Navigating the Transition From Cancer Care to Primary Care: Assistance of a Survivorship Care Plan
Purpose/Objectives: To examine symptom and quality-of-life (QOL) trajectories in breast cancer and lymphoma survivors enrolled in a survivorship navigation intervention and to explore patient, caregiver, and primary care provider (PCP) satisfaction with receipt of a survivorship care plan (SCP).
Design: Prospective, cohort, longitudinal.
Setting: The Billings Clinic, an integrated cancer center in Montana.
Sample: 67 patients with breast cancer or lymphoma who recently completed cancer treatment, along with 39 of their caregivers and 23 PCPs.
Methods: Data collection at one, three, and six months by the Functional Assessment of Cancer Therapy–General and satisfaction surveys.
Main Research Variables: Symptoms, QOL, and satisfaction with the survivorship navigator and the SCP.
Findings: Symptoms persisted six months following treatment. Symptoms and QOL indicators with worst intensity were energy, sleep, coping, and satisfaction with sex life. Patients with more comorbidities reported worse QOL, telephoned the survivorship navigator more often, and were more satisfied with the SCP. Patients with lymphoma reported higher QOL, but it was not significantly different from patients with breast cancer. Patients were significantly more satisfied than caregivers with the SCP at time 1. PCPs were highly satisfied with the SCP.
Conclusions: Some symptoms persist, even when cancer treatment has ended. Patients with comorbidities are at higher risk for more severe symptoms and worse QOL and may benefit from ongoing support. SCPs can facilitate patients’ transition to primary care following cancer treatment.
Implications for Nursing: Healthcare professionals who care for breast cancer survivors need to routinely assess them for the presence of comorbid conditions. Obese breast cancer survivors may benefit from weight reduction interventions to possibly decrease their risk of developing lymphedema and improve their overall health status.
Jump to a section
Cancer survival rates have been steadily improving during the past two decades. The overall risk of dying from cancer has decreased by 20% from 1991–2010 (Siegel, Ma, Zou, & Jemal, 2014), and the number of cancer survivors is expected to reach 18 million by 2020 (Mariotto, Yabroff, Shao, Feuer, & Brown, 2011). Cancer survivorship begins at diagnosis and continues throughout the patient’s life. Long-term physical and emotional symptoms and other sequelae often accompany cancer survivorship and require ongoing surveillance and management. Patients may be particularly vulnerable in the immediate post-initial treatment phase as they continue to experience side effects of cancer treatment and are transitioning back into primary care. Significant gaps are known to exist during the transition from cancer care to primary care, including lack of communication between the oncology and primary care teams and dearth of role clarity (Grunfeld & Earle, 2010); as a result, programs that bridge the gaps during these care transitions are needed (Hudson et al., 2012).
Background
In the report From Cancer Patient to Cancer Survivor: Lost in Transition, the Institute of Medicine (IOM) suggested that patients completing cancer treatment be given a summary of their cancer treatment and recommendations for follow-up care (Hewitt, Greenfield, & Stovall, 2006). A two-day IOM workshop convened following its publication to provide additional direction for cancer survivorship care planning implementation. The proceedings included discussion about care plan templates, implementation issues (e.g., reimbursement), and plans for testing survivorship models. Participants overwhelmingly indicated that research on patient-centered cancer treatment outcomes and the value of cancer treatment plans is essential (Hewitt & Ganz, 2007).
Since the release of From Cancer Patient to Cancer Survivor: Lost in Transition (Hewitt et al., 2006) and Implementing Cancer Survivorship Care Planning (Hewitt & Ganz, 2007), a plethora of studies have investigated concerns related to cancer survivorship, including which physical symptoms persist following initial cancer treatment (Brant et al., 2011; Burton, Fanciullo, Beasley, & Fisch, 2007; Stein, Syrjala, & Andrykowski, 2008), optimal survivorship models of care (Hahn & Ganz, 2011; Howell et al., 2012), and patient and provider preferences regarding survivorship plans (Kantsiper et al., 2009; Mayer, Gerstel, Leak, & Smith, 2012; Merport, Lemon, Nyambose, & Prout, 2012; Salz et al., 2012; Shalom, Hahn, Casillas, & Ganz, 2011; Watson, Sugden, & Rose, 2010). The use of cancer survivorship plans has been explored for patients with breast cancer (Hershman et al., 2013; Kantsiper et al., 2009; Smith, Singh-Carlson, Downie, Payeur, & Wai, 2011), gynecologic cancer (Brothers, Easley, Salani, & Andersen, 2013; Nicolaije et al., 2012), colorectal cancer, (Denlinger & Barsevick, 2009; Faul et al., 2012; Faul, Shibata, Townsend, & Jacobsen, 2010; Salz et al., 2012), head and neck cancer (Campbell, Massey, & Myers, 2012), and prostate cancer (Skolarus et al., 2013), among others. Despite the multitude of studies, questions remain regarding best models of survivorship care, patient and caregiver satisfaction with survivorship care planning, and the influence of survivorship care planning on patient outcomes (e.g., persistent symptoms, adherence to follow-up care, seamless transition back to primary care). A need exists to determine which models are most feasible, cost effective, and patient friendly, as well as which lead to sustainable outcomes. The Billings Clinic, a large integrated cancer center in Montana, used a survivorship navigator to prepare and deliver the survivorship care plan (SCP) and assist patients with the transition from cancer care back to primary care.
The purposes of this study were to (a) examine post-treatment symptom and quality-of-life (QOL) trajectories in breast cancer and lymphoma survivors enrolled in a survivorship navigation intervention and (b) explore patient, caregiver, and primary care provider (PCP) satisfaction with receipt of an SCP and treatment summary delivered by a survivorship navigator within three months following the end of initial cancer treatment.
Methods
Theoretical Framework
The dynamic symptom model was the organizing framework for this study (Brant, Beck, & Miaskowski, 2010). This model considers critical antecedents that can influence the symptom experience (e.g., age, gender, comorbidities, presence of a caregiver), symptom interventions and individuals to ameliorate or eliminate symptom severity (e.g., an SCP, survivorship navigator, PCP), longitudinal expression and analysis implications to model the dynamic nature of symptoms (i.e., symptoms measured at one, three, and six months for this study), and the consequences of uncontrolled symptoms over time (e.g., QOL).
Design
A prospective cohort intervention approach was used in this study, in which a survivorship navigator provided participants with a survivorship treatment summary and care plan following initial cancer treatment. Post-treatment symptoms were explored, along with patient, caregiver, and PCP satisfaction with the SCP.
Sample and Setting
A convenience sample was comprised of patients with lymphoma or breast cancer who recently completed chemotherapy at the Billings Clinic. Patients without a reliable translator who were unable to understand or speak English and those with significant cognitive deficits who were unable to understand or use the data collection tools and surveys were excluded from the study. Patients with breast cancer were chosen to take part in the study because a multidisciplinary breast team had recently completed foundational work in survivorship treatment summaries and care plans and was ready to move to comprehensive survivorship planning. Lymphoma survivors were also chosen because this cancer center is the primary referral site for hematologic malignancies, drawing patients from across the region. These diagnoses allowed inclusiveness of both genders and drew more older adult and rural cancer survivors into the study.
Procedure
Disease-specific navigation is the standard of care within the research setting where this study was conducted. Navigators meet with patients at diagnosis, schedule patient appointments, and provide patient education about the disease process and treatment plan. The breast cancer and hematology nurse navigators approached all patients with breast cancer or lymphoma who had recently completed initial cancer treatment to participate in the study. Those interested were contacted by the survivorship navigator, hired specifically for this study, who further explained the study and obtained informed consent. The survivorship navigator’s role included developing the SCP surveys, conducting the survivorship visit, following up with the PCP regarding the SCP, gathering follow-up data at three and six months, and answering telephone calls from the patients enrolled in the study about persistent symptoms and survivorship concerns. Caregivers who accompanied patients to the survivorship visit and primary caregivers also consented to participate in the study. After receiving consent, the survivorship navigator prepared an SCP and treatment summary for each patient, reviewed each plan with the patient’s medical oncologist, and met individually with each patient and caregiver within the first month following completion of active treatment to deliver and discuss the treatment summary and SCP, prepared as a paper brochure. Patients were also given the direct telephone number of the survivorship navigator and were encouraged to call with questions or concerns about persistent symptoms.
Symptoms were assessed at one, three, and six months following cancer treatment through a mailed survey. Satisfaction surveys were mailed to patients within one week of the initial survivorship navigator visit (time 1) and six months later (time 2). Primary caregivers received a satisfaction survey at these same times. Treatment summaries and SCPs were also mailed to each survivor’s PCP, along with a satisfaction survey to garner provider feedback and satisfaction with the SCP. The survivorship navigator telephoned patients, caregivers, and PCPs to remind them to return surveys, as needed. Outcomes included symptom amelioration during the six-month post-treatment trajectory and patient, caregiver, and PCP satisfaction with the SCP.
Instruments
Version 4 of the Functional Assessment of Cancer Therapy–General (FACT-G) was used to assess symptoms at one, three, and six months following delivery of the SCP. The 27-item, self-report QOL measure consists of four subscales: physical, emotional, functional, and social/familial well-being. Items are rated on a five-point Likert scale ranging from 0 (not at all) to 4 (very much). Total scores range from 0–28, with higher scores indicating better QOL. The FACT-G reports well-established validity and reliability (Cronbach alpha of 0.89) for the entire scale and subscales (Cronbach alpha of 0.65–0.82). Test-retest reliability is reported at 0.82–0.92 (Cella et al., 1993). Subsequent use of updated versions, including version 4, have continued to support the instrument’s reliability (Victorson, Barocas, Song, & Cella, 2008).
SCPs were developed by an interdisciplinary team at the cancer center based on the 10 IOM recommendations (Hewitt et al., 2006; Hewitt & Ganz, 2007) and disease-specific templates from the American Society of Clinical Oncology (2016) and the National Comprehensive Cancer Network (2016). Plans were prefaced by an individualized treatment summary and prepared as a paper brochure for each patient.
At the time of this study, a lack of satisfaction surveys existed to evaluate SCPs. Investigators who had previous experience in item writing and survey development drew from scaling and content of past surveys in creating a new survey for the purposes of this study. Items were suggested and reviewed by the team of researchers. The patient, caregiver, and provider satisfaction surveys evaluated the usability and feasibility of, as well as overall satisfaction with, the SCP. Opinions were rated on a six-point Likert-type scale ranging from 1 (strongly disagree) to 6 (strongly agree). Eight items comprised each survey, including ease of understanding the plan, ability to better manage anxiety and symptoms because of the SCP, and ease of the transition of care between the regional cancer center and the PCP. Satisfaction for patients and caregivers was measured at one and six months and once for providers on receipt of the patient’s SCP. A tracking tool for patient telephone calls to the survivorship navigator captured patients’ incoming calls, the date and time of the call, reasons for the call, and actions taken in response to patient needs.
Data Analysis
Data were entered into SPSS®, version 22.0, by the research team. Analysis commenced according to each specific aim. One specific aim examined symptom trajectories reported by cancer survivors at one, three, and six months post-active treatment. Overall QOL and subscale domains of the FACT-G were explored through means, medians, modes, and standard deviations (SDs) at each point in time. Missing data on the FACT-G were scored according to criteria set by Fairclough and Cella (1996). Pearson correlations were used to measure the relationship between symptom severity and patient satisfaction rates with the survivorship plan.
Change over time in the FACT subscales and total score were analyzed in a repeated measures analysis of covariance model with time (three time points) as the only within-subjects variable and type of cancer (breast cancer versus lymphoma) as the sole between-subjects factor. The number of comorbidities (measured at each time point) was used as a covariate. The data were analyzed using the linear mixed model and the maximum likelihood estimation. One strength of this analytical method is that it is not biased by listwise deletion of missing data. In this model, all data were retained in the analyses (as opposed to losing power with an analysis that employs listwise deletion).
The second specific aim was to explore patient, caregiver, and PCP satisfaction with the newly developed SCPs. Descriptive statistics, including means, medians, modes, and SDs, were used to explore satisfaction scores.
Findings
Population Demographics
Sixty-seven cancer survivors participated in the study (see Table 1). Many of the patients lived in rural areas, and about half (n = 35) lived outside of the cancer center’s county. One patient traveled almost 400 miles to receive cancer care. In addition, 39 caregivers participated in the study. The majority (n = 30) were caregivers of patients with breast cancer. Thirty-three were spouses or partners, two were sons or daughters, and four were other relatives. Twenty-three PCPs who received SCPs provided feedback on their satisfaction with the SCP: 11 local physicians (MDs) from internal and family medicine, 10 MDs from rural areas, 1 doctor of osteopathic medicine, and 1 nurse practitioner. 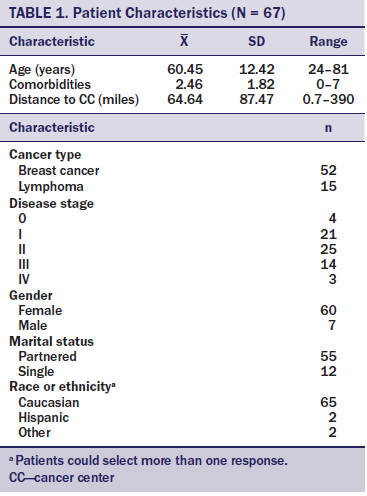
As is common in longitudinal studies, missing data existed. Although 67 patients were enrolled in the study, 18 patients with breast cancer and 7 patients with lymphoma were missing at least one time point. Overall, 25 patients were missing data from at least one time point. The current authors examined predictors of missing information and found that missing information was not statistically related to cancer type, age, comorbidities, or marital status. Consequently, the data are classified as missing at random (Little & Rubin, 2002). The utility of various covariates in the model was also explored, with the result being that the only covariate of statistical importance was the number of comorbidities.
Symptom Experiences
All well-being subscales of the FACT-G were significantly different than zero (intercept p < 0.0001), indicating physical, social, psychological, and functional morbidity throughout cancer treatment. The patterns of change for all four subscales of the FACT-G over time were relatively flat, suggesting no significant change over time but symptom persistence. Differences between cancer type (breast cancer versus lymphoma), change over time, and the cancer type by time interaction were examined using a series of linear mixed model analyses. In these models, the current authors examined the main effect of cancer type, time, and the cancer type by time interaction. Few significant main effects and no interaction effects were found. However, significant differences existed between cancer types regarding social well-being (p = 0.04). Patients with lymphoma showed higher social functioning than did patients with breast cancer. The trajectories over time were relatively flat, and this stability over time was confirmed by the analyses. The only subscale that showed a trend to significant change was physical well-being (p = 0.06). A small increase in physical functioning occurred over time. In some cases, such as physical well-being, the figures seem to indicate that trajectories of change were different between breast cancer and lymphoma; however, in no case were statistically significant interactions found (all p values were greater than 0.3).
Some morbidity in well-being persisted but did not significantly improve over time. Patients with lymphoma reported better physical, functional, and emotional well-being and overall QOL, but the differences were not significant. Modest differences were observed in cancer type and social QOL (p = 0.04), with patients with lymphoma reporting significantly higher social wellness than those with breast cancer. This result should be taken with caution; it is the sole main effect within a context of no differences in time, cancer type, or the interaction effect. Patients with more comorbidities (p = 0.01) also had poorer functioning and significantly worse QOL (p = 0.01).
Some significant changes were noted in individual symptoms over time. Patients with breast cancer complained of experiencing worse nausea and feeling more ill at six months compared to one month (p = 0.015; p = 0.019). Patients with lymphoma felt better able to physically meet the needs of their families between one and six months (p = 0.016). Socially, patients with breast cancer felt less close to friends between one month and three months (p = 0.036), whereas patients with lymphoma reported improvement with this item (p = 0.017). However, patients with lymphoma were less satisfied with their sex life at three months compared to one month (p = 0.031). Emotionally, patients with lymphoma reported they coped worse with their illness between three and six months (p = 0.041). Both groups demonstrated changes in nervousness, with patients with breast cancer improving initially (baseline to three months; p = 0.009) and then becoming more nervous at six months (p = 0.035); patients with lymphoma reported less nervousness between three and six months (p = 0.036). Symptoms rated the lowest on each subscale were energy (physical), sex life (social), satisfaction with illness coping ability (emotional), and sleep (functional) (see Figure 1). Unlike a traditional repeated measures analysis of variance (ANOVA), the linear mixed model does not produce effect size metrics as an option (and the computation of R2s as effect sizes can be problematic) (Snijders & Bosker, 2012). Consequently, the current authors have taken a hybrid approach and run the analyses in a traditional model and reported the partial eta squares. The authors recognize that these effect sizes are downwardly biased because the traditional ANOVA is underpowered, a result of missing data. 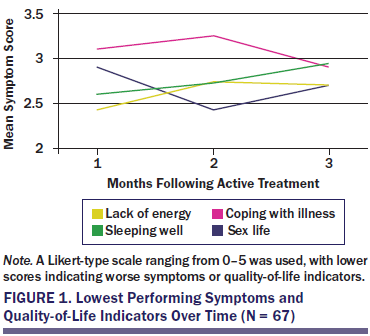
Twenty patients called the survivorship navigator within the first three months following delivery of the SCP (range = 1–5 calls). Only one patient called between three and six months. A positive correlation was noted in navigator calls and number of physical symptoms (r = –0.26, p = 0.05), emotional symptoms (r = –0.26, p = 0.04), poorer functioning (r = –0.27, p = 0.04), and overall poorer QOL (r = –0.27, p = 0.04).
Survivorship Care Plan Satisfaction
Patients: The majority of patients (n = 49) strongly agreed that they were satisfied with the SCP. Most thought it was easy to understand and that the survivorship navigator adequately answered questions about the plan. The SCP helped most patients to feel less anxious initially, but this declined at six months. Slight agreement was noted when patients were asked if they discussed the SCP with their PCP. At first, most patients perceived that their PCP was better able to manage their needs with the SCP, but this declined at six months. Satisfaction scores are included in Table 2. 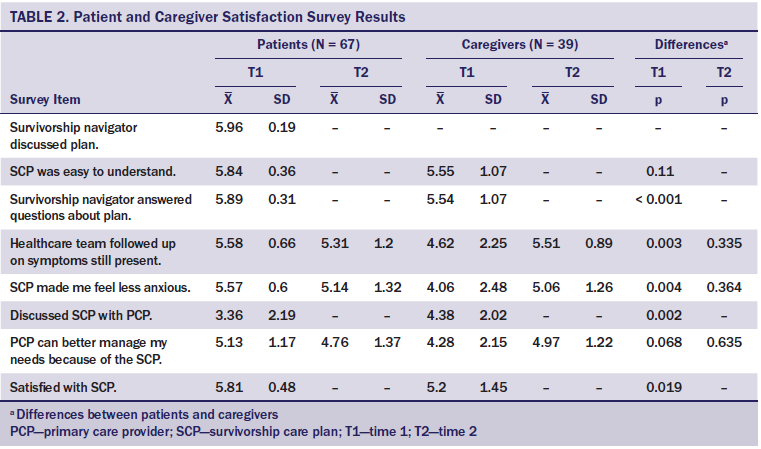
The item “I discussed my survivorship care plan with my primary care provider” was modestly correlated in patients who had the highest number of comorbidities (r = 0.323, p = 0.03). A modest relationship also existed in patients with comorbidities and their perception that their PCP can better manage their needs because of the SCP (r = 0.293, p = 0.03).
Patients also provided open-ended responses at the end of their surveys. All responses were positive. Comments from patients included the following: “I want you to know how reassuring it is to be recognized, supported, and facilitated” and “Great to have this kind of follow-up support and to have critical information all in one place and portable.” Another explained the usefulness of the SCP in detail.
It was the best care I have received. This booklet will be great. If I have to travel, everything needed is in it. This, to me, was a great idea. Following us as we move on in life, especially right after our active treatment, is important. We aren’t left out, not knowing a direction. This will help us ease back to somewhat normal. Thank you!
Caregivers: Caregivers were significantly less satisfied overall with the SCP compared to patients (p = 0.019) at time 1. Most caregivers slightly agreed at time 1 that the SCP made them feel less anxious initially, but this was significantly different from the patients who perceived even less initial anxiety thanks to receipt of the SCP (p = 0.004). At six months, caregiver perceptions about anxiety resembled patients’ perceptions. Caregivers slightly to moderately agreed that the PCP was better able to manage their significant other’s needs initially, and more caregivers strongly agreed by six months.
Primary care providers: The majority of PCPs strongly agreed with the statement “I am satisfied with the cancer survivorship plan and treatment summary” (n = 13, mean = 5.3). Most felt it was adequately described (mean = 5.39), was easy to understand (mean = 5.26), was comprehensive (mean = 5.61), was helpful in providing optimal care (mean = 5.41), and provided direction for cancer follow-up (mean = 5.48). Thirteen strongly agreed that they would follow the SCP, seven moderately agreed, one slightly agreed, and one slightly disagreed (mean = 5.45).
Survivorship care plan and symptom relationships: Significant negative correlations existed between satisfaction with the SCP and anxiety at one month (r = 0.3, p = 0.03) and higher emotional QOL (r = 0.43, p = 0.002). Perception that the SCP would improve care with the PCP was also significantly correlated with the following three variables: emotional QOL at three months (r = 0.32, p = 0.013), emotional QOL at six months (r = 0.58, p < 0.0001), and higher overall QOL at six months (r = 0.412, p = 0.009)
Discussion
The findings from this study suggest that symptoms persist in patients with breast cancer and lymphoma, even six months following the completion of cancer treatment. This is consistent with other studies and systematic reviews (Kenyon, Mayer, & Owens, 2014). Unsurprisingly, the physical symptoms with the worst severity were energy and sleep. A prevalence study on fatigue in cancer survivors indicated that 29% (n = 150) of 515 patients had moderate to severe fatigue (Wang et al., 2014). One study of 464 breast cancer survivors found that fatigue was a major problem as many as six months after treatment and prevented women from being active (Charlier et al., 2012). Sleep disturbance was also found to be significant in breast cancer survivors in a systematic review of 12 studies (Budhrani, Lengacher, Kip, Tofthagen, & Jim, 2015). One study of 68 women with breast cancer found that fatigue and sleep returned to baseline one year after treatment, but both were still worse in these patients than in a comparison group of individuals without cancer (Ancoli-Israel et al., 2014). Fatigue and sleep disturbance are also documented in adult lymphoma survivors post-treatment (Brant et al., 2011), but the majority of reports are in childhood survivors (Zeller et al., 2014).
Coping was the lowest rated emotional symptom. Coping decreased between three and six months, and nervousness improved at three months but worsened at six months. Women with breast cancer also reported being less close to friends at baseline compared to three months. Brant et al. (2011) found that anxiety and depression improved in men with lung or colorectal cancer or lymphoma following treatment but then worsened. A “honeymoon effect” may occur directly after treatment; however, experiencing a fear of recurrence and living with persistent symptoms becomes a reality for patients, and coping and nervousness may worsen.
Satisfaction with sex life was rated lowest in the social domain. Sexual satisfaction is often ignored, and this finding reinforces the need to discuss changes in sex life with the patient and his or her significant other. Often, strategies including sexual therapy can be employed to enhance sexual QOL.
One positive finding is that patients with more comorbidities and higher symptom burden were more likely to telephone the survivorship navigator. Those patients who likely required symptom management interventions actually reached out for support, suggesting that patients who have other chronic illnesses and who experience more symptom burden may benefit more from access to a survivorship navigator and receipt of an SCP. Having an identified person to contact for symptom management in the post-survivorship period (survivorship navigator) may have encouraged patients in this direction. The use of a survivorship navigator resonates with a report by Jefford et al. (2013), explaining that traditional survivorship care focused on disease recurrence; however, moving forward, survivorship care must include rapid access to care, as well as information and education to enable confidence in self-management after treatment. A survivorship navigator provides just that.
To the current authors’ knowledge, this study is the first to evaluate caregiver satisfaction with the SCP, which is significant because caregivers are often involved in survivorship care of their significant other. Overall, high satisfaction existed with receipt of the SCP for patients and caregivers. This finding is consistent with other studies reporting that SCPs are well received (Mayer, Gerstel, et al., 2014; Rosales et al., 2014; Sprague et al., 2013). In the current study, compared to caregivers, patients were significantly more satisfied with the SCP and more strongly agreed with their PCP’s ability to better manage their needs because of the SCP. A study by Kantsiper et al. (2009) reported that survivors believed PCPs lacked the necessary expertise to provide survivorship care. Having an SCP to discuss follow-up care may lessen this fear, and the current study suggests that an SCP may help patients to feel more confident about their PCP’s ability to provide survivorship care.
Receipt of the SCP also made patients feel less anxious. Although this was also true for caregivers, the perception was greater among patients, particularly initially. However, a systematic review of five randomized, controlled trials found a lack of difference in care satisfaction, cancer care coordination, or oncological outcomes between those who received an SCP and those who did not (Brennan, Gormally, Butow, Boyle, & Spillane, 2014). One study within the systematic review suggested that the SCP reduced unmet needs; overall levels of survivor satisfaction with the SCP were very high. Grunfeld et al. (2011) evaluated distress in women with early-stage breast cancer who were randomized to receive an SCP or standard care and found no differences in distress between groups. Patients did report feeling less anxious because of the SCP in this study, but lack of a control group limits these findings (Grunfeld et al., 2011).
PCPs were also highly satisfied with the SCP. These results are mixed in previous studies. One study reported that only 40% of PCPs surveyed felt that a cancer care review, which is similar to an SCP, was useful in providing care (Watson et al., 2010). Intent to use the SCP was also high in the current study; most strongly or moderately agreed that they will follow the SCP. A previous study by Nissen et al. (2007) reported that only 52% of PCPs were comfortable with providing cancer surveillance and only 43% were confident in following standard guidelines for survivorship care. The SCP may allow PCPs to more comfortably provide cancer surveillance and follow-up care. This is an important finding because PCPs assume the sole care of patients following cancer treatment, particularly in rural areas. In the regional cancer center used in this study, more than half of the 1,500 patients seen annually live outside of the metropolitan area. About 8% of patients receiving cancer care services are Native Americans, many living on one of Montana’s seven Indian reservations. In addition to significant travel distances for treatment (as many as 400 miles each way), these survivors face unique community living and cultural challenges when returning to their respective communities. Because patients may continue to experience physical and/or psychosocial distress after the end of active treatment, the barriers of distance, lack of services in rural areas, and community cultural norms pose real constraints to optimal cancer survivorship for these groups. Although intent to use the SCP was high, additional studies should be employed that measure actual use of the SCP and whether this use leads to positive patient outcomes.
Limitations
A summative evaluation of SCP studies noted that only four randomized, controlled trials in this area of research exist and that this area of research is limited by lack of randomized, controlled trials overall, of sample diversity, and of standardized data collection tools (Mayer, Birken, Check, & Chen, 2014). The current study notes those same limitations. Additional limitations, such as the small convenience sample, the small number of patients with lymphoma compared to patients with breast cancer, the single site, the significant amount of missing data, and the lack of a control group limit the overall findings. The satisfaction tools were also not previously tested. Missing symptom data are also acknowledged across the six-month post-treatment trajectory.
These limitations provide direction for future research. Randomized, controlled trials should be conducted regarding the timing of delivery of the SCP, who should deliver the SCP, and how the SCP can best support patients across the survivorship trajectory. Most importantly, survivorship care does not simply involve surveillance but rather ongoing management of symptoms along the continuum. Models that support symptom management during the transition to primary care should be examined. Partnerships between the PCP and the cancer care team may be important to evaluate. Ongoing work should investigate how these plans can improve not only surveillance and the transition to primary care but also how they may improve symptoms and overall QOL.
Implications for Practice
Symptoms persist beyond cancer treatment, and coping with persistent symptoms and a cancer diagnosis post-treatment can be difficult. In the current study, patients with greater symptom burden and more comorbidities contacted the survivorship navigator more frequently, implying the importance of having a designated nurse available to respond to calls and concerns about survivorship. This could be a RN navigator or another clinical nurse within the practice. Calls dropped between three and six months, yet coping decreased. Therefore, having nurses make follow-up calls to patients after treatment to assess the transition of active treatment to survivorship, rather than waiting for the patient to call in, may be important. Nurse-led survivorship classes could also be offered to facilitate this sometimes difficult transition.
In addition, this study highlights the relationship of patients and caregivers as a team, with individual perceptions about care. Because caregiver satisfaction was lower in this study, nurses should be reminded to include the caregiver in conversations about symptoms and follow-up, with patient permission, and ask for feedback and questions from patients and their caregivers. 
Conclusion
Overall, nurses should be reminded that the SCP is an important document that can facilitate a patient’s transition to primary care, but optimal use of the SCP is highly dependent on open communication among the oncology and primary care teams, the patient, and the caregiver. Often, the nurse is the facilitator of this transition and can help to ensure seamless care delivery following cancer treatment.
References
American Society of Clinical Oncology. (2016). ASCO cancer treatment and survivorship care plans. Retrieved from http://www.cancer.net/survivorship/follow-care-after-cancer-treatment/a…
Ancoli-Israel, S., Liu, L., Rissling, M., Natarajan, L., Neikrug, A.B., Palmer, B.W., . . . Maglione, J. (2014). Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: A 1-year longitudinal study. Supportive Care in Cancer, 22, 2535–2545. doi:10.1007/s00520-014-2204-5
Brant, J.M., Beck, S., Dudley, W.N., Cobb, P., Pepper, G., & Miaskowski, C. (2011). Symptom trajectories in posttreatment cancer survivors. Cancer Nursing, 34, 67–77. doi:10.1097/NCC.0b013e3181f04ae9
Brant, J.M., Beck, S., & Miaskowski, C. (2010). Building dynamic models and theories to advance the science of symptom management research. Journal of Advanced Nursing, 66, 228–240. doi:10.1111/j.1365-2648.2009.05179.x
Brennan, M.E., Gormally, J.F., Butow, P., Boyle, F.M., & Spillane, A.J. (2014). Survivorship care plans in cancer: A systematic review of care plan outcomes. British Journal of Cancer, 111, 1899–1908. doi:10.1038/bjc.2014.505
Brothers, B.M., Easley, A., Salani, R., & Andersen, B.L. (2013). Do survivorship care plans impact patients’ evaluations of care? A randomized evaluation with gynecologic oncology patients. Gynecologic Oncology, 129, 554–558. doi:10.1016/j.ygyno.2013.02.037
Budhrani, P.H., Lengacher, C.A., Kip, K., Tofthagen, C., & Jim, H. (2015). An integrative review of subjective and objective measures of sleep disturbances in breast cancer survivors. Clinical Journal of Oncology Nursing, 19, 185–191. doi:10.1188/15.CJON.185-191
Burton, A.W., Fanciullo, G.J., Beasley, R.D., & Fisch, M.J. (2007). Chronic pain in the cancer survivor: A new frontier. Pain Medicine, 8, 189–198. doi:10.1111/j.1526-4637.2006.00220.x
Campbell, B.H., Massey, B.L., & Myers, K.B. (2012). Survivorship care plans for patients with head and neck cancer. Archives of Otolaryngology—Head and Neck Surgery, 138, 1116–1119. doi:10.1001/jamaoto.2013.683
Cella, D.F., Tulsky, D.S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., . . . Harris, J. (1993). The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 570–579.
Charlier, C., Van Hoof, E., Pauwels, E., Lechner, L., Spittaels, H., Bourgois, J., & De Bourdeaudhuij, I. (2012). Treatment-related and psychosocial variables in explaining physical activity in women three weeks to six months post-treatment of breast cancer. Patient Education and Counseling, 89, 171–177. doi:10.1016/j.pec.2012.06.029
Denlinger, C.S., & Barsevick, A.M. (2009). The challenges of colorectal cancer survivorship. Journal of the National Comprehensive Cancer Network, 7, 883–893.
Fairclough, D.L., & Cella, D.F. (1996). Functional Assessment of Cancer Therapy (FACT-G): Non-response to individual questions. Quality of Life Research, 5, 321–329.
Faul, L.A., Rivers, B., Shibata, D., Townsend, I., Cabrera, P., Quinn, G.P., & Jacobsen, P.B. (2012). Survivorship care planning in colorectal cancer: Feedback from survivors and providers. Journal of Psychosocial Oncology, 30, 198–216. doi:10.1080/07347332.2011.651260
Faul, L.A., Shibata, D., Townsend, I., & Jacobsen, P.B. (2010). Improving survivorship care for patients with colorectal cancer. Cancer Control, 17, 35–43.
Grunfeld, E., & Earle, C.C. (2010). The interface between primary and oncology specialty care: Treatment through survivorship. Journal of the National Cancer Institute. Monographs, 2010, 25–30. doi:10.1093/jncimonographs/lgq002
Grunfeld, E., Julian, J.A., Pond, G., Maunsell, E., Coyle, D., Folkes, A., . . . Levine, M.N. (2011). Evaluating survivorship care plans: Results of a randomized, clinical trial of patients with breast cancer. Journal of Clinical Oncology, 29, 4755–4762. doi:10.1200/JCO.2011.36.8373
Hahn, E.E., & Ganz, P.A. (2011). Survivorship programs and care plans in practice: Variations on a theme. Journal of Oncology Practice, 7, 70–75. doi:10.1200/jop.2010.000115
Hershman, D.L., Greenlee, H., Awad, D., Kalinsky, K., Maurer, M., Kranwinkel, G., . . . Crew, K.D. (2013). Randomized controlled trial of a clinic-based survivorship intervention following adjuvant therapy in breast cancer survivors. Breast Cancer Research and Treatment, 138, 795–806. doi:10.1007/s10549-013-2486-1
Hewitt, M., & Ganz, P.A. (2007). Implementing cancer survivorship care planning. Washington, DC: National Academies Press.
Hewitt, M., Greenfield, S., & Stovall, E. (Eds). (2006). From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press.
Howell, D., Hack, T.F., Oliver, T.K., Chulak, T., Mayo, S., Aubin, M., . . . Sinclair, S. (2012). Models of care for post-treatment follow-up of adult cancer survivors: A systematic review and quality appraisal of the evidence. Journal of Cancer Survivorship, 6, 359–371. doi:10.1007/s11764-012-0232-z
Hudson, S.V., Miller, S.M., Hemler, J., McClinton, A., Oeffinger, K.C., Tallia, A., & Crabtree, B.F. (2012). Cancer survivors and the patient-centered medical home. Translational Behavioral Medicine, 2, 322–331. doi:10.1007/s13142-012-0138-3
Jefford, M., Rowland, J., Grunfeld, E., Richards, M., Maher, J., & Glaser, A. (2013). Implementing improved post-treatment care for cancer survivors in England, with reflections from Australia, Canada and the USA. British Journal of Cancer, 108, 14–20. doi:10.1038/bjc.2012.554
Kantsiper, M., McDonald, E.L., Geller, G., Shockney, L., Snyder, C., & Wolff, A.C. (2009). Transitioning to breast cancer survivorship: Perspectives of patients, cancer specialists, and primary care providers. Journal of General Internal Medicine, 24(Suppl. 2), S459–S466. doi:10.1007/s11606-009-1000-2
Kenyon, M., Mayer, D.K., & Owens, A.K. (2014). Late and long-term effects of breast cancer treatment and surveillance management for the general practitioner. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 43, 382–398. doi:10.1111/1552-6909.12300
Little, R.J.A., & Rubin, D.B. (2002). Statistical analysis with missing data (2nd ed.). New York, NY: John Wiley and Sons.
Mariotto, A.B., Yabroff, K.R., Shao, Y., Feuer, E.J., & Brown, M.L. (2011). Projections of the cost of cancer care in the United States: 2010–2020. Journal of the National Cancer Institute, 103, 117–128. doi:10.1093/jnci/djq495
Mayer, D.K., Birken, S.A., Check, D.K., & Chen, R.C. (2014). Summing it up: An integrative review of studies of cancer survivorship care plans (2006–2013). Cancer, 121, 978–996. doi:10.1002/cncr.28884
Mayer, D.K., Gerstel, A., Leak, A.N., & Smith, S.K. (2012). Patient and provider preferences for survivorship care plans. Journal of Oncology Practice, 8, e80–e86. doi:10.1200/jop.2011.000401
Mayer, D.K., Gerstel, A., Walton, A.L., Triglianos, T., Sadiq, T.E., Hawkins, N.A., & Davies, J.M. (2014). Implementing survivorship care plans for colon cancer survivors. Oncology Nursing Forum, 41, 266–273. doi:10.1188/14.ONF.266-273
Merport, A., Lemon, S.C., Nyambose, J., & Prout, M.N. (2012). The use of cancer treatment summaries and care plans among Massachusetts physicians. Supportive Care in Cancer, 20, 1579–1583. doi:10.1007/s00520-012-1458-z
National Comprehensive Cancer Network. (2016). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Survivorship [v.2.2016]. Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf
Nicolaije, K.A., Husson, O., Ezendam, N.P., Vos, M.C., Kruitwagen, R.F., Lybeert, M.L., & van de Poll-Franse, L.V. (2012). Endometrial cancer survivors are unsatisfied with received information about diagnosis, treatment and follow-up: A study from the population-based PROFILES registry. Patient Education and Counseling, 88, 427–435. doi:10.1016/j.pec.2012.05.002
Nissen, M.J., Beran, M.S., Lee, M.W., Mehta, S.R., Pine, D.A., & Swenson, K.K. (2007). Views of primary care providers on follow-up care of cancer patients. Family Medicine, 39, 477–482.
Rosales, A.R., Byrne, D., Burnham, C., Watts, L., Clifford, K., Zuckerman, D.S., & Beck, T. (2014). Comprehensive survivorship care with cost and revenue analysis. Journal of Oncology Practice, 10, e81–e85. doi:10.1200/jop.2013.000945
Salz, T., Oeffinger, K.C., Lewis, P.R., Williams, R.L., Rhyne, R.L., & Yeazel, M.W. (2012). Primary care providers’ needs and preferences for information about colorectal cancer survivorship care. Journal of the American Board of Family Medicine, 25, 635–651. doi:10.3122/jabfm.2012.05.120083
Shalom, M.M., Hahn, E.E., Casillas, J., & Ganz, P.A. (2011). Do survivorship care plans make a difference? A primary care provider perspective. Journal of Oncology Practice, 7, 314–318. doi:10.1200/jop.2010.000208
Siegel, R., Ma, J., Zou, Z., & Jemal, A. (2014). Cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 64, 9–29. doi:10.3322/caac.21208
Skolarus, T.A., Holmes-Rovner, M., Northouse, L.L., Fagerlin, A., Garlinghouse, C., Demers, R.Y., . . . Wei, J.T. (2013). Primary care perspectives on prostate cancer survivorship: Implications for improving quality of care. Urologic Oncology, 31, 727–732. doi:10.1016/j.urolonc.2011.06.002
Smith, S.L., Singh-Carlson, S., Downie, L., Payeur, N., & Wai, E.S. (2011). Survivors of breast cancer: Patient perspectives on survivorship care planning. Journal of Cancer Survivorship, 5, 337–344. doi:10.1007/s11764-011-0185-7
Snijders, T.A.B., & Bosker, R.J. (2012). Multilevel analysis: An introduction to basic and advanced multilevel modeling (2nd ed.). Thousand Oaks, CA: Sage.
Sprague, B.L., Dittus, K.L., Pace, C.M., Dulko, D., Pollack, L.A., Hawkins, N.A., & Geller, B.M. (2013). Patient satisfaction with breast and colorectal cancer survivorship care plans. Clinical Journal of Oncology Nursing, 17, 266–272. doi:10.1188/13.CJON.17-03AP
Stein, K.D., Syrjala, K.L., & Andrykowski, M.A. (2008). Physical and psychological long-term and late effects of cancer. Cancer, 112(Suppl. 11), 2577–2592. doi:10.1002/cncr.23448
Victorson, D., Barocas, J., Song, J., & Cella, D. (2008). Reliability across studies from the Functional Assessment of Cancer Therapy-General (FACT-G) and its subscales: A reliability generalization. Quality of Life Research, 17, 1137–1146. doi:10.1007/s11136-008-9398-2
Wang, X.S., Zhao, F., Fisch, M.J., O’Mara, A.M., Cella, D., Mendoza, T.R., & Cleeland, C.S. (2014). Prevalence and characteristics of moderate to severe fatigue: A multicenter study in cancer patients and survivors. Cancer, 120, 425–432. doi:10.1002/cncr.28434
Watson, E.K., Sugden, E.M., & Rose, P.W. (2010). Views of primary care physicians and oncologists on cancer follow-up initiatives in primary care: An online survey. Journal of Cancer Survivorship, 4, 159–166. doi:10.1007/s11764-010-0117-y
Zeller, B., Loge, J.H., Kanellopoulos, A., Hamre, H., Wyller, V.B., & Ruud, E. (2014). Chronic fatigue in long-term survivors of childhood lymphomas and leukemia: Persistence and associated clinical factors. Journal of Pediatric Hematology/Oncology, 36, 438–444. doi:10.1097/mph.0000000000000051
About the Author(s)
Brant is an oncology clinical nurse specialist and nurse scientist, Blaseg is director of cancer services, integrative medicine, and supportive care, Aders is a patient care navigator, and Oliver is a data analyst, all at the Billings Clinic in Montana; Gray is a customer services representative at CenterPoint Human Services in Winston-Salem, NC; and Dudley is a professor in the Department of Public Health Education at the University of North Carolina in Greensboro. No financial relationships to disclose. Brant and Blaseg contributed to the conceptualization and design. Aders and Oliver completed the data collection. Oliver, Gray, and Dudley provided statistical support. Brant and Dudley contributed to the analysis and manuscript preparation. Brant can be reached at jbrant@billingsclinic.org, with copy to editor at ONFEditor@ons.org. Submitted June 2015. Accepted for publication January 22, 2016.

