Beliefs in Chemotherapy and Knowledge of Cancer and Treatment Among African American Women With Newly Diagnosed Breast Cancer
Purpose/Objectives: To examine beliefs regarding the necessity of chemotherapy and knowledge of breast cancer and its treatment in African American women with newly diagnosed breast cancer, and to explore factors associated with women’s beliefs and knowledge.
Design: Descriptive, cross-sectional study.
Setting: Six urban cancer centers in Western Pennsylvania and Eastern Ohio.
Sample: 101 African American women with newly diagnosed breast cancer.
Methods: Secondary analysis using baseline data collected from participants in a randomized, controlled trial at their first medical oncology visit before the first cycle of chemotherapy.
Main Research Variables: Belief in chemotherapy, knowledge of cancer and recommended treatment, self-efficacy, healthcare system distrust, interpersonal processes of care, symptom distress, and quality of life.
Findings: African American women endorsed the necessity of chemotherapy. Most women did not know their tumor size, hormone receptors, specific therapy, or why chemotherapy was recommended to them. Women who perceived better interpersonal communication with physicians, less self-efficacy, or were less involved in their own treatment decision making held stronger beliefs about the necessity of chemotherapy. Women without financial difficulty or having stronger social functioning had more knowledge of their cancer and recommended chemotherapy.
Conclusions: African American women with newly diagnosed breast cancer generally agreed with the necessity of chemotherapy. Knowledge of breast cancer, treatment, and risk reduction through adjuvant therapy was limited.
Implications for Nursing: Oncology nurses could help advocate for tailored educational programs to support informed decision making regarding chemotherapy acceptance for African American women.
Jump to a section
Breast cancer is the most common cancer among American women and the second-leading cause of cancer death in the United States (American Cancer Society, 2015). Although survival is improving for all women with breast cancer, African American women with newly diagnosed breast cancer have overall lower five-year survival rates (78%) than Caucasian women (90%) (National Cancer Institute, 2014). Biologic differences do not explain all racial variation in breast cancer survival (Danforth, 2013; Martin et al., 2009). Historically, explanations for such disparities in survivorship include late-stage presentation in African American women related to poor adherence to breast cancer screening (Fedewa et al., 2011; Tariq, Latif, Zaiden, Jasani, & Rana, 2013). In addition, some social, economic, and cultural barriers to screening and treatment, such as social injustice, poverty, and a general mistrust of the healthcare system, may disproportionately affect African American women (Gerend & Pai, 2008).
Evidence shows that systemic chemotherapy and hormonal therapy improve survival after a diagnosis of breast cancer (Early Breast Cancer Trialists’ Collaborative, 2005; Peto et al., 2012). However, African American women are more likely to discontinue the treatment early or have treatment delays as compared to Caucasian women (Fedewa, Ward, Stewart, & Edge, 2010; Hershman et al., 2009). Previous studies (Martin et al., 2014; Nurgalieva et al., 2013; Sheppard et al., 2013) have explored factors associated with chemotherapy treatment delays and early treatment cessation and indicated that the patient–physician relationship and patients’ spiritual beliefs may be associated with treatment disparities (Sheppard et al., 2013) in addition to other factors, such as age; marital status; insurance coverage (Jansen, Otten, & Stiggelbout, 2006; Jorgensen, Young, & Solomon, 2013); cognitive, emotional, and social network variables (Magai, Consedine, Adjei, Hershman, & Neugut, 2008); and disease- or treatment-associated factors. Research also suggests that additional unknown sociocultural factors may influence treatment disparities (Nurgalieva et al., 2013).
Distinctive attitudes, perceptions, and stressors may affect breast cancer treatment adherence among African American women (Allicock, Graves, Gray, & Troester, 2013; Jansen et al., 2006; Jassem et al., 2013; Johnson, Elbert-Avila, & Tulsky, 2005; Thune-Boyle, Myers, & Newman, 2006). Medication nonadherence can be a reasoned decision for patients when they perceive limited benefits about the medication. Leventhal’s well-known self-regulatory theory suggests that patients are more likely to adhere to a prescribed medication regimen if they believe that the regimen makes common sense in the context of health beliefs and the likelihood of benefit (Leventhal, Meyer, & Nerenz, 1980). To ensure that consent for chemotherapy in African American women with newly diagnosed breast cancer is informed, it is necessary to explore and understand their perceptions regarding the necessity of chemotherapy.
Knowledge about cancer, treatment, and likely treatment outcomes is critically important for decision making regarding adherence to prescribed therapy (Sadler et al., 2007). African Americans traditionally are less active in seeking generic health information than other ethnic groups (Matthews, Sellergren, Manfredi, & Williams, 2002). In general, they have less knowledge about their bodies and lack awareness about cancer prevention (Ashing-Giwa et al., 2004). In a survey of women with breast cancer, African American women were found to be less likely than Caucasian women to correctly answer questions about their tumor characteristics, including stage and receptor status (Freedman, Kouri, West, & Keating, 2015). African Americans report a preference for cancer information tailored to individual risk (Darnell, Chang, & Calhoun, 2006) and health communication to be personally relevant and culturally appropriate (Allicock et al., 2013). How best to address the preferences for communication and education in African American patients with cancer requires a great deal of attention from healthcare providers. In addition, because of the disproportionate number of African Americans living at or below poverty levels, African Americans may have lower levels of health literacy than Caucasians and are less likely to question physicians (Gordon, Street, Sharf, & Souchek, 2006; Rust & Davis, 2011; Shea et al., 2004), limiting the amount of information they receive (Skalla, Bakitas, Furstenberg, Ahles, & Henderson, 2004). Breast cancer treatment is increasingly tailored and complex. Options for individual patients with breast cancer may differ from those of other patients based on the person’s tumor pathology (Olopade, Grushko, Nanda, & Huo, 2008), tumor subtype, treatment options, and associated treatment effects, making these discussions even more challenging (Nehls et al., 2013). Because the information is critically important for an informed decision, clinicians must understand the risk factors for lack of understanding among all women, work to increase clarity and relevance in information presentation, and subsequently improve patient understanding (Royak-Schaler et al., 2008). The healthcare system in general and individual providers may also play a role in influencing understanding (Lennes, Temel, Hoedt, Meilleur, & Lamont, 2013; Matthews et al., 2002). Few studies have specifically reported on African American women’s knowledge of cancer pathology and treatment effects (Ashing-Giwa et al., 2004; Hofman et al., 2004).
The purpose of the current study was to examine beliefs regarding the necessity of chemotherapy in African American women with newly diagnosed breast cancer, as well as their knowledge of their cancer pathology, the treatment recommended to them, and likely treatment outcomes. In addition, factors associated with African American women’s beliefs in chemotherapy and knowledge were also explored. It was expected that belief in chemotherapy was associated with physician communication and perceived relationship to the healthcare system. An additional hypothesis was that knowledge of cancer and recommended treatment was associated with sociodemographics, such as age, education, income, and communication with physicians. Findings from this study are expected to guide development of tailored interventions for African American women to improve patient counseling regarding understanding of chemotherapy recommendations.
Methods
This study was a secondary analysis using baseline data from 101 African American women who participated in a parent study at six urban cancer centers in Western Pennsylvania and Eastern Ohio. The parent study was a nonblinded, repeated-measures, intent-to-treat randomized, controlled trial comparing the efficacy of a psychoeducational intervention with that of usual care on percentage of prescribed dose of breast cancer chemotherapy received (Rosenzweig et al., 2011). Preliminary findings of the parent study revealed that the psychoeducational group demonstrated more rapid initiation of chemotherapy and better overall adherence to chemotherapy (Rosenzweig et al., 2011).
Sample
Participants in the study were African American women from southwestern Pennsylvania and eastern Ohio newly diagnosed with breast cancer. Informed consent was signed by all participants after the physician confirmed that chemotherapy was recommended. Inclusion criteria were (a) being African American, as determined by patient self-report, (b) aged 18 years or older, (c) being diagnosed with invasive breast cancer, (d) being of female gender, and (e) being recommended for chemotherapy. Exclusion criteria were (a) impaired cognition, as determined by clinician performing the initial history and physical examination, (b) inability to read and understand English, and (c) receiving hormonal therapy alone. Baseline data were collected before first therapy at the patient’s first visit to medical oncology or at a subsequent visit for prechemotherapy testing within one week of recommendation. Standard chemotherapy teaching about chemotherapy toxicity and potential side effects was completed by the RN in the clinic after the chemotherapy recommendation was made. Chemotherapy teaching did not include why the recommendation for chemotherapy was made. Questions to the nurse about the need for chemotherapy were referred back to the physician, per clinic policy.
Measures
Baseline questionnaires were administered by the research staff in a private conference room adjacent to the clinic area, free of distraction. It took about 40 minutes to complete all questionnaires.
Belief in chemotherapy: Belief in the necessity of chemotherapy was assessed using a subscale adapted with permission from the Beliefs about Medicines Questionnaire (BMQ). The subscale consisted of six items assessing African American women’s beliefs about the necessity of chemotherapy, such as “Chemotherapy is effective,” and “My health, at present, depends on chemotherapy.” Respondents indicated their degree of agreement with each statement on a five-point Likert-type scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Scores for this subscale could range from 6–36. Higher scores indicated stronger beliefs in the necessity of chemotherapy. A Cronbach alpha of 0.86 was reported for the necessity scale of the original BMQ (Horne, Weinman, & Hankins, 1999).
Understanding of tumor and treatment: The Tumor and Treatment Knowledge Assessment is an investigator-created questionnaire and is deliberately brief because of the researcher’s reluctance to “test” patients in a clinical setting. Six questions, including size of tumor(s), lymph node status, status of hormone receptors, HER2 status, the name of specific therapy, and the reason that the chemotherapy recommendation was made, were asked in a conversational manner. The accuracy of the responses was then determined by study personnel against the medical record.
Demographic and medical variables: Sociodemographic variables included age, income, years of education, employment, insurance status, and spiritual beliefs. Clinical variables included comorbidities, previous medical history, current medications, current cancer treatment, and course of illness. Both were measured by the standard demographic and medical variable questionnaires from the University of Pittsburgh School of Nursing in Pennsylvania.
Health beliefs and distrust: The Health Care System Distrust Scale was constructed to measure a patient’s perceptions of the healthcare system. This 10-item, five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree) measures patient’s perceptions of healthcare honesty (four items), confidentiality (two items), competence (two items), and fidelity (two items) (Rose, Peters, Shea, & Armstrong, 2004). Higher scores indicate stronger healthcare system distrust. The internal consistency of the scale was 0.75 in a sample population with 43% African Americans and 45% Caucasians (Rose et al., 2004).
Communication satisfaction: The Medical Effectiveness Research Center Interpersonal Processes of Care (MERC IPC) questionnaire is a 29-item measure to assess interpersonal processes of care from the perspective of diverse racial/ethnic groups into a framework for investigating how processes of communication, decision making, and interpersonal style might account for observed ethnic and socioeconomic differences in health care (Stewart, Napoles-Springer, & Perez-Stable, 1999). For each item, respondents were asked how often that type of care had been provided during the past 12 months using a five-point scale (1 = always, 2 = often, 3 = sometimes, 4 = rarely, 5 = never). An example of a question from the communication subscale is, “How often did doctors speak too fast?” Other example questions include, “How often did you and your doctors work out a treatment plan together?”for the decision-making subscale and, “How often were doctors concerned about your feelings?” for the interpersonal style subscale. Higher subscale scores indicate better perception of the process of care. The instrument was validated with internal consistency reliability ranging from 0.64–0.93 in ethnically diverse populations (Stewart et al., 1999; Wong, Korenbrot, & Stewart, 2004).
Self-efficacy: The General Self-Efficacy Scale (GSE) is a 10-item scale with a score for each question ranging from 1 (“not at all true”) to 4 (“exactly true”) assessing optimistic self-beliefs used to cope with a variety of demands in life (Schwarzer & Jerusalem, 1995). Higher scores indicate stronger patient belief in self-efficacy. Several studies have shown that the GSE has high reliability, stability, and construct validity (Bosscher & Smit, 1998; Luszczynska, Scholz, & Schwarzer, 2005).
Quality of life: The Functional Assessment of Cancer Therapy is a 27-item Likert-type self-report questionnaire yielding four subscales (physical well-being, social well-being, functional well-being, and emotional well-being) measuring health-related quality of life for patients with cancer (Brady et al., 1997; Cella et al., 1993). Each item is rated on a scale from 0 (not at all) to 4 (very much). This questionnaire has been determined to be appropriate for use in clinical oncology settings and shown to have good validity and reliability, with a Cronbach alpha of 0.89 for the total scale and 0.69–0.82 for the subscales (Cella et al., 1993).
Symptom distress: The McCorkle Symptom Distress Scale (SDS) was developed based on interviews with patients about their symptom experiences, with scores ranging from 1–5 on a Likert-type scale, with 5 indicating most severe (McCorkle & Quint-Benoliel, 1983). Total symptom distress can be obtained as the unweighted sum of 13 items. A cumulative score greater than 33 indicates severe distress, necessitating immediate intervention. Psychometric testing among patients with cancer using the SDS revealed high reliability with a Cronbach alpha of 0.97 (McCorkle & Quint-Benoliel, 1983).
Data Management and Analysis
Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Pittsburgh (Harris et al., 2009). Data analysis was conducted using SPSS®, version 22.0. Descriptive statistics were used to describe the sample sociodemographics and summarize participants’ beliefs in chemotherapy and knowledge of cancer and treatment. For continuous variables, means and SDs were calculated. Categorical variables were described using frequencies and percentages. Correlation analyses, Mann–Whitney U tests, and multiple linear regression were used to assess relationships of sociodemographics, health system distrust, communication satisfaction, self-efficacy, quality of life, and symptom distress with beliefs in chemotherapy and knowledge of tumor and treatment. Both bivariate analysis results (significance level of p < 0.25) and literature reports were considered for selection of potential predictors in regression models (significance level of p < 0.05).
Results
The sample for this secondary analysis included 101 African American women with newly diagnosed breast cancer. Table 1 summarizes the personal characteristics of women in this study.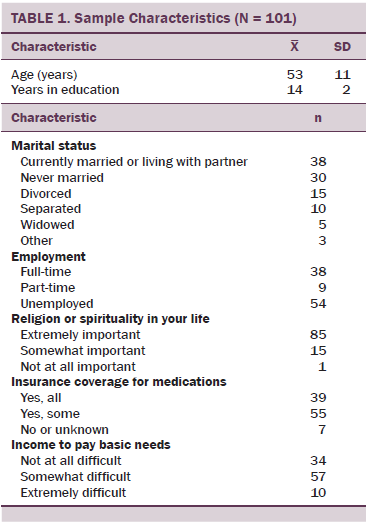
Beliefs in Chemotherapy
Prior to chemotherapy, African American women with newly diagnosed breast cancer had a mean score of 21.8 (SD = 4.6, range = 6–36) regarding their beliefs about the necessity of chemotherapy. Most women agreed or strongly agreed that their health depended on chemotherapy (n = 79), chemotherapy protected them from getting worse (n = 74), and chemotherapy was effective (n = 66) (see Table 2).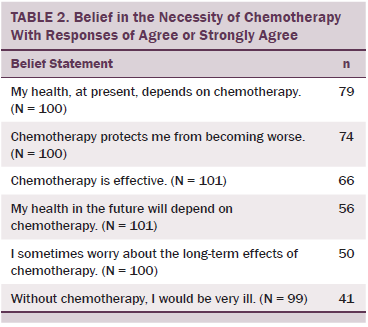
Bivariate correlation analyses demonstrated that women’s stronger beliefs about the necessity of chemotherapy medication were significantly associated with less distrust in the healthcare system (r = –0.217, p = 0.03), better interpersonal communication with physicians (r = 0.301, p = 0.002), and better interpersonal style of care experience with physicians (such as being respected, not discriminated against, and being emotionally supported) (r = 0.201, p = 0.045). Women’s sociodemographic characteristics were not found to be associated with their beliefs in necessity of chemotherapy. Women who had perceived economic distress (some or extreme difficulty to pay for basic needs) tended to believe more in necessity of chemotherapy than women of higher income, but the difference was marginally significant (p = 0.081).
The multiple linear regression model included age, income, self-efficacy, social support, health system distrust, interpersonal processes of care (communication, decision making, and interpersonal style), symptom distress, and knowledge of tumor and treatment. These variables significantly predicted the necessity of chemotherapy (F[10, 84] = 2.659, p = 0.007, R2 = 0.24). After controlling for the other variables in the model, women who perceived receiving better interpersonal communication with their physician had greater beliefs in necessity of chemotherapy (b = 0.057, p = 0.007); woman with higher self-efficacy (b = –0.159, p = 0.044) and women who were more involved in their own treatment decision making (b = –0.079, p = 0.02) had fewer beliefs in the necessity of chemotherapy (see Table 3).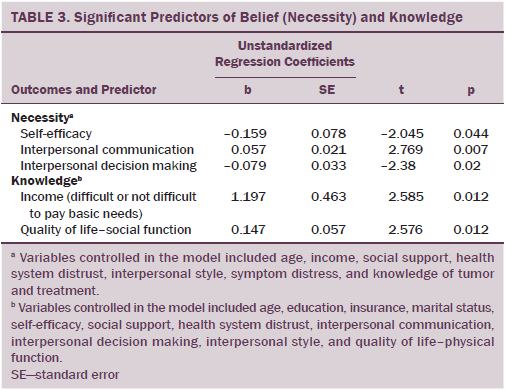
Knowledge of Tumor and Chemotherapy
More than half of African American women with newly diagnosed breast cancer did not know the size of their tumor (n = 57), the status of their hormone receptors (n = 65), the name of their specific recommended therapy (n = 66), or why chemotherapy was recommended to them (n = 80) (see Table 4). Higher knowledge of tumor and recommended chemotherapy was found to be significantly associated with higher quality of social function (r = 0.213, p = 0.034), some or all coverage of medication by insurance (U = 166, p = 0.027), and having no difficulty paying for basic needs by income (U = 773.5, p = 0.008). The multiple linear regression model includes sociodemographics (age, education, income, insurance, and marital status), self-efficacy, social support, health system distrust, interpersonal processes of care, and quality of life (physical and social function), which significantly predicted knowledge of tumor and chemotherapy (F[12, 81] = 2.634, p = 0.005, R2 = 0.281). After controlling for the other variables in the model, income and quality of social function significantly predicted that women with no difficulty at all paying for basic needs (b = 1.197, p = 0.012) and women having better social function (b = 0.147, p = 0.012) had more knowledge of their tumor and recommended chemotherapy.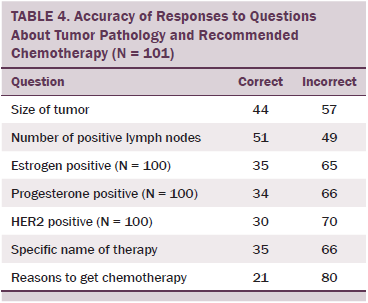
Discussion
African American women with newly diagnosed breast cancer believed that chemotherapy was necessary. However, they lacked knowledge about their disease and why chemotherapy was recommended to them. Lack of knowledge about breast cancer among minority women is supported by previous studies (Ashing-Giwa et al., 2004; Freedman et al., 2015). In particular, gaps were found in information provided from physicians to African American women with breast cancer about treatment, side effects, and follow-up care, including long-term effects of their treatment (Royak-Schaler et al., 2008). Lack of understanding of treatment recommendations can increase patients’ concerns and may affect their decision making about treatment (Cowley, Heyman, Stanton, & Milner, 2000). To improve patients’ understanding of information about the treatment goal, long-term effects, and side effects of the treatment, clinicians may need to be more culturally competent in communication and integrate appropriate communication skills when providing patient education and support (Nehls et al., 2013). The role of lay or professional navigators may mitigate communication difficulties between clinicians and patients in breast cancer care (Robinson-White, Conroy, Slavish, & Rosenzweig, 2010).
The current study also found that African American women’s beliefs in the necessity of chemotherapy were highly associated with their relationship with the healthcare system, particularly their trust in hospital care and their communication with healthcare providers. Women reporting poor relationships with the healthcare system and their physicians are expected to have less belief in the necessity of chemotherapy. This finding is consistent with previous studies that suggest that physician trust and patient–physician communication were critically important factors for patients with cancer in deciding whether to accept chemotherapy (Jorgensen et al., 2013; Kreling, Figueiredo, Sheppard, & Mandelblatt, 2006). Medical mistrust and less physician communication were found to be common among minority patients with cancer (Bergamo et al., 2013; Kreling et al., 2006). African American patients reported fewer encounters with physicians, asked fewer questions, and received less information about cancer treatment than Caucasian patients (Baldwin et al., 2005; Gordon et al., 2006). In this current study, a high percentage of women reported misunderstanding of cancer and recommended treatment, indicating possible ineffective patient–physician communication.
Greater self-efficacy and perceived shared decision making can increase the sense of control and engagement in health care (Andersen, Bowen, Morea, Stein, & Baker, 2009; Jones et al., 2010). However, both factors were found in the current analysis to significantly predict less belief on the part of the patient in the necessity of chemotherapy. It is possible that women feel confident that other options are available to treat breast cancer. It also is possible that a confidence in the ability to engage in one’s own health care, coupled with a lack of understanding of tumor, treatment, and potential benefit of adjuvant chemotherapy, encourages a woman to challenge the belief that chemotherapy is of benefit or the only option. Therefore, healthcare providers should combine efforts at improving healthcare empowerment with concrete, understandable information about the importance of chemotherapy within the context of the individual presenting with breast cancer. Jansen et al. (2006) reported that women who preferred less involvement in decision making were more likely to perceive that they had no choice and accepted recommended treatment (such as adjuvant chemotherapy). An additional concern with women who believe they have no choice is that they may follow the treatment recommendation and start chemotherapy but, when they begin to experience side effects and do not communicate this information to physicians, continuous adherence and persistence to chemotherapy can be difficult (Chawla & Arora, 2013).
Because of a lack of information and understanding of cancer and treatment effects, patients with cancer can heavily rely on their physician to make treatment decisions for them (Arora & McHorney, 2000; Seror et al., 2013; Sheppard et al., 2010). Therefore, if a woman feels that she can engage and make good healthcare decisions, she may not accept all treatment recommendations passively. The role of the clinician then is to offer the reasons why adjuvant chemotherapy is potentially lifesaving in an educationally accessible manner. If physicians lack communication skills or the time for this engagement, alternative educators should be routinely integrated into practice.
Previous studies reported that the age of the patient might be associated with the belief and acceptance of chemotherapy (Jorgensen et al., 2013; Lennes et al., 2013; Martin et al., 2014; Morimoto, Coalson, Mowat, & O’Malley, 2010; Ziner et al., 2012). However, this was not confirmed in the current study, likely because this study included participants who were relatively young. Spirituality is important for African American women coping with breast cancer (Johnson et al., 2005; Yoo, Levine, & Pasick, 2014). Spirituality was not found to be associated with women’s beliefs in chemotherapy in the current study, but the majority of women rated spirituality as being extremely important. Lack of variation in their rating could be the reason for nonsignificance.
Knowledge and cancer fatalism play an important role in the patient’s decision to start chemotherapy (Holmes, 2012). In the current study, income and social well-being were found to significantly predict African American women’s knowledge of cancer pathology and recommended treatment. This finding is not surprising and is consistent with previous reports that knowledge deficits about chemotherapy were more prevalent among lower-income women (Lee et al., 2012). Lee et al. (2012) also demonstrated that higher knowledge was significantly associated with physician’s discussion of chemotherapy, which implies that effective communication with physicians may be a key factor in chemotherapy acceptance. However, interpersonal communication in the current study was not found to be associated with women’s knowledge, which may be because interpersonal communication was measured by the manner of communication, such as whether the doctor talks too fast, whether the doctor uses medical jargon, or how often the doctor cares about the patient’s concerns. The measure did not actually assess how the patient understood the information delivered. Patient-centered communication should ensure not only that adequate information is delivered to the patient, but also that the patient fully understands what she may want to know regarding her newly diagnosed illness (Mazor et al., 2013).
African American women’s social function also is an important predictor of knowledge gained about cancer and treatment. Social support affects African American women seeking medical care and adherence to treatment (Fowler, 2007; Paschal, Ablah, Wetta-Hall, Molgaard, & Liow, 2005). Women with stronger social support are more likely to actively seek health information, such as information from the Internet (Guillory et al., 2014), from their social networks, or from participating in support programs (Kent et al., 2013). After their diagnosis, African American women with breast cancer may experience a decline in social support (Thompson, Rodebaugh, Perez, Schootman, & Jeffe, 2013). They are less likely than other groups of women to use healthcare services and may rely more frequently on informal sources of support, such as family members and/or social support networks (Copeland, Scholle, & Binko, 2003). Social networking and interaction may help women better communicate with their healthcare providers, enhancing their ability to obtain accurate cancer and treatment knowledge.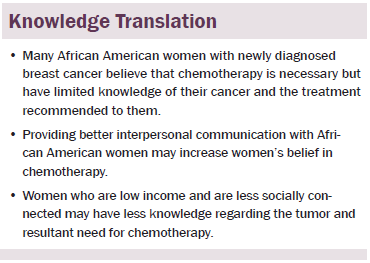
Limitations
A few limitations can be identified in the current study. Questionnaires were completed by African American women who came to the clinic for chemotherapy consultation based on surgical referral. Women who decided not to come to the clinic were not able to be included. Therefore, it is possible that the current study excluded African American women who are at high risk for nonadherence to cancer treatment, which may cause sampling bias and affect the generalization of the findings. In addition, as a secondary analysis, only baseline factors from the questionnaires were included in regression models. Finally, because only African American women with newly diagnosed breast cancer were included in the study, comparison to a Caucasian population was not done but would be of interest.
Conclusion
African American women with newly diagnosed breast cancer and recommended for chemotherapy believe that chemotherapy is necessary. African American women with better communication with their healthcare providers and less involvement in treatment decision making are expected to have stronger beliefs regarding the necessity of chemotherapy. Low income and low socially connected African American women have less knowledge regarding their tumors and resultant needs for chemotherapy.
A foundational element of informed consent is the provision of information to make the consent truly informed. The information must be provided in accordance with the patient’s ability to understand the information and in a manner that the patient finds the information to be necessary. Findings from this study may help design targeted interventions to better guide clinicians in providing information to aid in the decisions regarding chemotherapy. Interventions to improve understanding of tumor and treatment among minority patients are necessary to ensure informed consent for all women.
References
Allicock, M., Graves, N., Gray, K., & Troester, M.A. (2013). African American women’s perspectives on breast cancer: Implications for communicating risk of basal-like breast cancer. Journal of Health Care for the Poor and Underserved, 24, 753–767. doi:10.1353/hpu.2013.0082
American Cancer Society. (2015). Cancer facts and figures, 2015. Retrieved from http://www.cancer.org/acs/groups/content/@editorial/documents/document/…
Andersen, M.R., Bowen, D.J., Morea, J., Stein, K.D., & Baker, F. (2009). Involvement in decision-making and breast cancer survivor quality of life. Health Psychology, 28, 29–37. doi:10.1037/0278-6133.28.1.29
Arora, N.K., & McHorney, C.A. (2000). Patient preferences for medical decision making: Who really wants to participate? Medical Care, 38, 335–341.
Ashing-Giwa, K.T., Padilla, G., Tejero, J., Kraemer, J., Wright, K., Coscarelli, A., . . . Hills, D. (2004). Understanding the breast cancer experience of women: A qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology, 13, 408–428. doi:10.1002/pon.750
Baldwin, L.M., Dobie, S.A., Billingsley, K., Cai, Y., Wright, G.E., Dominitz, J.A., . . . Taplin, S.H. (2005). Explaining Black-White differences in receipt of recommended colon cancer treatment. Journal of National Cancer Institute, 97, 1211–1220.
Bergamo, C., Lin, J.J., Smith, C., Lurslurchachai, L., Halm, E.A., Powell, C.A., . . . Wisnivesky, J.P. (2013). Evaluating beliefs associated with late-stage lung cancer presentation in minorities. Journal of Thoracic Oncology, 8, 12–18. doi:10.1097/JTO.0b013e3182762ce4
Bosscher, R.J., & Smit, J.H. (1998). Confirmatory factor analysis of the General Self-Efficacy Scale. Behavior Research and Therapy, 36, 339–343.
Brady, M.J., Cella, D.F., Mo, F., Bonomi, A.E., Tulsky, D.S., Lloyd, S.R., . . . Shiomoto, G. (1997). Reliability and validity of the Functional Assessment of Cancer Therapy–Breast quality-of-life instrument. Journal of Clinical Oncology, 15, 974–986.
Cella, D.F., Tulsky, D.S., Gray, G., Sarafian, B., Linn, E., & Bonomi, A. (1993). The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 570–579.
Chawla, N., & Arora, N.K. (2013). Why do some patients prefer to leave decisions up to the doctor: Lack of self-efficacy or a matter of trust? Journal of Cancer Survivorship, 7, 592–601. doi:10.1007/s11764-013-0298-2
Copeland, V.C., Scholle, S.H., & Binko, J.A. (2003). Patient satisfaction: African American women’s views of the patient-doctor relationship. Journal of Health and Social Policy, 17, 35–48. doi:10.1300/J045v17n02_02
Cowley, L., Heyman, B., Stanton, M., & Milner, S.J. (2000). How women receiving adjuvant chemotherapy for breast cancer cope with their treatment: A risk management perspective. Journal of Advanced Nursing, 31, 314–321.
Danforth, D.N., Jr. (2013). Disparities in breast cancer outcomes between Caucasian and African American women: A model for describing the relationship of biological and nonbiological factors. Breast Cancer Research, 15, 208. doi:10.1186/bcr3429
Darnell, J.S., Chang, C.H., & Calhoun, E.A. (2006). Knowledge about breast cancer and participation in a faith-based breast cancer program and other predictors of mammography screening among African American women and Latinas. Health Promotion Practice, 7(3, Suppl.), 201S–212S. doi:10.1177/1524839906288693
Early Breast Cancer Trialists’ Collaborative. (2005). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet, 365, 1687–1717. doi:10.1016/S0140-6736(05)66544-0
Fedewa, S.A., Edge, S.B., Stewart, A.K., Halpern, M.T., Marlow, N.M., & Ward, E.M. (2011). Race and ethnicity are associated with delays in breast cancer treatment (2003–2006). Journal of Health Care for the Poor and Underserved, 22, 128–141. doi:10.1353/hpu.2011.0006
Fedewa, S.A., Ward, E.M., Stewart, A.K., & Edge, S.B. (2010). Delays in adjuvant chemotherapy treatment among patients with breast cancer are more likely in African American and Hispanic populations: A national cohort study 2004–2006. Journal of Clinical Oncology, 28, 4135–4141. doi:10.1200/jco.2009.27.2427
Fowler, B.A. (2007). The influence of social support relationships on mammography screening in African-American women. Journal of National Black Nurses Association, 18, 21–29.
Freedman, R.A., Kouri, E.M., West, D.W., & Keating, N.L. (2015). Racial/ethnic disparities in knowledge about one’s breast cancer characteristics. Cancer, 121, 724–732.
Gerend, M.A., & Pai, M. (2008). Social determinants of Black-White disparities in breast cancer mortality: A review. Cancer Epidemiology, Biomarkers and Prevention, 17, 2913–2923. doi:10.1158/ 1055-9965.EPI-07-0633
Gordon, H.S., Street, R.L., Jr., Sharf, B.F., & Souchek, J. (2006). Racial differences in doctors’ information-giving and patients’ participation. Cancer, 107, 1313–1320. doi:10.1002/cncr.22122
Guillory, J., Niederdeppe, J., Kim, H., Pollak, J.P., Graham, M., Olson, C., & Gay, G. (2014). Does social support predict pregnant mothers’ information seeking behaviors on an educational website? Maternal and Child Health Journal, 18, 2218–2225. doi:10.1007/s10995-014-1471-6
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatcis, 42, 377–381.
Hershman, D.L., Unger, J.M., Barlow, W.E., Hutchins, L.F., Martino, S., Osborne, C.K., . . . Albain, K.S. (2009). Treatment quality and outcomes of African American versus white breast cancer patients: Retrospective analysis of Southwest Oncology studies S8814/S8897. Journal of Clinical Oncology, 27, 2157–2162.
Hofman, M., Morrow, G.R., Roscoe, J.A., Hickok, J.T., Mustian, K.M., Moore, D.F., . . . Fitch, T.R. (2004). Cancer patients’ expectations of experiencing treatment-related side effects: A University of Rochester Cancer Center–Community Clinical Oncology Program study of 938 patients from community practices. Cancer, 101, 851–857. doi:10.1002/cncr.20423
Holmes, J.S. (2012). Chemotherapy adherence decision making in early stage breast cancer (Unpublished doctoral dissertation). Retrieved from http://search.proquest.com/docview/1037346372
Horne, R., Weinman, J., & Hankins, M. (1999). The Beliefs about Medicines Questionnaire (BMQ): The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health, 14, 1–24.
Jansen, S.J., Otten, W., & Stiggelbout, A.M. (2006). Factors affecting patients’ perceptions of choice regarding adjuvant chemotherapy for breast cancer. Breast Cancer Research and Treatment, 99, 35–45. doi:10.1007/s10549-006-9178-z
Jassem, J., Ozmen, V., Bacanu, F., Drobniene, M., Eglitis, J., Lakshmaiah, K.C., . . . Zaborek, P. (2013). Delays in diagnosis and treatment of breast cancer: A multinational analysis. European Journal of Public Health, 24, 761–767. doi:10.1093/eurpub/ckt131
Johnson, K.S., Elbert-Avila, K.I., & Tulsky, J.A. (2005). The influence of spiritual beliefs and practices on the treatment preferences of African Americans: A review of the literature. Journal of American Geriatrics Society, 53, 711–719. doi:10.1111/j.1532-5415.2005.53224.x
Jones, J.M., Cheng, T., Jackman, M., Rodin, G., Walton, T., & Catton, P. (2010). Self-efficacy, perceived preparedness, and psychological distress in women completing primary treatment for breast cancer. Journal of Psychosocial Oncology, 28, 269–290. doi:10.1080/07347331003678352
Jorgensen, M.L., Young, J.M., & Solomon, M.J. (2013). Adjuvant chemotherapy for colorectal cancer: Age differences in factors influencing patients’ treatment decisions. Patient Preference and Adherence, 7, 827–834. doi:10.2147/ppa.s50970
Kent, E.E., Alfano, C.M., Smith, A.W., Bernstein, L., McTiernan, A., Baumgartner, K.B., & Ballard-Barbash, R. (2013). The roles of support seeking and race/ethnicity in posttraumatic growth among breast cancer survivors. Journal of Psychosocial Oncology, 31, 393–412. doi:10.1080/07347332.2013.798759
Kreling, B., Figueiredo, M.I., Sheppard, V.L., & Mandelblatt, J.S. (2006). A qualitative study of factors affecting chemotherapy use in older women with breast cancer: Barriers, promoters, and implications for intervention. Psycho-Oncology, 15, 1065–1076. doi:10.1002/pon.1042
Lee, C., Belkora, J., Wetschler, M., Chang, Y., Moy, B., Partridge, A., & Sepucha, K. (2012). The quality of decisions about adjuvant chemotherapy for early stage breast cancer. Cancer Research. Retrieved from http://cancerres.aacrjournals.org/content/69/24_Supplement/2083
Lennes, I.T., Temel, J.S., Hoedt, C., Meilleur, A., & Lamont, E.B. (2013). Predictors of newly diagnosed cancer patients’ understanding of the goals of their care at initiation of chemotherapy. Cancer, 119, 691–699. doi:10.1002/cncr.27787
Leventhal, H., Meyer, D., & Nerenz, D. (1980). The common sense model of illness danger. In S. Rachman (Ed.), Medical psychology (pp. 7–30). New York, NY: Pergamon.
Luszczynska, A., Scholz, U., & Schwarzer, R. (2005). The General Self-Efficacy Scale: Multicultural validation studies. Journal of Psychology, 139, 439–457. doi:10.3200/JRLP.139.5.439-457
Magai, C., Consedine, N.S., Adjei, B.A., Hershman, D., & Neugut, A. (2008). Psychosocial influences on suboptimal adjuvant breast cancer treatment adherence among African American women: Implications for education and intervention. Health Education and Behavior, 35, 835–854. doi:10.1177/1090198107303281
Martin, D.N., Boersma, B.J., Yi, M., Reimers, M., Howe, T.M., Yfantis, H.G., . . . Ambs, S. (2009). Differences in the tumor microenvironment between African-American and European-American breast cancer patients. PLoS One, 4(2), e4531. doi:10.1371/journal.pone.0004531
Martin, M.Y., Fouad, M.N., Oster, R.A., Schrag, D., Urmie, J., Sanders, S., & Pisu, M. (2014). What do cancer patients worry about when making decisions about treatment? Variation across racial/ethnic groups. Supportive Care in Cancer, 22, 233–244. doi:10.1007/s00520-013-1958-5
Matthews, A.K., Sellergren, S.A., Manfredi, C., & Williams, M. (2002). Factors influencing medical information seeking among African American cancer patients. Journal of Health Community, 7, 205–219. doi:10.1080/10810730290088094
Mazor, K.M., Beard, R.L., Alexander, G.L., Arora, N.K., Firneno, C., Gaglio, B., . . . Gallagher, T.H. (2013). Patients’ and family members’ views on patient-centered communication during cancer care. Psycho-Oncology, 22, 2487–2495. doi:10.1002/pon.3317
McCorkle, R., & Quint-Benoliel, J. (1983). Symptom distress, current concerns and mood disturbance after diagnosis of life-threatening disease. Social Science and Medicine, 17, 431–438.
Morimoto, L., Coalson, J., Mowat, F., & O’Malley, C. (2010). Factors affecting receipt of chemotherapy in women with breast cancer. International Journal of Women’s Health, 2, 107–122.
National Cancer Institute. (2014). Contents of the SEER Cancer Statistics Review (CSR), 1975–2011. Retrieved from http://seer.cancer.gov/csr/1975_2011/sections.html
Nehls, W., Gabrijel, S., Kiss, A., Kollmeier, J., Schmalz, O., Albrecht, H., . . . Bauer, T.T. (2013). Physician communication in a lung cancer center—Does the message come across? Pneumologie, 67, 688–693. doi:10.1055/s-0033-1358999
Nurgalieva, Z.Z., Franzini, L., Morgan, R.O., Vernon, S.W., Liu, C.C., & Du, X.L. (2013). Impact of timing of adjuvant chemotherapy initiation and completion after surgery on racial disparities in survival among women with breast cancer. Medical Oncology, 30, 419. doi:10.1007/s12032-012-0419-1
Olopade, O.I., Grushko, T.A., Nanda, R., & Huo, D. (2008). Advances in breast cancer: Pathways to personalized medicine. Clinical Cancer Research, 14, 7988–7999. doi:10.1158/1078-0432.CCR-08-1211
Paschal, A.M., Ablah, E., Wetta-Hall, R., Molgaard, C.A., & Liow, K. (2005). Stigma and safe havens: A medical sociological perspective on African-American female epilepsy patients. Epilepsy and Behavior, 7, 106–115. doi:10.1016/j.yebeh.2005.03.020
Peto, R., Davies, C., Godwin, J., Gray, R., Pan, H.C., Clarke, M., . . . Pritchard, K. (2012). Comparisons between different polychemotherapy regimens for early breast cancer: Meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet, 379, 432–444. doi:10.1016/s0140-6736(11)61625-5
Robinson-White, S., Conroy, B., Slavish, K., & Rosenzweig, M. (2010). Patient navigation in breast cancer: A systematic review. Cancer Nursing, 33, 127–140.
Rose, A., Peters, N., Shea, J.A., & Armstrong, K. (2004). Development and testing of the health care system distrust scale. Journal of General Internal Medicine, 19, 57–63.
Rosenzweig, M., Brufsky, A., Rastogi, P., Puhalla, S., Simon, J., & Underwood, S. (2011). The attitudes, communication, treatment, and support intervention to reduce breast cancer treatment disparity. Oncology Nursing Forum, 38, 85–89. doi:10.1188/11.ONF.85-89
Royak-Schaler, R., Passmore, S.R., Gadalla, S., Hoy, M.K., Zhan, M., Tkaczuk, K., . . . Hutchison, A.P. (2008). Exploring patient-physician communication in breast cancer care for African American women following primary treatment. Oncology Nursing Forum, 35, 836–843. doi:10.1188/08.ONF.836-843
Rust, C., & Davis, C. (2011). Health literacy and medication adherence in underserved African-American breast cancer survivors: A qualitative study. Social Work in Health Care, 50, 739–761. do:10.1080/00981389.2011.585703
Sadler, G.R., Ko, C.M., Cohn, J.A., White, M., Weldon, R.N., & Wu, P. (2007). Breast cancer knowledge, attitudes, and screening behaviors among African American women: The Black cosmetologists promoting health program. BMC Public Health, 7, 57.
Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: NFER-NELSON.
Seror, V., Cortaredona, S., Bouhnik, A.D., Meresse, M., Cluze, C., Viens, P., . . . Peretti-Watel, P. (2013). Young breast cancer patients’ involvement in treatment decisions: The major role played by decision-making about surgery. Psycho-Oncology, 22, 2546–2556. doi:10.1002/pon.3316
Shea, J.A., Beers, B.B., McDonald, V.J., Quistberg, D.A., Ravenell, K.L., & Asch, D.A. (2004). Assessing health literacy in African American and Caucasian adults: Disparities in Rapid Estimate of Adult Literacy in Medicine (REALM) scores. Family Medicine, 36, 575–581.
Sheppard, V.B., Isaacs, C., Luta, G., Willey, S.C., Boisvert, M., Harper, F.W., . . . Mandelblatt, J.S. (2013). Narrowing racial gaps in breast cancer chemotherapy initiation: The role of the patient-provider relationship. Breast Cancer Research and Treatment, 139, 207–216. doi:10.1007/s10549-013-2520-3
Sheppard, V.B., Williams, K.P., Harrison, T.M., Jennings, Y., Lucas, W., Stephen, J., . . . Taylor, K.L. (2010). Development of decision-support intervention for Black women with breast cancer. Psycho-Oncology, 19, 62–70. doi:10.1002/pon.1530
Skalla, K.A., Bakitas, M., Furstenberg, C.T., Ahles, T., & Henderson, J.V. (2004). Patients’ need for information about cancer therapy. Oncology Nursing Forum, 31, 313–319. doi:10.1188/04.ONF.313-319
Stewart, A.L., Napoles-Springer, A., & Perez-Stable, E.J. (1999). Interpersonal processes of care in diverse populations. Milbank Quarterly, 77, 305–339.
Tariq, K., Latif, N., Zaiden, R., Jasani, N., & Rana, F. (2013). Breast cancer and racial disparity between Caucasian and African American women, part 1 (BRCA-1). Clinical Advances in Hematology and Oncology, 11, 505–509.
Thompson, T., Rodebaugh, T.L., Perez, M., Schootman, M., & Jeffe, D.B. (2013). Perceived social support change in patients with early stage breast cancer and controls. Health Psychology, 32, 886–895. doi:10.1037/a0031894
Thune-Boyle, I.C., Myers, L.B., & Newman, S.P. (2006). The role of illness beliefs, treatment beliefs, and perceived severity of symptoms in explaining distress in cancer patients during chemotherapy treatment. Behavioral Medicine, 32, 19–29. doi:10.3200/BMED.32.1.19-29
Wong, S.T., Korenbrot, C.C., & Stewart, A.L. (2004). Consumer assessment of the quality of interpersonal processes of prenatal care among ethnically diverse low-income women: Development of a new measure. Women’s Health Issues, 14, 118–129. doi:10.1016/j.whi.2004.04.003
Yoo, G.J., Levine, E.G., & Pasick, R. (2014). Breast cancer and coping among women of color: A systematic review of the literature. Supportive Care in Cancer, 22, 811–824. doi:10.1007/s00520-013-2057-3
Ziner, K.W., Sledge, G.W., Bell, C.J., Johns, S., Miller, K.D., & Champion, V.L. (2012). Predicting fear of breast cancer recurrence and self-efficacy in survivors by age at diagnosis. Oncology Nursing Forum, 39, 287–295. doi:10.1188/12.ONF.287-295
About the Author(s)
Jiang is a research fellow in the Department of Systems, Populations and Leadership at the University of Michigan School of Nursing in Ann Arbor; and Sereika is a professor in the School of Nursing and director of the Center for Research and Evaluation in the Department of Health and Community Systems, Bender is a professor in the School of Nursing and PhD program director, Brufsky is a professor in the School of Medicine, and Rosenzweig is an associate professor in the School of Nursing, all at the University of Pittsburgh in Pennsylvania. No financial relationships to disclose. Jiang, Sereika, Bender, Brufsky, and Rosenzweig contributed to the conceptualization and design. Rosenzweig completed the data collection. Jiang and Sereika provided statistical support and analysis. Jiang, Sereika, Bender, and Rosenzweig contributed to the manuscript preparation. Jiang can be reached at jiangyu@umich.edu, with copy to editor at ONFEditor@ons.org. Submitted May 2015. Accepted for publication August 16, 2015.

