurse participants, mostly identified as being White. Undoubtedly, the views of people from Black, Asian, and minority ethnic groups are underrepresented, and these populations may have priorities that differ from those presented. Future consensus-seeking exercises should aim to purposively sample people from Black, Asian, and minority ethnic minority groups who are living with cancer or who are providing care to them. Sufficient time should be built into the research process to ensure that these groups (the members of which may take more time to recruit) are reached. The importance of recruiting a diverse sample, including those from minority groups, should be emphasized when approaching eligible participants; this may help engagement with, and participation in, the research. The views of family members of people with cancer were not sought in this study and so are omitted. Because cancer is a family issue, their views are important to consider.
Implications for Nursing
This study demonstrates that people living with cancer provide a valuable contribution to informing research agendas for oncology nursing and should have a voice in future priority setting. Within this study, patient experts indicated a greater consensus for issues regarding palliative and end-of-life care than nurse experts. The importance of timely referral to palliative care, models of end-of-life care that integrate health and social care, and access to specialist palliative care services at the end of life were unanimously considered to be important future research priorities by patient experts.
This Delphi survey also highlighted the importance of preparing nurses to support cancer survivors’ engagement with evolving models of supportive care services, which may increasingly be delivered in the community or via remote services. A potential increase in eHealth interventions within cancer supportive care will have implications in terms of the training needs of the oncology nursing workforce; this warrants consideration.
Further implications of this research study are that cross-disciplinary work between oncology nurses and pediatric nurses should be encouraged to facilitate better support for the children of parents with cancer. Symptoms that have not previously been focused on in research, such as neuropathy, also require greater consideration.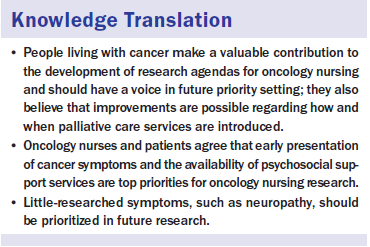
Conclusion
This consensus-building exercise demonstrates that nurses and patients support dedication of continued research resources to investigate issues around early presentation and diagnosis of cancer. As Corner et al. (2007) explained, many patients opine that “prevention is better than cure” (p. 878). The current authors’ research would also support an examination into the interface between cancer and palliative care, the role of primary care in cancer service provision, family-based services, optimal services for patients’ rehabilitation and psychological well-being as they live with and beyond a cancer diagnosis, and the role of eHealth and technology in supported self-management.
The authors gratefully acknowledge the Delphi panel members who gave generously of their expertise and time to reach consensus regarding research priorities of U.K. nurses and patients.
About the Author(s)
Cox is a research fellow, Arber is a senior lecturer, and Gallagher is a professor, all in the School of Health Sciences and Faculty of Health and Medical Sciences at the University of Surrey in Guildford; MacKenzie is an independent patient advocate in Bookham, Surrey; and Ream is a professor and director of research in the School of Health Sciences and Faculty of Health and Medical Sciences at the University of Surrey, all in the United Kingdom. This research was funded by the United Kingdom Oncology Nursing Society. Cox, Arber, Gallagher, and Ream contributed to the conceptualization and design and provided the analysis. Cox and Ream completed the data collection. Cox provided statistical support. All of the authors contributed to the manuscript preparation. Cox can be reached at a.cox@surrey.ac.uk, with copy to editor at ONFEditor@ons.org. Submitted June 2016. Accepted for publication July 18, 2016.

