Integrative Review: Effects of Music on Cancer Pain in Adults
Problem Identification: To evaluate the literature for music’s effect on adult cancer pain.
Literature Search: An electronic literature search from 1986–2014 was conducted to evaluate the effects of quantitative music among adults with cancer pain in settings including homes, hospitals, and palliative care units. Databases used were PubMed (MEDLINE®) and Scopus.
Data Evaluation: The study designs, methods, measures, outcomes, and limitations were evaluated independently by the primary author and verified by the second author. The primary outcome measure of interest was the effect of music in cancer pain.
Synthesis: Of 82 studies, 5 of them—totaling 248 participants—met eligibility criteria. Review of findings suggests a paucity of innovative approaches for using music to mitigate cancer pain among adults. Psychological outcomes, anxiety, depression, and mood were understudied. Advanced pain, multiple cancer types, and lack of racial diversity characterize the samples.
Conclusions: Modern treatments for cancer have improved survival rates; however, patients often experience tumor- and treatment-related pain. Pharmacologic and nonpharmacologic methods may minimize cancer pain. The use of music as an adjunct to pain medication requires additional studies, particularly on mechanisms of its effect on pain among diverse, large samples with multiple cancer pain types. A limitation of this review is the small number of available studies to date.
Implications for Practice: The evidence for music therapy in the management of pain is limited. Integrative methods using music may represent an important intervention that nurses may be able to suggest as an inexpensive, nontoxic, and readily available intervention for potentially minimizing cancer pain.
Jump to a section
Despite advances in pain neurophysiology, assessment, and treatment, the burden of cancer pain is significant and one of the most common and distressing symptoms in patients with cancer (Hui & Bruera, 2014). This challenge continues to increase because of the rising global prevalence of pain and cancer. The World Health Organization estimates that limited or no treatment for cancer pain affects as many as 5.5 million people (Popat, McQueen, & Feeley, 2013). In addition, an estimated 12 million individuals are diagnosed with cancer each year throughout the world, with 7 million people dying annually (Popat et al., 2013). Cancer pain, a common and feared symptom among patients, is broadly classified into nociceptive (somatic and visceral) and neuropathic pain. Nociceptors, sensory receptors preferentially sensitive to noxious stimuli, are primary afferent nerves with peripheral terminals. Neuropathic pain is characterized as a complex combination of syndromes with inflammatory and ischemic components involving multiple sites (de la Cruz & Bruera, 2010). Neuropathic pain related to treatment surpasses tumor effects as the major contributor to chronic pain in survivors (Paice, 2011). Estimates indicate that pain affects about 49%–57% of survivors and 56%–75% of patients with extensive disease (Hui & Bruera, 2014). Based on a systematic review of the past 40 years, prevalence of cancer pain for patients at all disease stages was reported to be 53%, with more than 33% of patients rating their pain as moderate to severe (van den Beuken-van Everdingen et al., 2007).
Recommendations to improve pain control include evidence-based clinical practice guidelines that integrate a variety of pharmacologic and nonpharmacologic options (Miaskowski et. al., 2005; Paice & Ferrell, 2011). Nonpharmacologic interventions are categorized as alternative medical systems, manipulative and body-based methods, energy therapies, and mind-body medicine (Bardia, Barton, Prokop, Bauer, & Moynihan, 2006). Music is frequently classified within the category of mind-body interventions (Bardia et al., 2006; Elkins, Fisher, & Johnson, 2010). Complementary methods such as music are gaining increasing interest among patients and providers and may be administered as an adjuvant on an intermittent basis to reduce pain (Elkins et al., 2010).
Complementary or alternative methods, defined as complex interventions, differ from the precise mechanisms of action and schedules commonly ascribed to drug-based interventions (Bennett, 2010). Multiple complementary, alternative, and mind–body interventions have been studied. Complexity of these interventions is challenging to evaluate, and methods to elucidate these interventions are important to study. Qualitative aspects of measurement, focus groups, interviews, grounded theories, music therapy, and, particularly, the independent use of music by nurses should be evaluated.
First-line standard treatment approaches to manage pain are understudied but are common practice to treat pain. For example, pure opioid agonists produce analgesia by activation of mu and kappa receptors in the central nervous system, reducing or eliminating many types of pain. Opioids, administered continuously or intermittently over time, are a cornerstone in the management of acute and chronic cancer pain. A specific physiologic mechanism for pain relief using music has not been elucidated. However, decreased pain may be related to endogenous pain modulation and psychological outcomes including reduced anxiety, relaxation, improved mood, distraction, and suggestion of effectiveness by a healthcare provider or researcher (Bennett, 2010; Weisenberg, 1987).
Several methodologic challenges affect the design and conduct of nonpharmacologic studies, including optimal dosing determination, complexity and fidelity of the intervention in the experimental arm, selection of an appropriate control, blinding of subjects, valid and reliable measures, separation of specific effects from context effects, and timing and selection of appropriate outcomes (Bennett, 2010).
Quantitative studies specifically addressing music and cancer pain are few in number. Population parameters of effect size are not presently available from meta-analyses. However, Huang, Good, and Zauszniewski (2010) reported Cohen’s d of 0.64 and 0.7 for sensation and distress of pain, respectively. These data represent large effect sizes in a study examining the effectiveness of music in relieving cancer pain. Despite a lack of detailed mechanistic underpinnings, methodologic challenges, and a paucity of studies examining music and cancer pain as integrative therapy, music interventions to relieve cancer pain are widely used.
Further investigation of music’s role in cancer pain is essential to establish efficacy and safety. In this literature review, an evaluation of the effect of music on cancer pain was done. This review is consistent with the Oncology Nursing Society’s commitment to integrate best scientific evidence for pain relief into practice, education, and research. In addition, the Institute of Medicine ([IOM], 2011) released a blueprint for transforming prevention, care, education, and research to relieve cancer and other chronic pain. Analysis of the effect of music on cancer pain is necessary to identify gaps and ultimately promote methodologically sound investigations with results demonstrating efficacy and safety or lack thereof. Scholarly research that provides evidence of effective interventions that are inexpensive, nontoxic, noninvasive, and easily applied to individualize pain care and promotion of self-management may potentially contribute to the IOM transformation for pain relief.
Literature Search
The purpose of this review was to examine published quantitative experimental research studies specifically conducted to investigate the effects of music as an intervention for cancer-related pain. Inclusion criteria were studies published in English with participants aged 21 years and older with intact cognitive and auditory function. An exclusion criterion was cognitive dysfunction that would prevent intended use of the intervention or report of pain or mood. For the purposes of this review, cancer-related pain was defined as pain because of a diagnosis of cancer that may involve tumor- or treatment-related pain. The literature review was initially done in February 2011 and updated in May 2014 using the databases of PubMed (MEDLINE®) and Scopus. Medical Subject Headings (MeSH) terms used included pain, neoplasm, music, music therapy, complementary therapies, and randomized clinical trial. The key words anxiety and depression were added in the Scopus search. CINAHL® included similar headings to MeSH. The search was limited to English-language articles published from 1986–2014. The Cochrane Collaboration also was searched for synthesis of data on music interventions for pain relief in patients with cancer.
Search Results
Seventy-two potentially relevant studies were retrieved. A manual search of references in selected studies contributed 10 additional articles for a total of 82 studies. Seventy-seven studies were excluded primarily because they did not contain the condition of cancer pain as the primary research focus; conditions included stress, mood, anxiety, emotional distress, depression, agitation, psychotic symptoms, and quality of life or a combination of conditions with few patients diagnosed with cancer. In addition, studies were eliminated because of a case study approach involving few participants or a varied live music intervention delivered by a music therapist to a small number of participants.
Five studies including 248 participants met the criteria for eligibility—quantitative research using music as an intervention for cancer-related pain in adults. Findings for each of the studies—purpose, design, treatment and control groups, sample, setting, type of music, intervention details, outcome measures, limitations, and results—are presented in Table 1. All studies proposed to evaluate the effect of music on cancer-related pain with participants who were taking analgesics or sedatives or had such medications prescribed. One study (Kwekkeboom, 2003) included distraction in addition to music as an intervention to assess effects on pain.
[[{"type":"media","view_mode":"media_original","fid":"19266","attributes":{"alt":"","class":"media-image","height":"507","typeof":"foaf:Image","width":"708"}}]]
[[{"type":"media","view_mode":"media_original","fid":"19271","attributes":{"alt":"","class":"media-image","height":"371","typeof":"foaf:Image","width":"708"}}]]
Design, Setting, Sample, and Treatment Groups
Of the five studies, two researchers selected randomized, controlled designs and one researcher chose an experimental crossover design (Beck, 1991; Huang et al., 2010; Kwekkeboom, 2003). Two other studies used a pre-/post-test (Zimmerman, Pozehl, Duncan, & Schmitz, 1989) and quasi-experimental design (Curtis, 1986). Study settings included home, palliative care, and hospitals. Sample size among studies ranged from 9–126 participants. The mean age of participants spanned from 53–60 years, with no reported mean for one study (Curtis, 1986). In all studies, with the exception of Huang et al. (2010), participants were classified as Caucasian or white, with four participants classified as other. In all studies, treatment and control groups appeared to be similar.
Intervention
Music therapy, unlike music, requires specialization in the field. Music therapists may employ several instruments and tailor the session to varied unique designs. All authors of the five studies did research with a specific aim to evaluate the effect of music on cancer pain. Design and treatment groups varied among investigators. Of the five studies, two described the music interventions as relaxing (Beck, 1991) and calming (Curtis, 1986). Huang et al. (2010) offered patients folk songs, Buddhist hymns, harp, and piano. Kwekkeboom (2003) used a variety of music styles, and Zimmerman et al. (1989) used 10 varied types of instrumental audio recordings. All investigators used recorded music, which was preselected by the investigator or a music therapist.
With the exception of Beck (1991), four investigators offered a limited variety of prerecorded musical selections. Participants chose their preferred music and listened via headphones or earphones in the range of 15–45 minutes for 1–10 days. A researcher or nurse delivered the interventions in at least three of the studies. Who delivered the interventions in Curtis (1986) was not clear. Beck’s (1991) study setting was the home, so participants likely applied the intervention. Two studies were done outside of the United States—one in Canada (Curtis, 1986) and one in Taiwan (Huang et al., 2010).
Beck (1991) included four treatment phases. During phase one, baseline data were recorded by participants for three days, followed by randomization to music or sound twice a day during a three-day period. In phase two, participants indicated pain and mood ratings prior to and following intervention (either music or sound, a 60-cycle hum) at a time convenient to them. Phase three involved crossover to the alternative intervention not selected in phase two. Following each phase, a washout day of no intervention was implemented to minimize carryover effects from the prior intervention. The researcher visited participants on all three washout days to interview participants and collect data. A final phase allowed the researcher to collect additional data regarding the participants’ experience of music versus sound.
Curtis’s (1986) intervention was similar to Beck’s (1991) in some respects. Curtis (1986) included three conditions for each participant—no intervention, background sound, and music. During the course of 10 days, each participant received a 15-minute music intervention once each day for 10 days. All patients received analgesics.
Huang et al. (2010) planned the music intervention as a single session. The majority of patients (n = 62) in the treatment group chose audio recordings of instrumental Taiwanese music. Patients were instructed to listen to selected music for 30 minutes. To prevent demoralization among control group participants (n = 64), Huang et al. (2010) allowed them to listen to music after resting. These participants rested in bed for 30 minutes and were given a recording of chosen music after 30 minutes.
Kwekkeboom’s (2003) intervention involved a variable duration of music listening prior to and during operative procedures. In addition, a second group was offered the option to select a book on tape with various story styles. A portable cassette player and headphones were used to deliver the intervention. Participants in the control group rested quietly before and after the procedure. Participants received local anesthetics along with analgesics or sedatives as requested.
Zimmerman et al. (1989) also planned the intervention as a single session. Patients in the treatment group were instructed to relax, which potentially could reduce pain while they listened to a 30-minute recording of selected music. Participants in the control group were encouraged to rest and relax to minimize pain.
Outcome Measures
The primary outcome measure of interest was the effect of music on pain. Baseline and post-treatment pain intensity were measured using pain visual analog scales (P-VAS), numeric rating scales (NRS), and a modified graphic rating scale (GRS). The P-VAS and NRS are commonly accepted as valid and reliable measures of pain intensity (Hjermstad et al., 2011). Anchors of “no pain” to “excruciating pain” typify the P-VAS, and the NRS range is 0–10, with 0 indicating no pain and 10 indicating excruciating pain. The modified GRS used by Curtis (1986) was described as a 10 cm horizontal line with descriptive terms. Reliability and validity ratings for the modified GRS are not available. In addition to the P-VAS, Beck (1991) also included the Present Pain Inventory (PPI) of the McGill Pain Questionnaire (MPQ). The PPI is a one-dimensional instrument with a scale ranging from 0 (no pain) to 5 (excruciating pain). The MPQ is a multidimensional tool with demonstrated reliability and validity to measure cancer pain.
Results
Despite nonsignificant findings, Beck (1991) reported a decrease in pain that was twice as great for music in comparison to sound. All participants in Beck’s (1991) sample (N = 15) had advanced-stage disease, and all but one participant took scheduled analgesics. About half of the sample used methadone (Dolophine®). All participants in the sample enjoyed music. Five reported that they participated in special music events, three enjoyed listening to music, six were music performers, and one was a musician. Overall, preferences for music included easy listening (n = 6), country/Western (n = 4), classical (n = 3), new age (n = 1), and rock (n = 1). Levels of response to music among the sample included great (n = 3), moderate (n = 4), some (n = 4), and none (n = 4).
Nonsignificant findings also were reported in Curtis (1986). However, individual patient responses did indicate a positive effect for music in reducing pain among a sample of terminally ill patients. One of the study conditions, background sound, which was described as listening to ambient sounds within the hospital environment, appeared to have a negative effect on participants (Curtis, 1986).
Kwekkeboom (2003) concluded that music may act as a mode of distraction, accounting for no significant differences between the interventions of music and a book on tape. In addition, experimental interventions may not have been helpful in Kwekkeboom’s (2003) study because patients, some recently diagnosed with cancer, may have preferred little to no distraction. An alert state during procedures (e.g., biopsies, catheter or port placement or removal) may have been a preference for some patients, particularly those recently diagnosed with cancer. Kwekkeboom (2003) reported that about one-third of patients used analgesics and anxiolytics. If a greater number of patients in the music group requested analgesics and anxiolytics, perhaps the effects of music would have been significantly greater than effects of simple distraction. The mean procedural pain score of 2.33 (adjusted for covariates), with a range of 0–10, may explain few requests for analgesics.
Among the five studies, two showed significant differences in self-reported pain using music (Huang et al., 2010; Zimmerman et al., 1989). Huang et al. (2010) found that music significantly reduced pain in the experimental group (p < 0.001). Pain sensation and pain distress using Cohen’s d were reported as 0.64 and 0.7, respectively. In addition, Huang et al.’s (2010) findings showed 50% pain relief among 42% of patients assigned to the intervention group, compared to 8% of patients in the control group.
Zimmerman et al. (1989) reported significant differences in pain reduction on all MPQ indices. P-VAS scores also were reported to be significantly decreased in the music group (p < 0.01).
Conceptual Frameworks
Two of five studies used frameworks for support. Beck (1991) developed a model emanating from psychological and physiologic pain theories related to endogenous pain modulation. Possible mechanisms linking music to affective and cognitive effects were postulated to account for improved mood, decreased anxiety, and increased control and distraction, all potentially reducing pain. Huang et al. (2010) briefly cited a conceptual framework of acute pain management published by Good (2004).
Of the five studies analyzed in this literature review, one author described an adequate model to support the study. Beck (1991) developed and clearly described a model of distraction as one pathway that leads to endogenous pain modulation. An additional framework, the biopsychosocial model, is frequently cited as a chief model to assess and treat cancer pain (Somers, Keefe, Kothadia, & Pandiani, 2010). This model addresses the impact of biologic (e.g., tissue damage), psychological (e.g., anxiety, fear), and social (e.g., satisfaction with relationships) factors, all influencing pain response and treatment. Multiple unique aspects relevant to an individual with cancer pain—a primary focus of pain evaluation—are accounted for in this model.
Discussion
This review reveals a paucity of randomized, controlled trials (RCTs) for music as a treatment for cancer pain. Two authors published RCTs that examined music as a therapeutic intervention for cancer-related pain in adults (Huang et al., 2010; Kwekkeboom, 2003). Both of these studies provide important implications for subsequent studies. First, and perhaps most relevant, the Huang et al. (2010) trial with 126 Taiwanese participants reported significant findings. Caucasian participants almost exclusively characterize the other four samples in this review.
Beck’s (1991) study, although dated, has been critically appraised and continues to be cited in the literature because of rigorous methodology (Bradt, Dileo, Grocke, & Magill, 2011; Cepeda, Carr, Lau, & Alvarez, 2006). Small sample size (N = 15) may have contributed to nonsignificant findings in Beck’s (1991) study. Finally, Kwekkeboom (2003), although not reporting significant outcomes, does provide useful interpretations for the distracting effects associated with listening to music.
The National Institutes of Health ([NIH), 2011) released a report recommending best practices for combining quantitative and qualitative research, a method proposed for significant public health problems. Adding qualitative methods would provide valuable insights into the lived experience of unrelieved cancer pain. Two studies cited in this review (Beck, 1991; Huang et al., 2010) included information about the participants’ past and current experience with music to manage pain. Using focus groups involving patients with cancer to gather unique perceptions about cancer treatment may identify important patterns. Engagement of participants may be more effective in small focus groups.
Inclusion of ethnic and racial minorities in studies of cancer pain is a priority, mandated for funding by NIH since 2003 (Green et al., 2003). Ethnic and racial minorities may carry the largest burden from cancer because of less than adequate access to healthcare facilities that provide prescription pain medications, including opioids and other agents noted to minimize neuropathic pain (Shavers, Bakos, & Sheppard, 2010). Ethnic and racial minorities may have misperceptions that pain medications are addictive (Paice & Ferrell, 2011). Projections indicate that ethnic and racial minority populations will constitute 50% of the U.S. population by 2050 (Shavers et al., 2010).
Discussions with patients to dispel myths about cancer pain and treatment approaches require regular and detailed communication with providers. Without access to adequate health care, further suffering will ensue. Integrative methods such as music can minimize cancer pain.
Limitations
Few quantitative studies of music for cancer pain have been conducted. Only five studies were eligible for inclusion in this review, a significant limitation. Of these studies, most had inadequate sample size. Most patients were hospitalized with advanced disease and a wide variety of malignancies. Limited choice of music was available for patient selection in all studies. In addition, lack of racial and ethnic diversity was characteristic of all studies, with the exception of one study conducted in Taiwan. Only two studies involved RCTs. Overall, conceptual models linking the action of music to pain relief are not well described.
Implications for Nursing
Music interventions applied in this review were generally tailored to patient preferences. A Cochrane review published in 2006 indicated that positive effects of music did not significantly differ between participants who selected the music and those not given the option for self-selection (Cepeda et al., 2006). Additional research is necessary to evaluate this finding. Preferred procedures using music have been suggested to include instrumental music, low tones with strings as a predominant feature opposed to brass or percussion, and a decibel volume no greater than 60 (Staum & Brotons, 2000). Other attributes of music such as pitch, timbre, tempo, and rhythm also are important to evaluate (Nilsson, 2008; Sacks, 2007). Musical selections also have been recommended to match average heart rates—60–80 beats per minute—to promote positive outcomes on pain and relaxation (Nilsson, 2008). Continued research is a priority to elucidate the most favorable type of music and selection methods to reduce cancer pain.
An ideal opportunity to discuss the role of music for cancer pain includes introduction to the topic, beginning with nursing staff orientation. Orientation optimally should include content on the use of self-selected, culturally appropriate music as an adjunct to analgesic medications for cancer pain. Nursing faculty assigned as clinical preceptors can teach nursing students about the safety and efficacy of music to modulate cancer pain. Philanthropic organizations have acquired baby grand pianos for hospital units. The pianos include a variety of preselected recordings that patients and visitors can enjoy. At Rush University Medical Center in Chicago, Illinois, the authors have promoted music listening by inviting patients and nursing and medical students who are pianists to play the piano at intervals throughout the day and evening. Nurse researchers should continue to examine the possibilities of using music in a variety of formats to relieve cancer pain.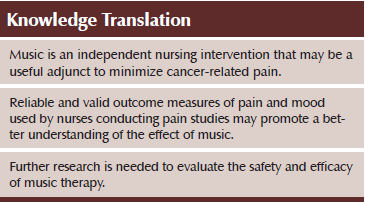
Conclusion
Pain is one of the most feared and prominent symptoms associated with cancer. The IOM’s (2011) blueprint addresses the critical need to transform prevention, care, education, and research to advance the science and practice for pain control. Global collaboration among researchers is essential to achieve significant progress toward optimal pain management and improved quality of life. As music delivery in hospitals and outpatient settings is becoming more popular, studying outcomes is increasingly important. Using methods such as Pandora® Radio maximizes patient preferences for a broad variety of selections that may reduce cancer pain. Nonpharmacologic pain interventions such as music are nontoxic, inexpensive, readily available, and an independent nursing intervention. Additional studies using rigorous methods including quantitative and qualitative approaches potentially may improve understanding of the effect of music on cancer pain.
References
Bardia, A., Barton, D.L., Prokop, L.J., Bauer, B.A., & Moynihan, T.J. (2006). Efficacy of complementary and alternative medicine therapies in relieving cancer pain: A systematic review. Journal of Clinical Oncology, 24, 5457–5464. doi:10.1200/JCO.2006.08.3725
Beck, S.L. (1991). The therapeutic use of music for cancer-related pain. Oncology Nursing Forum, 18, 1327–1337.
Bennett, M.I. (2010). Methodological issues in cancer pain: Nonpharmacological trials. In J.A. Paice, R.F. Bell, E.A. Kalso, & O.A. Soyannwo (Eds.), Cancer pain: From molecules to suffering (pp. 207–218). Seattle, WA: International Association for the Study of Pain Press.
Bradt, J., Dileo, C., Grocke, D., & Magill, L. (2011). Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews, 8, CD006911.
Cepeda, M.S., Carr, D.B., Lau, J., & Alvarez, H. (2006). Music for pain relief. Cochrane Database of Systematic Reviews, 2, CD004843.
Curtis, S.L. (1986). The effect of music on pain relief and relaxation of the terminally ill. Journal of Music Therapy, 23, 10–24.
de la Cruz, M.G., & Bruera, E. (2010). Pharmacologic considerations in palliative care. In P. Beaulieu, D. Lussier, F. Porreca, & A.H. Dickenson (Eds.), Pharmacology of pain (pp. 585–604). Seattle, WA: International Association for the Study of Pain Press.
Elkins, G., Fisher, W., & Johnson, A. (2010). Mind-body therapies in integrative oncology. Current Treatment Opinions in Oncology, 11, 128–140. doi:10.1007/s11864-010-0129-x
Good, M. (2004). Pain: A balance between analgesia and side effects. In S.J. Peterson (Ed.), Middle range theories: Application to nursing research (pp. 59–77). New York, NY: Lippincott Williams and Wilkins.
Green, C.R., Anderson, K.O., Baker, T.A., Campbell, L.C., Decker, S., Fillingim, R.B., . . . Vallerand, A.H. (2003). The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Medicine, 4, 277–294. doi:10.1046/j.1526-4637.2003.03034.x
Hjermstad, M.J., Fayers, P.M., Haugen, D.F., Caraceni, A., Hanks, G.W., Loge, J.H., . . . Kaasa, S. (2011). Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: A systematic literature review. Journal of Pain and Symptom Management, 6, 1073–1093.
Huang, S.T., Good, M., & Zauszniewski, J.A. (2010). The effectiveness of music in relieving pain in cancer patients: A randomized controlled trial. International Journal of Nursing Studies, 47, 1354–1362.
Hui, D., & Bruera, E. (2014). A personalized approach to assessing and managing pain in patients with cancer. Journal of Clinical Oncology, 32, 1640–1646. doi:10.1200/JCO.2013.52.2508
Institute of Medicine. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Retrieved from http://bit.ly/1Vs5ZaB
Kwekkeboom, K.L. (2003). Music versus distraction for procedural pain and anxiety in patients with cancer. Oncology Nursing Forum, 30, 433–440. doi:10.1188/03.ONF.433-440
Miaskowski, C., Cleary, J., Burney, R., Coyne, P., Finley, R., Foster, R., . . . Zahrbock, C. (2005). Guidelines for the management of pain in adults and children. Glenview, IL: American Pain Society.
National Institutes of Health. (2011, August 23). NIH releases best practices for combining qualitative and quantitative research. NIH News. Retrieved from http://www.nih.gov/news/health/aug2011/od-23a.htm
Nilsson, U. (2008). The anxiety- and pain-reducing effects of music interventions: A systematic review. AORN Journal, 87, 780–807. doi: 10.1016/j.aorn.2007.09.013
Paice, J.A. (2011). Chronic treatment-related pain in cancer survivors. Pain, 152(Suppl. 3), S84–S89. doi:10.1016/j.pain.2010.10.010
Paice, J.A., & Ferrell, B. (2011). The management of cancer pain. CA: A Cancer Journal for Clinicians, 61, 157–182. doi:10.3322/caac.20112
Popat, K., McQueen, K., & Feeley, T.W. (2013). The global burden of cancer. Best practice and research. Clinical Anaesthesiology, 27, 399–408. doi:10.1016/j.bpa.2013.10.010
Sacks, O. (2007). Musicophilia: Tales of music and the brain. New York, NY: Knopf.
Shavers, V.L., Bakos, A., & Sheppard, V.B. (2010). Race, ethnicity, and pain among the U.S. adult population. Journal of Health Care for the Poor and Underserved, 21, 177–220. doi:10.1353/hpu.0.0255
Somers, T.J., Keefe, F.J., Kothadia, S., & Pandiani, A. (2010). Dealing with cancer pain: Coping, pain catastrophizing, and related outcomes. In J.A. Paice, R.F. Bell, E.A. Kalso, & O.A. Soyannwo (Eds.), Cancer pain: From molecules to suffering (pp. 231–243). Seattle, WA: International Association for the Study of Pain Press.
Staum, M.J., & Brotons, M. (2000). The effect of music amplitude on the relaxation response. Journal of Music Therapy, 37, 22–39.
van den Beuken-van Everdingen, M.H., de Rijke, J.M., Kessels, A.G., Schouten, H.C., van Kleef, M., & Patijn, J. (2007). Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Annals of Oncology, 18, 1437–1449. doi:10.1093/annonc/mdm056
Weisenberg, M. (1987). Psychological interventions for the control of pain. Behavioral Research and Therapy, 25, 301–312.
Zimmerman, L., Pozehl, B., Duncan, K., & Schmitz, R. (1989). Effects of music in patients who had chronic cancer pain. Western Journal of Nursing Research, 11, 298–309. doi:10.1177/019394598901100304
About the Author(s)
AnnMarie Keenan, MS, RN, AOCN®, is an assistant professor and Joyce K. Keithley, DNSc, RN, FAAN, is a professor, both in the College of Nursing at Rush University in Chicago, IL. No financial relationships to disclose. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Forum or Oncology Nursing Society. Keenan can be reached at annmarie_k_keenan@rush.edu, with copy to editor at ONFEditor@ons.org. (Submitted November 2014. Accepted for publication April 29, 2015.)

