Prevalence, Risk Factors, and Levels of Burnout Among Oncology Nurses: A Systematic Review
Problem Identification: To determine (a) the average levels of emotional exhaustion (EE), depersonalization (D), and personal accomplishment (PA) among oncology nurses; (b) the prevalence of low, medium, and high levels of burnout for each dimension; and (c) the risk factors for burnout.
Literature Search: A systematic review was carried out using the CUIDEN, CINAHL®, LILACS, ProQuest, PubMed, SciELO, and Scopus databases.
Data Evaluation: The 436 search results obtained were reduced to a final sample of 27 articles after applying the inclusion and exclusion criteria.
Synthesis: With respect to levels of burnout, published results differ in their conclusions. In general, they indicate that oncology nurses feel little sense of PA and suffer from EE, although few signs of D exist.
Conclusions: Oncology nurses present high levels of EE and of reduced PA. A large proportion of these nurses are at risk of developing burnout. Age, work experience, workload, and communication skills are among the factors that may influence development of the syndrome.
Implications for Practice: Programs should be developed to identify interventions that would reduce EE and enhance feelings of PA. In addition, risk factors and protective measures should be studied more comprehensively.
Jump to a section
Healthcare work is characterized by the need to cope with complex situations arising from hospital settings in which treatment and care are provided to help people recover from disease. Healthcare providers are continually subjected to stress-inducing factors, which may provoke the development of burnout syndrome. Burnout syndrome, or, simply, burnout, is a psychological disorder that was first studied in the field of social services by Freudenberger (1974). Today, in the most widely accepted contextualization, it is characterized by the presence of emotional exhaustion (EE), depersonalization (D), and a diminished sense of personal accomplishment (PA) (Maslach & Jackson, 1981). EE refers to workers’ feeling of physical exertion and also exhaustion of their emotional resources; D is the development of negative feelings and perceptions directed at patients, along with a cynical attitude toward them; and low PA is the tendency of workers to assess themselves negatively in dealing with patients and not feeling fulfilled by their work (Maslach & Jackson, 1981).
The prevalence of burnout is high among nursing staff (Cañadas-De la Fuente et al., 2015), indicating that a high percentage of nurses are emotionally exhausted, as well as have a diminished sense of PA and have developed a depersonalized, cynical attitude toward patients. In the hospital context, this staff group may be the most commonly affected by the syndrome (Bacaicoa Parrado et al., 2012; Losa Iglesias & Becerro de Bengoa Vallejo, 2013). Nurses’ continual exposure to and direct interaction with patients, which is a key factor in the development of the syndrome (Caballero Domínguez, Hederich, & Palacio Sañudo, 2010), may account for the high prevalence of burnout recorded in this population.
Burnout affects not only the physical and mental health of individuals; its consequences are also reflected in workplace contexts, affecting the nursing care provided, patients’ illness and recovery, and the institution itself by increasing rates of absenteeism and sick leave (Epp, 2012; Gasparino, 2014). Consequently, in many countries (e.g., Sweden, the Netherlands), burnout is considered an occupational disease and can be a medical diagnosis (Schaufeli, Leiter, & Maslach, 2009).
Although many nurses are affected by burnout syndrome, not all of them work in the same type of hospital services. Burnout syndrome could be expected to vary from one service to another (Ahmadi, Azizkhani, & Basravi, 2014). For example, some studies describe high burnout levels in services such as emergency departments (Albendín-García et al., 2016) or intensive care units, whereas others show low burnout levels in primary care units (Tomás-Sábado et al., 2010). Of importance is identifying which nurses are at higher risk of developing the disorder in relation to the hospital service in which they work.
The day-to-day practice in the services mentioned previously can be very different from that found in an oncology nursing practice. The case of oncology nursing warrants special attention. Oncology nurses routinely face ethical dilemmas related to the care of patients with cancer (Houlihan, 2015; Pavlish, Brown-Saltzman, Jakel, & Fine, 2014); on a daily basis, they must address highly complex situations involving, among other aspects, suffering (of patients and their families), terminal diagnoses, the delivery of bad news, and mourning and death (Brown & Wood, 2009; Romeo-Ratliff, 2014). Oncology nurses must continually deal with people who have been diagnosed with an illness likely to cause their death. In identifying and empathizing with their patients, nurses are confronted with the reality of their own mortality and of the inevitability of the ultimate loss of health and life (Ksiazek, Stefaniak, Stadnyk, & Ksiazek, 2011). These factors mean a particularly high risk of burnout in oncology nursing and, consequently, of nurses leaving the profession (Romeo-Ratliff, 2014; Toh, Ang, & Devi, 2012).
Numerous studies on burnout in oncology nursing have been published. Some studies have measured the prevalence of burnout among nurses working in oncology (Girgis, Hansen, & Goldstein, 2009), whereas others have investigated sociodemographic, occupational, or psychological risk factors (Gama, Barbosa, & Vieira, 2014). Attention has also been focused on the use of various therapies, such as mindfulness (Moody et al., 2013), art therapy (Italia, Favaro-Scacco, Di Cataldo, & Russo, 2008), and psychotherapeutic interventions (Vázquez-Ortiz et al., 2012), as tools to reduce the level of burnout.
Although reviews have been conducted regarding nurses and other healthcare providers in the field of oncology, none have focused exclusively on burnout syndrome. Some authors, in studies of oncology nurses, have examined the relationships between variables such as shift work, job satisfaction, and burnout (Toh et al., 2012). Others have focused on burnout, psychiatric morbidity, and stress among nurses in the area of pediatric oncology (Mukherjee, Beresford, Glaser, & Sloper, 2009) but without using the Maslach Burnout Inventory (MBI) (Maslach & Jackson, 1981), which is the most widely employed measure. Other reviews have considered the question of stress and the importance of its prevention or reduction in oncology nursing (Hecktman, 2012), whereas others have looked at compassion fatigue (Yang & Kim, 2012), which is commonly experienced in oncology nursing. In addition, meta-analyses of studies of burnout among oncology providers have been carried out; however, these reviews include studies with mixed population samples, which, in many cases, do not include nurses or, if they do, do not provide specific information about this occupational group (Trufelli et al., 2008).
The aim of this review is to focus solely on oncology nurses and on burnout syndrome, evaluated according to the MBI to ensure that the results of all the studies reviewed are fully comparable. This systematic review addresses the following questions: What are the average levels of EE, D, and PA among nurses working in oncology services? What is the prevalence of EE, D, and PA among this population? What factors influence burnout syndrome among oncology nurses?
Methods
This systematic review was conducted in accordance with the recommendations made in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. These recommendations refer to (a) providing an explicit statement of the investigation questions, (b) specifying the criteria used for study eligibility, (c) stating the information sources and search strategy used, and (d) detailing the procedure related to review validity and replicability (Moher et al., 2015; Urrútia & Bonfill, 2010).
Studies selected for inclusion were those that were quantitative and supplied original empirical primary data; published findings in English, Spanish, or Portuguese; used the MBI to measure burnout syndrome; and had a study population comprised, in full or in part, of oncology nurses. Any date of publication was acceptable.
Use of the MBI was selected as one inclusion criteria because (a) the MBI is the most universally accepted instrument for assessing burnout syndrome and (b) the inclusion of studies using another instrument would not permit an integration of results because of different test scoring. Studies with mixed samples in which the level of burnout among oncology nurses was not reported separately were excluded. The decisions not to impose a time limitation, to consult databases containing gray literature, and not to exclude items by reason of the sample size were intended to reduce the possibility of publication bias.
Literature Search and Study Selection
The literature search was conducted in July 2015. The search descriptor and the corresponding equivalent in Spanish and Portuguese was burnout AND oncology nursing, and no search limiter was imposed. The databases consulted were CUIDEN, CINAHL®, LILACS, ProQuest (ebrary, MEDLINE®, ProQuest Deep Indexing: Health, ProQuest Deep Indexing: Medical, ProQuest Health and Medical Complete, PsycARTICLES, and PsycINFO), PubMed, SciELO, and Scopus.
The search for and selection of studies was carried out in four phases and conducted independently by two members of the research team; if they were unable to agree, a third team member was consulted. In the first phase, the studies were selected by reading the title and abstract. After this screening, the second phase consisted of reading the full text of all of the remaining articles and applying the same inclusion and exclusion criteria. In the third phase, the articles were read critically to assess their methodologic quality. The fourth phase consisted of a reverse search of the literature, examining the articles cited in the papers reviewed and in the systematic reviews related to the study topic that had been located during the first search.
Coding and Analysis
The variables considered were recorded in a data collection manual (available on request from the corresponding author). For longitudinal or intervention studies, the baseline or initial measurement data were recorded. The following variables were compiled from each study: (a) the first author’s name; (b) date of publication; (c) language of publication (English, Spanish, Portuguese); (d) study topic; (e) type of publication (article, thesis); (f) type of sampling (random, intentional); (g) type of MBI (Human Services Survey [HSS], General Survey [GS]); (h) impact of the journal impact factor (included or not included in Journal Citation Reports®); (i) mean and standard deviation of EE; (j) mean and standard deviation of D; (k) mean and standard deviation of PA; (l) percentage of the sample with low, medium, and high EE; (m) percentage of the sample with low, medium, and high D; (n) percentage of the sample with low, medium, and high PA; (o) sociodemographic risk factors for EE, D, and PA; (p) occupational risk factors for EE, D, and PA; and (q) psychological risk factors for EE, D, and PA.
The variable MBI type has two values that correspond with the two instrument versions used in the selected studies. The MBI-HSS has 22 items (9 for EE, 5 for D, 8 for PA), and it is exclusively used for social and healthcare workers (Maslach & Jackson, 1981). The MBI-GS has 16 items, can be used in any profession, and maintains the three previous dimensions. The MBI-GS has five items for exhaustion, five items for cynicism or D, and six items for professional efficiency. Both versions have the same conceptual structure and categorize the workers in high, medium, or low levels for each dimension; this categorization is established by cut points that were established by the authors of the test and can be found in the test manual (Maslach, Jackson, & Leiter, 1996).
To ensure the reliability of the data extraction and encoding, these tasks were performed independently by two researchers. The average degree of agreement between them was calculated, for the continuous variables, from the intraclass correlation coefficient. The average value obtained was 0.92 (minimum = 0.86; maximum = 1). The Cohen kappa coefficient was used for categorical variables, and the average value was 0.9 (minimum = 0.83; maximum = 1).
To assess the methodologic quality of the studies included, items from two different guides to critical reading were used. Quasi-experimental studies were evaluated using items 3, 4, 6, 7, 8, 9, 10, and 11 from the checklist of nonrandomized intervention studies proposed by Vallvé, Artés, and Cobo (2005), and observational studies were evaluated using items 2, 3, 4, 5, 6, 15, 16, 17, and 18 from the checklist proposed by Ciaponni (2010).
Results
The search yielded 436 results. After reading the title and abstract of each text, 374 articles were excluded because they did not meet the inclusion criteria. Of the 62 articles that remained for full-text reading, 23 were finally included. Following the critical reading, none were excluded for presenting methodological bias. After the reverse search of the reviews and studies chosen, an additional four articles were included. As a result, the final sample was made up of 27 studies. The search and study selection process is detailed in Figure 1.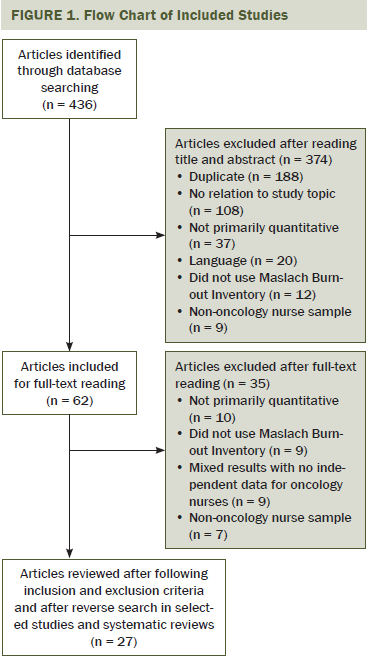
Study Characteristics
The total sample population of the review was composed of 11,107 oncology nurses. Of that number, about 75% were women, and the mean response rate for the studies included was about 74%. Of the included studies, the oldest was published in 1993 and the most recent in 2015. Sixty-five percent of the studies were published from 2009–2015.
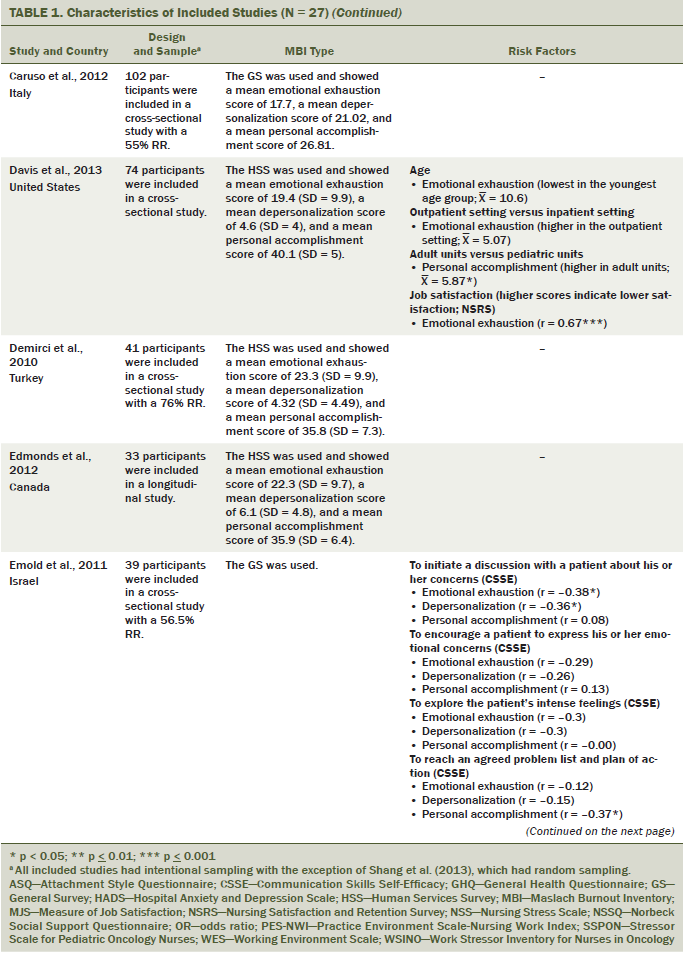
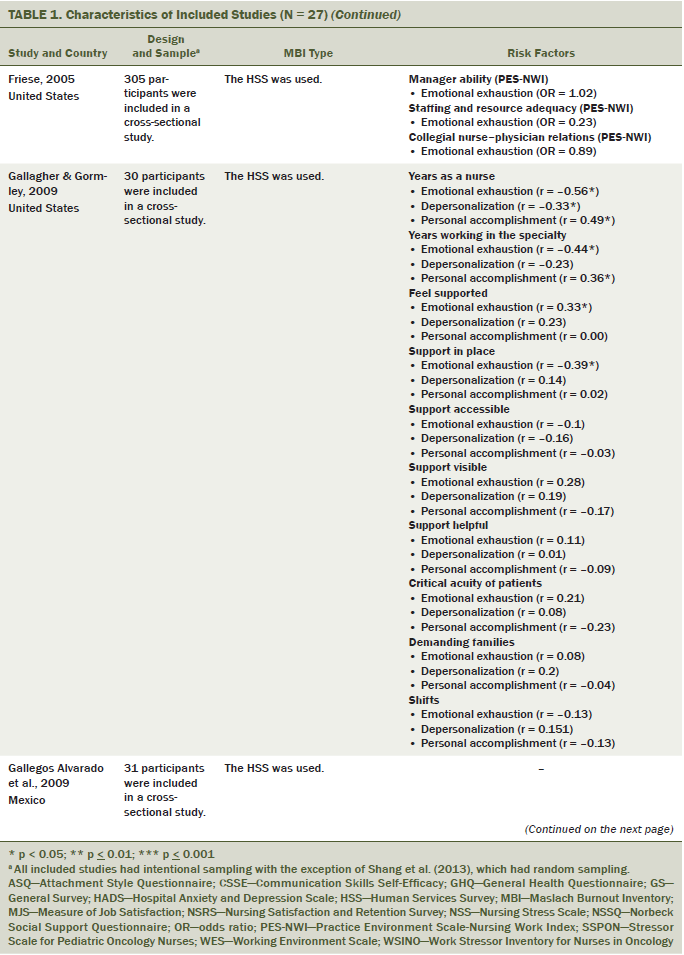
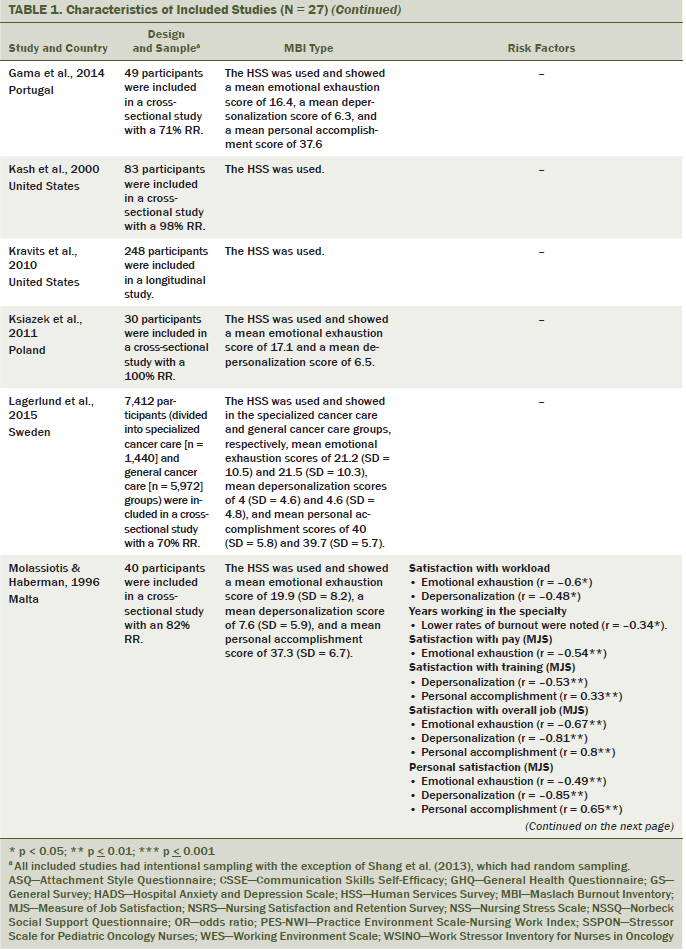
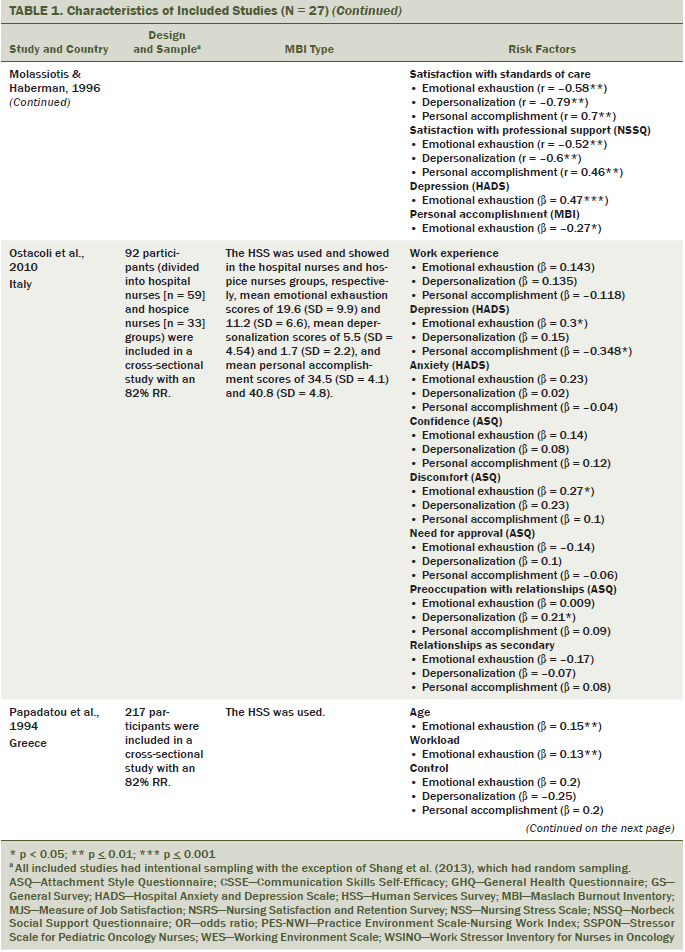
Most of the studies were journal articles; only one doctoral thesis met the criteria for inclusion (Russell, 2014). One study was published in Spanish (Gallegos Alvarado, Parra Domínguez, Castillo Díaz, & Murillo Ortiz, 2009), with the rest in English. Regarding the geographic location of the studies included, about 49% took place in Europe, 37% in the Americas, 11% in Oceania, and 4% in Asia. The MBI subtype most commonly used was the MBI-HSS; only two studies used the MBI-GS (Caruso et al., 2012; Emold, Schneider, Meller, & Yagil, 2011). All of the studies were cross-sectional except those by Edmonds, Lockwood, Bezjak, and Nyhof-Young (2012); Kravits, McAllister-Black, Grant, and Kirk (2010); and Turner et al. (2009), which were longitudinal. Random sampling was used in only one case (Shang, Friese, Wu, & Aiken, 2013). The main characteristics of the 27 articles included in the review and the risk factors identified for burnout syndrome are listed in Table 1.

Prevalence and Mean Values of Burnout
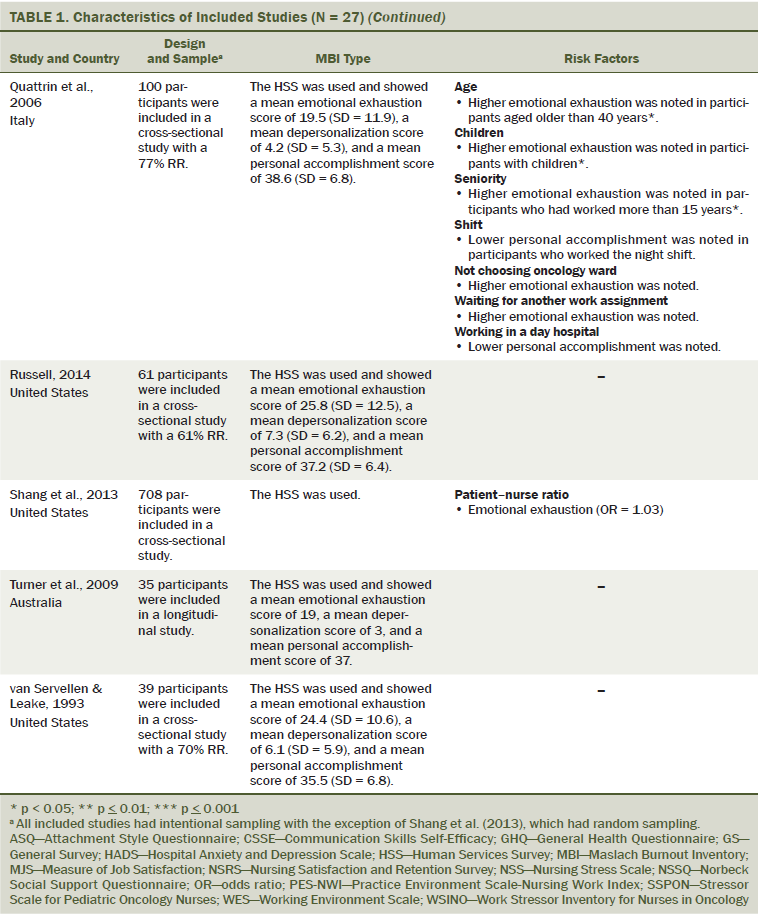
In the articles examined in this review, great variability existed in the average score recorded for the three burnout dimensions (EE, D, PA) that affect oncology nurses. This discrepancy was also present in the percentages found for the prevalence of low, medium, or high degrees of burnout in each of the dimensions. About 3%–38% of sample populations are reported to suffer from severe EE; the highest value was reported by Kravits et al. (2010), but similarly high levels of prevalence have been reported by Barrett and Yates (2002) and Ostacoli et al. (2010) (about 37% for each). Conversely, other studies have observed a high prevalence of the mildest form of EE; Gallegos Alvarado et al. (2009) reported 84% of this subtype and Bressi et al. (2008) 46%. In between these extremes are studies that have observed a high prevalence of moderate levels of EE, which would indicate the existence of nursing providers who are at risk of experiencing emotional exhaustion (Gallagher & Gormley, 2009; Molassiotis & Haberman, 1996).
Unlike the other two dimensions, for D, the predominant values of the samples of each study are more homogeneous, with most studies reporting low levels of D; Gallegos Alvarado et al. (2009) reported that 97% of participants presented low levels of D, and Gallagher and Gormley (2009) observed about 63% of participants to be in this category. However, some studies reported a high prevalence of the most severe D (Lagerlund, Sharp, Lindqvist, Runesdotter, & Tishelman, 2015; Ostacoli et al., 2010; Papadatou, Anagnostopoulos, & Monos, 1994) or of moderate D (Gallagher & Gormley, 2009; Molassiotis & Haberman, 1996).
For PA, the values reported correspond mainly to the low end of the scale (Gallegos Alvarado et al., 2009; Kravits et al., 2010). However, Alacacioglu, Yavuzsen, Dirioz, Oztop, and Yilmaz (2009) reported that 100% of the sample reported an absence of personal accomplishment in their work.
Table 2 shows the percentages of participants in each study who presented high, medium, or low levels with respect to each of the dimensions of the syndrome. Not all of the studies in this review reported the prevalence of each level for each dimension, but they did all provide descriptive information about the average values within the study population for each dimension.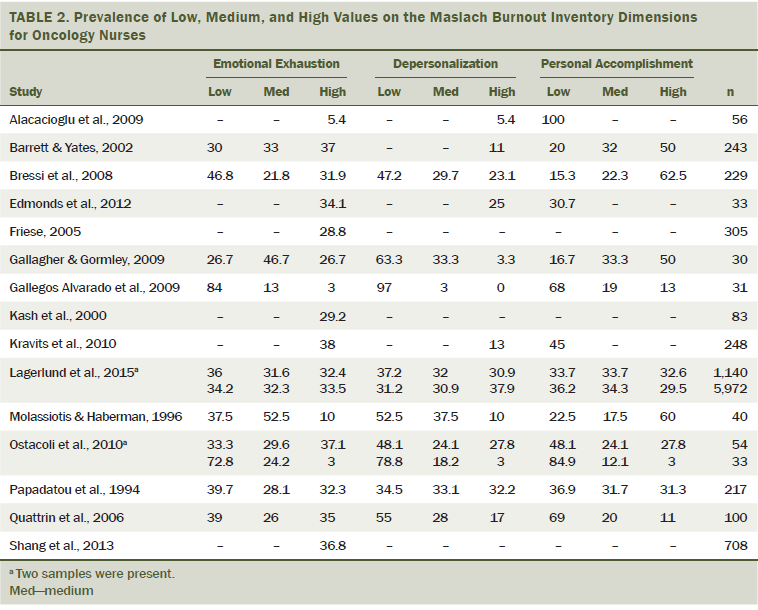
Among the articles that only reported the average values (N = 17), and following the classification proposed by Maslach et al. (1996) of low, medium, and high values for each dimension, the studies in question would be grouped as follows: for EE, 3 report low average levels, 13 report moderate levels, and 1 reports high levels; for D, 14 report low average levels, and 3 report moderate levels; and for PA, 3 report low average levels, 13 report moderate levels, and 1 reports high levels. The studies that only inform about average values follow a similar distribution to those that inform about prevalence values: They suggest that oncology nurses present medium and high levels of EE, and that they do not feel completely fulfilled with their work but do not usually have a negative and cynical attitude toward patients.
Risk Factors for Burnout Syndrome
A wide variety of variables may influence or provoke burnout among oncology nurses. Current practice in studies of these risk factors is to classify them into three groups: sociodemographic, occupational, and psychological (Vargas, Cañadas, Aguayo, Fernández, & De la Fuente, 2014). This classification scheme was adopted accordingly.
Sociodemographic factors: Several studies have analyzed age as a risk factor for burnout, and youth is generally agreed on as a protective factor against EE. Consequently, younger oncology nurses appear to experience less EE (Davis, Lind, & Sorensen, 2013; Papadatou et al., 1994), and it is more prevalent among those aged older than 40 years (Quattrin et al., 2006). However, Caruso et al. (2012) found no significant differences in this regard. Gender, marital status, and level of training do not seem to exert a significant influence on the development of burnout (Alacacioglu et al., 2009; Caruso et al., 2012). However, Quattrin et al. (2006) found that nurses with children are at greater risk of developing EE.
Occupational factors: In the studies reviewed, the factor that has been most extensively analyzed is that of occupational variables and their influence on burnout. Seniority in the profession and in oncology nursing is a protective factor against burnout (Gallagher & Gormley, 2009), although other authors (Alacacioglu et al., 2009; Escot, Artero, Gandubert, Boulenger, & Ritchie, 2001; Ostacoli et al., 2010; Quattrin et al., 2006) have reported that greater experience may aggravate burnout. Other factors that protect against burnout include job satisfaction (Davis et al., 2013; Molassiotis & Haberman, 1996), work with hospitalized adult patients, the presence of positive features in the workplace (Davis et al., 2013; Emold et al., 2011), and higher salaries (Molassiotis & Haberman, 1996).
Risk factors that have been highlighted include workload, the need to cope with death, and the pain and suffering of patients and their families. These factors tend to increase EE and D and reduce PA, placing nurses at greater risk of burnout (Borteyrou, Truchot, & Rascle, 2014). A similar outcome has been reported for workload, which is associated with higher levels of EE and D (Borteyrou et al., 2014; Papadatou et al., 1994) and lower levels of PA (Molassiotis & Haberman, 1996). Shift work appears to increase D and decrease PA and EE but not significantly so for any of the dimensions (Gallagher & Gormley, 2009). In contrast, nurses who work the night shift exclusively present a significantly lower degree of PA (Quattrin et al., 2006). Other factors that may provoke the development of burnout are the presence of work stressors, such as perceiving that mistakes might be made or that accomplishing all of the tasks required is impossible, or witnessing the suffering of patients’ families (Barnard, Street, & Love, 2006). Additional factors include having to deal with death, dying, and the suffering of patients and relatives (Borteyrou et al., 2014).
Psychological factors: Satisfaction in the workplace seems to be a protective factor against burnout, increasing PA and decreasing EE and D (Molassiotis & Haberman, 1996). However, other psychological variables, such as depression, anxiety, and the presence of interpersonal conflict, act as risk factors, increasing EE and D and decreasing PA (Borteyrou et al., 2014; Ostacoli et al., 2010), as does the fear of cancer (Molassiotis & Haberman, 1996).
Other factors: The articles reviewed also mentioned other risk factors related to burnout, including psychiatric health, an area in which disorders are associated with greater EE and D and reduced PA (Escot et al., 2001). Other variables, such as social support, professional support, and communication skills, have been shown to protect nurses against the development of burnout (Emold et al., 2011; Molassiotis & Haberman, 1996). Oncology nurses are more likely to present EE if they did not choose to work in oncology or are in line to be transferred to another service (Quattrin et al., 2006). They also experience more burnout when they feel they do not connect with patients or if they feel their experience is not being taken into account in decision-making processes (Escot et al., 2001).
Discussion
The aim of this review of research studies into burnout syndrome among oncology nurses was to determine the average levels and the prevalence of high, moderate, and low scores for the three dimensions of burnout, as well as the factors that influence development of the syndrome.
Similar reviews regarding burnout in nurses in other areas of health care (Adriaenssens, De Gucht, & Maes, 2015; Albendín-García et al., 2016) have highlighted the importance of studying burnout levels and risk factors, focusing on the areas in which nurses carry out their work because of the peculiarity of each hospital service. However, reviews of burnout in oncology nursing have not focused exclusively on burnout syndrome as this review does, and the number of studies analyzed in these reviews are less than in this study (Mukherjee et al., 2009; Toh et al., 2012).
In the current review, the studies analyzed report a greater prevalence of high levels of EE and low levels of D and PA. These findings should be taken into account in view of international research results of similarly high levels of burnout among nurses (Cañadas-De la Fuente et al., 2015), particularly for oncology nurses. In this respect, several studies have reported a high prevalence of EE, affecting more than 30% of the sample population, and of D, affecting more than 20% of the sample population, together with low levels of PA, which appears to be the main problem in this area of health care (Alacacioglu et al., 2009; Gallegos Alvarado et al., 2009). This finding reflects the fact that oncology nurses are subjected to greater stress than healthcare providers in other areas (Eelen et al., 2014). Although nurses may derive great satisfaction from working with patients with cancer (Jasperse, Herst, & Dungey, 2014), the psychological and physical impact of the disease leads to significant EE (Edmonds et al., 2012). The stress of working with these patients generates D (Jasperse et al., 2014), and, above all, it inevitably erodes feelings of PA (Emold et al., 2011). The burnout pattern for oncology nurses—high EE with low PA and low D—is repeated in other healthcare providers, such as clinical oncologists and palliative care physicians (Asai et al., 2007). Nevertheless, other studies with oncologists, pediatricians, and general practitioners have reported a higher D level (Arigoni, Bovier, Mermillod, Waltz, & Sappino, 2009).
The prevalence of each level in the three dimensions varies considerably among the studies reviewed. This may be because the samples correspond to different countries, which may be relevant to the influence of the syndrome (Pisanti, van der Doef, Maes, Lazzari, & Bertini, 2011; Tourigny, Baba, & Wang, 2010; van der Schoot, Oginska, & Estryn-Behar, 2003) because each country has a healthcare system with its own characteristics regarding nurses’ training, workload, and remuneration (Hasselhorn, Widerszal-Bazyl, & Radkiewicz, 2003; van der Schoot et al., 2003). In addition, the reliability or otherwise translation, adaptation, and validation of questionnaires in each country must be taken into account. As indicated by Vargas et al. (2014), the language used in questionnaires and the adaptations made can moderate the observed relationship between burnout and its risk factors. Consequently, oncology nurses present higher levels of EE in studies carried out in the United States, Italy, and Australia (Barrett & Yates, 2002; Kravits et al., 2010; Ostacoli et al., 2010), whereas levels of D are significantly higher in studies carried out in Greece, Italy, and Canada (Edmonds et al., 2012; Ostacoli et al., 2010; Papadatou et al., 1994). The lowest levels of PA have been measured in Turkey, Mexico, and Italy (Alacacioglu et al., 2009; Gallegos Alvarado et al., 2009; Quattrin et al., 2006).
The main risk factors of burnout among oncology nurses include advanced age; greater work experience; a heavy workload; the need to deal with patients with terminal cancer, pain, suffering, and death; the presence of job stressors; and depression (Barnard et al., 2006; Borteyrou et al., 2014; Davis et al., 2013; Gallagher & Gormley, 2009; Quattrin et al., 2006). In other words, a nurse who is young and relatively inexperienced may be more protected against the development of burnout in the oncology setting; however, in other populations, a greater length of service and longer work experience may protect against burnout (Gallagher & Gormley, 2009), as may the satisfaction of working in this area (Gama et al., 2014) and with these patients (Jasperse et al., 2014). The special characteristics of patients make oncology a high-risk area for nurses who must continually deal with situations involving death, pain, and suffering (Brown & Wood, 2009; Romeo-Ratliff, 2014). Therefore, any review of this area must take into account the differing contexts in which studies are conducted.
Various protective factors against burnout have also been identified. Job satisfaction, personal satisfaction, and salary are important, as is the support received from colleagues and the communication skills of all concerned (Jasperse et al., 2014; Molassiotis & Haberman, 1996). These skills are often cited by nurses as one of the main priorities of ongoing training, as good communication has a very positive effect in reducing burnout in oncology and related settings (Jasperse et al., 2014). All of these factors contribute to making the oncology setting a rewarding one in which to work (Converso, Loera, Viotti, & Martini, 2015).
Despite this consideration on the relationship between risk factors and burnout, in many cases, the relationships are contradictory. A clear example of this is the question of experience (Albendín-García et al., 2016); accordingly, more research is needed regarding burnout and its association with this and other variables (Ahmadi et al., 2014; García-Izquierdo & Ríos-Rísquez, 2012) to obtain a better understanding of risk profiles. For a quantitative analysis of the heterogeneity among studies, a meta-analysis should be conducted to determine the average effect size of each variable in relation to burnout. Unfortunately, the studies obtained in the current literature search did not contain sufficient information for this information to be extracted; this could be done when more articles are published with empirical data on the questions addressed in this systematic review (Sánchez-Meca & Botella, 2010).
Limitations
This study presents some limitations. A meta-analytic method was not used to summarize the data obtained because of the lack of sufficient studies analyzing the risk factors in question. In addition, most of the studies examined use the MBI scale for the general population. As far as the current authors know, no MBI adaptation exists for nursing providers. The MBI-HSS and MBI-GS have been widely used with all types of professionals, although having an adaptation of these tests for nursing providers would be interesting; if this adaptation had existed, researchers would have been able to come to different conclusions in the evaluation of burnout syndrome. For nursing samples, the psychometric properties, validity, and reliability of burnout instruments have been checked by some authors to develop a specific scale for nurses (De la Fuente et al., 2013, 2015).
Implications for Practice
A significant number of oncology nurses suffer from EE and low levels of PA. Nurses should be aware of the high physical and emotional demands that may be involved when working in the oncology setting. In this area, nurses must face the need to communicate bad news to the patient and his or her family, along with pain, suffering, and death. Oncology nurses should also be aware that the care and treatment they provide will not always be sufficient for the patient to defeat the illness; this should not make them have feelings of low personal and professional satisfaction.
Additional studies that identify protective and risk factors for the syndrome are needed. In addition, these studies should be analyzed more comprehensively to establish burnout prevention programs. Nursing research should focus on developing programs to identify interventions that would reduce EE and enhance feelings of PA in oncology nurses.
Conclusion
Oncology nurses are vulnerable to burnout. The prevalence of this condition, regarding the dimension of D, does not appear to be alarming. Nevertheless, many oncology nurses are at risk of developing the syndrome because significant levels of high EE and low PA have been reported. The variables that appear to exert most influence, either as risk factors or as protection against the syndrome, are age, experience (or seniority), workload, job satisfaction, and issues related to health care (e.g., having communication skills; coping with suffering, pain, and death). Additional research is needed to compile empirical information on these variables so that quantitative and meta-analytic reviews of the subject can be carried out.
References
Adriaenssens, J., De Gucht, V., & Maes, S. (2015). Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. International Journal of Nursing Studies, 52, 649–661. doi:10.1016/j.ijnurstu.2014.11.004
Ahmadi, O., Azizkhani, R., & Basravi, M. (2014). Correlation between workplace and occupational burnout syndrome in nurses. Advanced Biomedical Research, 3, 44. doi:10.4103/2277-9175.125751
Alacacioglu, A., Yavuzsen, T., Dirioz, M., Oztop, I., & Yilmaz, U. (2009). Burnout in nurses and physicians working at an oncology department. Psycho-Oncology, 18, 543–548. doi:10.1002/pon.1432
Albendín-García, L., Gómez-Urquiza, J.L., Cañadas-De la Fuente, G.A., Cañadas, G.R., San Luis, C., & Aguayo, R. (2016). Prevalencia bayesiana y niveles de burnout en enfermería de urgencias. Una revisión sistemática [Bayesian prevalence and burnout levels in emergency nurses. A systematic review]. Revista Latinoamericana de Psicología, 48, 137–145. doi:10.1016/j.rlp.2015.05.004
Arigoni, F., Bovier, P.A., Mermillod, B., Waltz, P., & Sappino, A.P. (2009). Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: Who are most at risk? Supportive Care in Cancer, 17, 75–81. doi:10.1007/s00520-008-0465-6
Asai, M., Morita, T., Akechi, T., Sugawara Y., Fujimori, M., Akizuki, N., . . . Uchitomi, Y. (2007). Burnout and psychiatric morbidity among physicians engaged in end-of-life care for cancer patients: A cross-sectional nationwide survey in Japan. Psycho-Oncology, 16, 421–428. doi:10.1002/pon.1066
Bacaicoa Parrado, P., Díaz Herrera, V., Gea Valero, M., Linares Pérez, J., Araya Pérez, E., Alba Domínguez J.F., . . . Marrero Mederos, M.J. (2012). Comparativa del síndrome burnout entre el personal de enfermería en cardiología de dos hospitales de tercer nivel [Burnout syndrome comparison among nurses in the cardiology departments of two tertiary hospitals]. Enfermería en Cardiología, 19, 34–40.
Barnard, D., Street, A., & Love, A.W. (2006). Relationships between stressors, work supports, and burnout among cancer nurses. Cancer Nursing, 29, 338–345. doi:10.1097/00002820-200607000-00013
Barrett, L., & Yates, P. (2002). Oncology/haematology nurses: A study of job satisfaction, burnout, and intention to leave the specialty. Australian Health Review, 25, 109–121. doi:10.1071/ah020109
Borteyrou, X., Truchot, D., & Rascle, N. (2014). Development and validation of the Work Stressor Inventory for Nurses in Oncology: Preliminary findings. Journal of Advanced Nursing, 70, 443–453. doi:10.1111/jan.12231
Bressi, C., Manenti, S., Porcellana, M., Cevales, D., Farina, L., Felicioni I., . . . Invernizzi, G. (2008). Haemato-oncology and burnout: An Italian Survey. British Journal of Cancer, 98, 1046–1052. doi:10.1038/sj.bjc.6604270
Brown, C., & Wood, A. (2009). Oncology nurses’ grief: A literature review. Clinical Journal of Oncology Nursing, 13, 625–627. doi:10.1188/09.CJON.625-627
Caballero Domínguez, C.C., Hederich, C., & Palacio Sañudo, J.E. (2010). El burnout académico: Delimitación del síndrome y factores asociados con su aparición [Academic burnout: Delineation of the syndrome and factors associated with its emergence]. Revista Latinoamericana de Psicología, 42, 131–146.
Cañadas-De la Fuente, G.A., Vargas, C., San Luis, C., García, I., Cañadas, G.R., & De la Fuente, E.I. (2015). Risk factors and prevalence of burnout syndrome in the nursing profession. International Journal of Nursing Studies, 52, 240–249. doi:10.1016/j.ijnurstu.2014.07.001
Caruso, A., Vigna, C., Bigazzi, V., Sperduti, I., Bongiorno, L., & Allocca, A. (2012). Burnout among physicians and nurses working in oncology. La Medicina del Lavoro, 103, 96–105.
Ciapponi, A. (2010). Guía de lectura crítica de estudios observacionales en epidemiología (primera parte) [Critical appraisal guide of observational studies in epidemiology (first part)]. Evidencia: Actualización en la Práctica Ambulatoria, 13, 135–140.
Converso, D., Loera, B., Viotti, S., & Martini, M. (2015). Do positive relations with patients play a protective role for healthcare employees? Effects of patients’ gratitude and support on nurses’ burnout. Frontiers in Psychology, 6, 470. doi:10.3389/fpsyg.2015.00470
Davis, S., Lind, B.K., & Sorensen, C. (2013). A comparison of burnout among oncology nurses working in adult and pediatric inpatient and outpatient settings. Oncology Nursing Forum, 40, E303–E311. doi:10.1188/13.ONF.E303-E311
De la Fuente, E.I., García, J., Cañadas, G.A., San Luis, C., Cañadas, G.R., Aguayo, R., . . . Vargas, C. (2015). Psychometric properties and scales of the Granada Burnout Questionnaire applied to nurses. International Journal of Clinical and Health Psychology, 15, 130–138. doi:10.1016/j.ijchp.2015.01.001
De la Fuente, E.I., Lozano, L.M., García-Cueto, E., San Luis, C., Vargas, C., Cañadas, G.R., . . . Hambleton, R.K. (2013). Development and validation of the Granada Burnout Questionnaire in Spanish police. International Journal of Clinical and Health Psychology, 13, 216–225. doi:10.1016/s1697-2600(13)70026-7
Demirci, S., Yildirim, Y.K., Ozsaran, Z., Uslu, R., Yalman, D., & Aras, A.B. (2010). Evaluation of burnout syndrome in oncology employees. Medical Oncology, 27, 968–974. doi:10.1007/s12032-009-9318-5
Edmonds, C., Lockwood, G.M., Bezjak, A., & Nyhof-Young, J. (2012). Alleviating emotional exhaustion in oncology nurses: An evaluation of Wellspring’s “Care for the Professional Caregiver Program.” Journal of Cancer Education, 27, 17–36. doi:10.1007/s13187-011-0278-z
Eelen, S., Bauwens, S., Baillon, C., Distelmans, W., Jacobs, E., & Verzelen, A. (2014). The prevalence of burnout among oncology professionals: Oncologists are at risk of developing burnout. Psycho-Oncology, 23, 1415–1422. doi:10.1002/pon.3579
Emold, C., Schneider, N., Meller, I., & Yagil, Y. (2011). Communication skills, working environment and burnout among oncology nurses. European Journal of Oncology Nursing, 15, 358–363. doi:10.1016/j.ejon.2010.08.001
Epp, K. (2012). Burnout in critical care nurses: A literature review. Dynamics, 23, 25–31.
Escot, C., Artero, S., Gandubert, C., Boulenger, J.P., & Ritchie, K. (2001). Stress levels in nursing staff working in oncology. Stress and Health, 17, 273–279. doi:10.1002/smi.907
Freudenberger, H.J. (1974). Staff burn-out. Journal of Social Issues, 30, 159–165.
Friese, C.R. (2005). Nurse practice environments and outcomes: Implications for oncology nursing. Oncology Nursing Forum, 32, 765–772. doi:10.1188/05.ONF.765-772
Gallagher, R., & Gormley, D.K. (2009). Perceptions of stress, burnout and support systems in pediatric bone marrow transplantation nursing. Clinical Journal of Oncology Nursing, 13, 681–685. doi:10.1188/09.CJON.681-685
Gallegos Alvarado, M., Parra Domínguez, M.L., Castillo Díaz, R., & Murillo Ortiz, E. (2009). Síndrome de burnout y factores psicosociales del personal de enfermería al cuidado del paciente oncológico [Burn-out syndrome and psycho-social factors of nurses in the care of oncologic patient]. Revista CONAMED, 14, 28–33.
Gama, G., Barbosa, F., & Vieira, M. (2014). Personal determinants of nurses’ burnout in end of life care. European Journal of Oncology Nursing, 18, 527–533. doi:10.1016/j.ejon.2014.04.005
García-Izquierdo, M., & Ríos-Rísquez, M.I. (2012). The relationship between psychosocial job stress and burnout in emergency departments: An exploratory study. Nursing Outlook, 60, 322–329. doi:10.1016/j.outlook.2012.02.002
Gasparino, R.C. (2014). Burnout syndrome in the nursing team of a teaching hospital. Cogitare Enfermagem, 19, 210–216.
Girgis, A., Hansen, V., & Goldstein, D. (2009). Are Australian oncology health professionals burning out? A view from the trenches. European Journal of Cancer, 45, 393–399. doi:10.1016/j.ejca.2008.09.029
Hasselhorn, H.M., Widerszal-Bazyl, M., & Radkiewicz, P. (2003). Burnout in the nursing profession in Europe. In H.M. Hasselhorn, P. Tackbenberg, & Bernd Hans Müller (Eds.), Working conditions and intent to leave the profession among nursing staff in Europe (pp. 53–57). Stockholm, Sweden: National Institute for Working Life and Authors.
Hecktman, H.M. (2012). Stress in pediatric oncology nurses. Journal of Pediatric Oncology Nursing, 29, 356–361. doi:10.1177/1043454212458367
Houlihan, N.G. (2015). A review of “Challenging situations when administering palliative chemotherapy—A nursing perspective.” Oncology Nursing Forum, 42, 319–320. doi: 10.1188/15.ONF.319-320
Italia, S., Favara-Scacco, C., Di Cataldo, A., & Russo, G. (2008). Evaluation and art therapy treatment of the burnout syndrome in oncology units. Psycho-Oncology, 17, 676–680. doi:10.1002/pon.1293
Jasperse, M., Herst, P., & Dungey, G. (2014). Evaluating stress, burnout and job satisfaction in New Zealand radiation oncology departments. European Journal of Cancer Care, 23, 82–88. doi:10.1111/ecc.12098
Kash, K.M., Holland, J.C., Breitbart, W., Berenson, S., Dougherty, J., Ouellette-Kobasa, S., & Lesko, L. (2000). Stress and burnout in oncology. Oncology, 14, 1621–1633.
Kravits, K., McAllister-Black, R., Grant, M., & Kirk, C. (2010). Self-care strategies for nurses: A psycho-educational intervention for stress reduction and the prevention of burnout. Applied Nursing Research, 23, 130–138. doi:10.1016/j.apnr.2008.08.002
Ksiazek, I., Stefaniak, T.J., Stadnyk, M., & Ksiazek, J. (2011). Burnout syndrome in surgical oncology and general surgery nurses: A cross-sectional study. European Journal of Oncology Nursing, 15, 347–350. doi:10.1016/j.ejon.2010.09.002
Lagerlund, M., Sharp, L., Lindqvist, R., Runesdotter, S., & Tishelman, C. (2015). Intention to leave the workplace among nurses working with cancer patients in acute care hospitals in Sweden. European Journal of Oncology Nursing, 19, 629–637. doi:10.1016/j.ejon.2015.03.011
Losa Iglesias, M.E., & Becerro de Bengoa Vallejo, R. (2013). Prevalence and relationship between burnout, job satisfaction, stress, and clinical manifestations in Spanish critical care nurses. Dimensions of Critical Care Nursing, 32, 130–137. doi:10.1097/DCC.0b013e31828647fc
Maslach, C., & Jackson, S.E. (1981). The measurement of experienced burnout. Journal of Organizational Behavior, 2, 99–113. doi:10.1002/job.4030020205
Maslach, C., Jackson, S.E., & Leiter, M.P. (1996). The Maslach Burnout Inventory (3rd ed.). Palo Alto, CA: Consulting Psychologists Press.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., . . . Stewart, L.A. (2015). Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4, 1. doi:10.1186/2046-4053-4-1
Molassiotis, A., & Haberman, M. (1996). Evaluation of burnout and job satisfaction in marrow transplant nurses. Cancer Nursing, 19, 360–367. doi:10.1097/00002820-199610000-00005
Moody, K., Kramer, D., Santizo, R.O., Magro, L., Wyshogrod, D., Ambrosio, J., . . . Stein, J. (2013). Helping the helpers: Mindfulness training for burnout in pediatric oncology—A pilot program. Journal of Pediatric Oncology Nursing, 30, 275–284. doi:10.1177/1043454213504497
Mukherjee, S., Beresford, B., Glaser, A., & Sloper, P. (2009). Burnout, psychiatric morbidity, and work-related sources of stress in paediatric oncology staff: A review of the literature. Psycho-Oncology, 18, 1019–1028. doi:10.1002/pon.1534
Ostacoli, L., Cavallo, M., Zuffranieri, M., Negro, M., Sguazzotti, E., Picci, R.L., . . . Furlan, P.M. (2010). Comparison of experienced burnout symptoms in specialist oncology nurses working in hospital oncology units or in hospices. Palliative and Supportive Care, 8, 427–432. doi:10.1017/S1478951510000295
Papadatou, D., Anagnostopoulos, F., & Monos, D. (1994). Factors contributing to the development of burnout in oncology nursing. British Journal of Medical Psychology, 67, 187–199. doi:10.1111/j.2044-8341.1994.tb01785.x
Pavlish, C., Brown-Saltzman, K., Jakel, P., & Fine, A. (2014). The nature of ethical conflicts and the meaning of moral community in oncology practice. Oncology Nursing Forum, 41, 130–140. doi:10.1188/14.ONF.130-140
Pisanti, R., van der Doef, M., Maes, S., Lazzari, D., & Bertini, M. (2011). Job characteristics, organizational conditions and distress/well-being among Italian and Dutch nurses: A cross-national comparison. International Journal of Nursing Studies, 48, 829–837. doi:10.1016/j.ijnurstu.2010.12.006
Quattrin, R., Zanini, A., Nascig, E., Annunziata, M.A., Calligaris, L., & Brusaferro, S. (2006). Level of burnout among nurses working in oncology in an Italian region. Oncology Nursing Forum, 33, 815–820. doi:10.1188/06.ONF.815-820
Romeo-Ratliff, A. (2014). An investigation into the prevalence of and relationships among compassion fatigue, burnout, compassion satisfaction, and self-transcendence in oncology nurses [Doctoral thesis]. Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3617709)
Russell, K. (2014). The perceptions of burnout, its prevention and its effect on patient care as described by oncology nurses in the hospital setting [Doctoral thesis]. Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3618494)
Sánchez-Meca, J., & Botella, J. (2010). Revisiones sistemáticas y metaanálisis: Herramientas para la práctica profesional [Systematic reviews and meta-analyses: Tools for professional practice]. Papeles del Psicólogo, 31, 7–17.
Schaufeli, W.B., Leiter, M.P., & Maslach, C. (2009). Burnout: 35 years of research and practice. Career Development International, 14, 204–220. doi:10.1108/13620430910966406
Shang, J., Friese, C.R., Wu, E., & Aiken, L.H. (2013). Nursing practice environment and outcomes for oncology nursing. Cancer Nursing, 36, 206–212. doi:10.1097/NCC.0b013e31825e4293
Toh, S.G., Ang, E., & Devi, M.K. (2012). Systematic review on the relationship between the nursing shortage and job satisfaction, stress and burnout levels among nurses in oncology/haematology settings. International Journal of Evidence-Based Healthcare, 10, 126–141. doi:10.1111/j.1744-1609.2012.00271.x
Tomás-Sábado, J., Maynegre-Santaularia, M., Pérez-Bartolomé, M., Alsina-Rodríguez, M., Quinta-Barbero, R., & Granell-Navas, S. (2010). Síndrome de burnout y riesgo suicida en enfermeras de atención primaria [Burnout syndrome and suicide risk among primary care nurses]. Enfermería Clínica, 20, 173–178.
Tourigny, L., Baba, V.V., & Wang, X. (2010). Burnout and depression among nurses in Japan and China: The moderating effects of job satisfaction and absence. International Journal of Human Resource Management, 21, 2741–2761. doi:10.1080/09585192.2010.528656
Trufelli, D.C., Bensi, C.G., Garcia, J.B., Narahara, J.L., Abrão, M.N., Diniz, R.W., . . . Del Giglio, A. (2008). Burnout in cancer professionals: A systematic review and meta-analysis. European Journal of Cancer Care, 17, 524–531. doi:10.1111/j.1365-2354.2008.00927.x
Turner, J., Clavarino, A., Butow, P., Yates, P., Hargraves, M., Connors, V., & Hausmann, S. (2009). Enhancing the capacity of oncology nurses to provide supportive care for parents with advanced cancer: Evaluation of an educational intervention. European Journal of Cancer, 45, 1798–1806. doi:10.1016/j.ejca.2009.02.023
Urrútia, G., & Bonfill, X. (2010). PRISMA declaration: A proposal to improve the publication of systematic reviews and meta-analysis. Medicina Clínica, 135, 507–511.
Vallvé, C., Artés, M., & Cobo, E. (2005). Non-randomized evaluation studies (TREND). Medicina Clínica, 125(Suppl. 1), 38–42.
van der Schoot, E., Oginska, H., & Estryn-Behar, M. (2003). Burnout in the nursing profession in Europe. In H.M. Hasselhorn, P. Tackbenberg, & Bernd Hans Müller (Eds.), Working conditions and intent to leave the profession among nursing staff in Europe (pp. 53–57). Stockholm, Sweden: National Institute for Working Life and Authors.
van Servellen, G., & Leake, B. (1993). Burn-out in hospital nurses: A comparison of acquired immunodeficiency syndrome, oncology, general medical, and intensive care unit nurse samples. Journal of Professional Nursing, 9, 169–177. doi:10.1016/8755-7223(93)90069-o
Vargas, C., Cañadas, G.A., Aguayo, R., Fernández, R., & De la Fuente, E.I. (2014). Which occupational risk factors are associated with burnout in nursing? A meta-analytic study. International Journal of Clinical and Health Psychology, 14, 28–38. doi:10.1016/S1697-2600(14)70034-1
Vázquez-Ortiz, J., Vázquez-Ramos, M.J., Álvarez-Serrano, M., Reyes-Alcaide, M., Martínez-Domingo, R., Nadal-Delgado, M., & Cruzado, J.A. (2012). Intervención psicoterapeútica grupal intensiva realizada en un entorno natural para el tratamiento del burnout en un equipo de enfermería oncológica. Psicooncología, 9, 161–182.
Yang, Y.H., & Kim, J.K. (2012). A literature review of compassion fatigue in nursing. Korean Journal of Adult Nursing, 24, 38–51. doi:10.7475/kjan.2012.24.1.38
About the Author(s)
Gómez-Urquiza is a nursing lecturer in the Department of Nursing and Faculty of Health Sciences at the University of Granada in Ceuta, Spain; Aneas-López is a staff nurse at the Queen Alexandra Hospital in Portsmouth, Hampshire, United Kingdom; De la Fuente-Solana is a professor in the Brain, Mind, and Behavior Research Center at the University of Granada; Albendín-García is a nurse at the Andalusian Health Service in Córdoba, Spain; and Díaz-Rodríguez and Cañadas-De la Fuente are both professors in the Department of Nursing and Faculty of Health Sciences at the University of Granada. This research was funded by the Excellence Research Project P11HUM-7771 (Junta de Andalucía, Spain) and the Research Project mP_BS_6 (CEI BioTic Granada and Ministerio de Ciencia e Innovación, Spain). Gómez-Urquiza and Cañadas-De la Fuente contributed to the conceptualization and design. Aneas-López, Albendin-García, and Díaz-Rodríguez completed the data collection. Gómez-Urquiza and De la Fuente-Solana provided the statistical support and analysis. Gómez-Urquiza, Aneas-López, De la Fuente-Solana, Albendín-García, Díaz-Rodríguez, and Cañadas-De la Fuente contributed to the manuscript preparation. This study is part of Gómez-Urquiza’s doctoral dissertation that is in development for the degree of Doctorate in Psychology at the University of Granada. Gómez-Urquiza can be reached at jlgurquiza@ugr.es, with copy to editor at ONFEditor@ons.org. Submitted August 2015. Accepted for publication November 10, 2015.

