Changing Practice: Frameworks From Implementation Science
A critical time lag exists from the generation of new knowledge to integration into direct patient care. One effort to address this problem is through clinical initiatives to translate research findings into everyday practice at the unit, department, or institutional level. Such efforts can be particularly challenging when faced with the real-world conditions that healthcare professionals must confront in their day-to-day practice. These initiatives may be in response to an external requirement, a desire to improve practice, or to change care delivery to a more evidence-based model.
Jump to a section
A critical time lag exists from the generation of new knowledge to integration into direct patient care. The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine (2013) report on high-quality cancer care includes recommendations for evidence-based care and translating evidence into clinical practice. One effort to address this problem is through clinical initiatives to translate research findings into everyday practice at the unit, department, or institutional level. Such efforts can be particularly challenging when faced with the real-world conditions that healthcare professionals must confront in their day-to-day practice. These initiatives may be in response to an external requirement, a desire to improve practice, or to change care delivery to a more evidence-based model.
Oncology nurses are leaders and pivotal players in evidence-based practice changes. Emergence of the doctor of nursing practice (DNP) degree in the past decade has provided additional education for advanced practice oncology nurses and nurse executives to develop and lead evidence-based implementation initiatives to improve the delivery and quality of care in specific practice settings. However, creating sustainable change is not easy because challenging the status quo is not a comfortable process for most individuals and organizations.
The purpose of this article is to provide an overview of conceptual approaches to initiating practice change, discuss two specific frameworks for implementing practice change, and provide an application to a relevant oncology practice problem. Many conceptual terms are used in this field—some interchangeably and some more commonly in different disciplines or national locations. At times, this can lead to confusion and a lack of clarity. Figure 1 provides definitions for some of the commonly encountered terminology. The field spans a broad spectrum from evaluating knowledge to implementation through evaluation. The authors specifically focus on implementation of the practice change. Implementation involves the process of putting a decision or plan into effect (Dictionary.com, n.d.).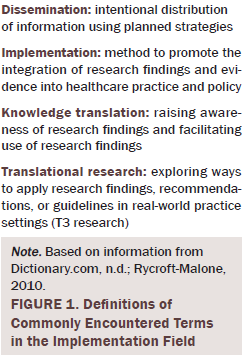
Many conceptual frameworks (or models or theories) have been identified that can be used to plan, deliver, and evaluate practice change. This plethora of models actually can make identification and selection of an appropriate model more challenging. Several reviews of models in this field have been conducted that provide guidance to individuals looking for a framework. Each review has a slightly different focus. Specifically targeting planned change, Graham and Tetrone (2007) reviewed 31 frameworks for common elements and action recommendations. This review emphasized the common elements of identifying the practice problem, adapting knowledge to the local setting, assessing barriers, selecting interventions, monitoring knowledge use, evaluating outcomes, and sustaining the practice change.
Focusing specifically on factors that enable or impede practice change, Flottorp et al. (2013) reviewed the literature and developed a comprehensive checklist of factors that determine practice. The domains of these factors included: (a) characteristics of the guideline or practice change; (b) individual professional factors; (c) patient factors; (d) professional interactions; (e) incentives and resources; (f) capacity for organizational change; and (g) social, political, and legal factors.
Examining theoretical models for the broader field of translational science, Mitchell, Fisher, Hastings, Silverman, and Wallen (2010) identified four prominent themes in their analysis of 47 models, including a theme of models focused on strategic change to promote adoption of new knowledge. Tabak, Khoong, Chambers, and Brownson (2012) reviewed 61 models in the area of dissemination and implementation research using a socioecologic framework to categorize the level for which the model was appropriate (individual, organization, community, or system). This review also identified models that were most appropriate for the implementation phase. Specifically targeting implementation frameworks, Nilsen (2015) identified three overarching goals for conceptual approaches that examine implementation: (a) process models, (b) models that seek to explain or understand implementation outcomes, and (c) evaluation frameworks.
Synthesizing across these review articles, a wide array of frameworks clearly exists, with varying levels of empirical support. All of these articles are a starting point for interested individuals to obtain an overview of frameworks in the field. Although individual approaches may vary, all models provide an organized framework to facilitate the implementation of knowledge from scientific discovery to application in real-life clinical settings. In addition, common components of all models include an identified need; data collection and analysis; a decision by stakeholders to accept, modify, or reject the evidence; implementation; and evaluation (Velasquez, McArthur, & Johnson, 2011). All of the reviewers also agree on the complexity and diversity in the field and the importance of a framework or model to guide the work. Because of a persistent gap between knowledge and practice and the lack of sustainability of many practice change initiatives, the use of a conceptual framework is advocated to critically evaluate what went right or wrong in the implementation phase.
A discussion of two frameworks is presented to provide a more detailed understanding of frameworks that are available to guide practice implementation initiatives.
Plan-Do-Study-Act Cycle
The Plan-Do-Study-Act (PDSA) cycle (Agency for Healthcare Research and Quality, 2008) is a four-step cycle advocated by the Institute for Healthcare Improvement (IHI). This process encourages (a) planning the change, including collecting data, (b) doing or implementing the change on a small scale, (c) analyzing data and results, and (d) refining the changes based on what was learned. Additional information on all aspects of this process is posted on the IHI website (www.ihi.org/resources/pages/howtoimprove/default.aspx). The process may be familiar to many nurses as a quality improvement tool. Figure 2 provides an author-developed example application of the PDSA framework to a planned practice change to implement distress screening in an oncology outpatient setting. Although not meant to be comprehensive, the figure provides some examples of specific content that fits into each step of the cycle. 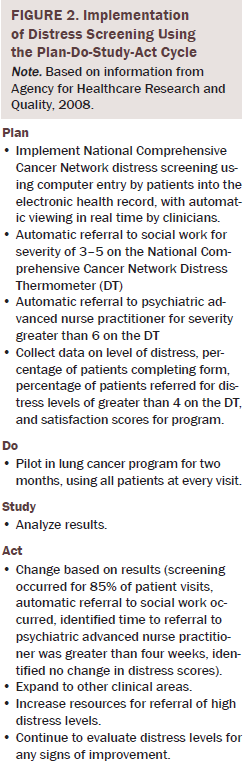
Promoting Action on Research Implementation in Health Services
The Promoting Action on Research Implementation in Health Services (PARIHS) framework was first introduced by Kitson, Harvey, and McCormack (1998), with subsequent revisions in 2002, 2004, and 2008 (Harvey et al., 2002; Kitson et al., 2008; McCormack et al., 2002; Rycroft-Malone, 2010; Rycroft-Malone et al., 2002; Rycroft-Malone, Harvey, et al., 2004; Rycroft-Malone, Seers, et al., 2004). The PARIHS model addresses the complexity of the practice environment and dynamic interrelationship among three main influences, depicted on a high–low continuum, that affect use of research findings in clinical practice: evidence, context, and facilitation (Hack, Ruether, Weir, Grenier, & Degner, 2011; Rycroft-Malone, 2010).
The underlying assumption of the PARIHS framework is that successful implementation of evidence-based practice initiatives will most likely occur when the following exist: robust scientific evidence that is concordant with professional experience and patient preferences (high evidence), a receptive setting and context with strong leadership and supportive culture (high context), and skilled facilitation to support the implementation process (high facilitation) (Rycroft-Malone, 2010). The framework also identified subelements for each core component that address the nature of evidence, contextual themes, and the process of facilitation (Hack, Carlson, et al., 2011; Rycroft-Malone, 2010).
Kitson et al. (2008) developed diagnostic and evaluative questions for each element and suggested that the framework be applied in a two-stage process in which initial diagnostic and evaluative information related to evidence and context would be used to guide facilitation efforts. Valid and reliable tools to assess organizational readiness for change and the context of implementation (Context Assessment Index) using the PARIHS framework were developed by Helfich, Yu-Fang, Sharp, and Sales (2009) and McCormack, McCarthy, Wright, Slater, and Coffey (2009), respectively. This comprehensive framework, designed to support evidence-based practice, has been used in diverse settings and can guide efforts by individual practitioners, healthcare teams, and organizations to successfully implement innovative clinical practice initiatives. Figure 3 highlights critical questions to consider when using the PARIHS framework.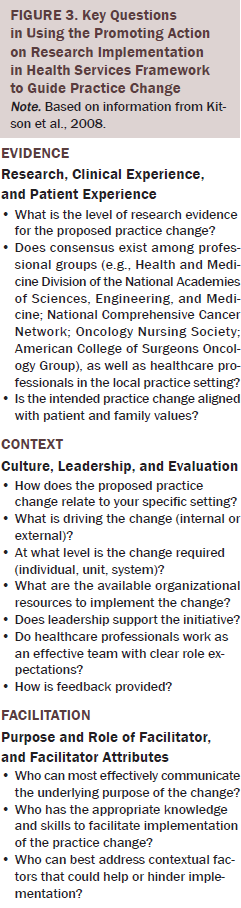
Conclusion
The field of implementation has many existing frameworks that can be used to guide practice change. The review articles that were presented are a good starting place for information for nurses unfamiliar with the field. No gold standard or single recommended approach currently exists for successful implementation. A planned approach to practice change needs to consider the full array of factors that influence implementation. Some examples of underlying conceptual issues to consider when planning practice change include the following:
• Does change occur primarily at the level of the individual? Frameworks on behavior change and classic theories on motivation and self-efficacy may provide direction.
• Does change occur as a group phenomenon? Identification of organizational commitment, early adopters, and key leaders may be helpful.
• What factors will facilitate an easy implementation? Review frameworks that examine barriers and facilitators.
• What is the appropriate setting or target for the practice change (unit, department, or organization)? Consider frameworks geared toward that specific targeted setting.
The first step in knowledge translation is examining the evidence. An excellent resource for evidence-based practice is the Oncology Nursing Society’s Putting Evidence Into Practice (PEP) resource (www.ons.org/practice-resources/pep). PEP guidelines have been developed for many commonly occurring symptoms in patients with cancer, with interventions rated for levels of effectiveness. Unfortunately, the state of the science is not as clear on how to successfully implement the new standard of care into practice.
As the need to improve healthcare systems continues, oncology nurses are poised to lead practice change initiatives. Many frameworks already have been developed and tested (many by nurses), which will assist in planning the practice change in a structured and comprehensive manner.
References
Agency for Healthcare Research and Quality. (2008). Plan-Do-Study-Act (PDSA) cycle. Retrieved from https://innovations.ahrq.gov/qualitytools/plan-do-study-act-pdsa-cycle
Dictionary.com. (n.d.). Implementation. Retrieved from http://www.dictionary.com/browse/implementation
Flottorp, S.A., Oxman, A.D., Krause, J., Musila, N.R., Wensing, M., Godycki-Cwirko, M., . . . Eccles, M.P. (2013). A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implementation Science, 8, 35. doi:10.1186/1748-5908-8-35
Graham, I.D., & Tetroe, J. (2007). Some theoretical underpinnings of knowledge translation. Academic Emergency Medicine, 14, 936–941. doi:10.1111/j.1553-2712.2007.tb02369.x
Hack, T.F., Carlson, L., Butler, L., Degner, L.F., Jakulj, F., Pickles, T., . . . Weir, L. (2011). Facilitating the implementation of empirically valid interventions in psychosocial oncology and supportive care. Supportive Care in Cancer, 19, 1097–1105. doi:10.1007/s00520-011-1159-z
Hack, T.F., Ruether, J.D., Weir, L.M., Grenier, D., & Degner, L.F. (2011). Study protocol: Addressing evidence and context to facilitate transfer and uptake of consultation recording use in oncology: A knowledge translation implementation study. Implementation Science, 6, 20. doi:10.1186/1748-5908-6-20
Harvey, G., Loftus-Hills, A., Rycroft-Malone, J., Titchen, A., Kitson, A., McCormack, B., & Seers, K. (2002). Getting evidence into practice: The role and function of facilitation. Journal of Advanced Nursing, 37, 577–588. doi:10.1046/j.1365-2648.2002.02126.x
Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: National Academies Press.
Helfich, C.D., Yu-Fang, L., Sharp, N.D., & Sales, A.E. (2009). Organizational readiness to change assessment (ORCA): Development of an instrument based on the Promoting Action on Research in Health Services (PARIHS) framework. Implementation Science, 4, 38. doi:10.1186/1748-5908-4-38
Kitson, A., Harvey, G., & McCormack, B. (1998). Enabling the implementation of evidence based practice: A conceptual framework. Quality in Health Care, 7, 149–158. doi:10.1136/qshc.7.3.149
Kitson, A.L., Rycroft-Malone, J., Harvey, G., McCormack, B., Seers, K., & Titchen, A. (2008). Evaluating the successful implementation of evidence into practice using the PARIHS framework: Theoretical and practical challenges. Implementation Science, 3, 1. doi:10.1186/1748-5908-3-1
McCormack, B., Kitson, A., Harvey, G., Rycroft-Malone, J., Titchen, A., & Seers, K. (2002). Getting evidence into practice: The meaning of ‘context’. Journal of Advanced Nursing, 38, 94–104. doi:10.1046/j.1365-2648.2002.02150.x
McCormack, B., McCarthy, G., Wright, J., Slater, P., & Coffey, A. (2009). Development and testing of the Context Assessment Index (CAI). Worldviews on Evidence-Based Nursing, 6, 27–35.
Mitchell, S.A., Fisher, C.A., Hastings, C.E., Silverman, L.B., & Wallen, G.R. (2010). A thematic analysis of theoretical models for translational science in nursing: Mapping the field. Nursing Outlook, 58, 287–300. doi:10.1016/j.outlook.2010.07.001
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10, 53. doi:10.1186/s13012-015-0242-0
Rycroft-Malone, J. (2010). Promoting action on research implementation in health services (PARIHS). In J. Rycroft-Malone & T. Bucknall (Eds.), Models and frameworks for implementing evidence-based practice: Linking evidence to action (pp. 109–135). Malden, MA: Wiley-Blackwell.
Rycroft-Malone, J., Harvey, G., Seers, K., Kitson, A., McCormack, B., & Titchen, A. (2004). An exploration of the factors that influence the implementation of evidence into practice. Journal of Clinical Nursing, 13, 913–924. doi:10.1111/j.1365-2702.2004.01007.x
Rycroft-Malone, J., Kitson, A., Harvey, G., McCormack, B., Seers, K., Titchen, A., & Estabrooks, C.A. (2002). Ingredients for change: Revisiting a conceptual framework. Quality and Safety in Health Care, 11, 174–180. doi:10.1136/qhc.11.2.174
Rycroft-Malone, J., Seers, K., Titchen, A., Harvey, G., Kitson, A., & McCormack, B. (2004). What counts as evidence in evidence-based practice? Journal of Advanced Nursing, 47, 81–90. doi:10.1111/j.1365-2648.2004.03068.x
Tabak, R., Khoong, E.C., Chambers, D.A., & Brownson, R.C. (2012). Bridging research and practice: Models for dissemination and implementation research. American Journal of Preventive Medicine, 43, 337–350. doi:10.1016/j.amepre.2012.05.024
Velasquez, D.M., McArthur, D.B., & Johnson, C. (2011). Doctoral nursing roles in knowledge generation. In P.G. Reed & N.B. Crawford Shearer (Eds.), Nursing knowledge and theory innovation: Advancing the science of practice (pp. 37–50). New York, NY: Springer.
About the Author(s)
Flannery is a research assistant professor and Rotondo is the interim associate dean for Education and Student Affairs, the director of the Doctor of Nursing Practice Program, and an assistant professor, both in the School of Nursing at the University of Rochester Medical Center in New York.No financial relationships to disclose. Flannery can be reached at marie_flannery@urmc.rochester.edu, with copy to editor at ONFEditor@ons.org.

