Severe Obesity in Cancer Care
Increasing weight and body fat composition has an impact on cancer detection and staging. Obese women are less likely to engage in breast and cervical screening practices. Excessive adipose tissue makes physical assessment more difficult, and patients with a BMI greater than 35 kg/m2 may have deeper and wider pelvic structures, which make internal examinations problematic. A retrospective review of 324 primary surgical patients found that patients with a BMI greater than 40 kg/m2 are seven times less likely to undergo complete surgical staging for endometrial cancer compared with individuals with a BMI less than 40 kg/m2. In addition, healthcare provider bias against the need for screening, feelings of discomfort and embarrassment, as well as patient’s fears of guilt, humiliation, and shame pose significant barriers to addressing the issue of obesity in clinical care with patients and family members.
Jump to a section
A 45-year-old woman with relapsed lymphoma named Mrs. D arrives for an appointment at the ambulatory care clinic to review the results of her recent lymph node biopsy and discuss treatment options with her oncologist. She stands in the waiting room and, when her name is called, she follows the nurse to the scale. She dreads this part of the visit. The old weight scale in the hallway cannot accommodate her weight, so she tells the nurse that she weighed herself at home this morning. At 178 cm and 190 kg, Mrs. D has a body mass index (BMI) of 60 kg/m2 and a body surface area 3.07 m2. The nurse averts her eyes, and the moment becomes awkward. Mrs. D is ushered into the room and instructed to have a seat. She gazes upon the chair in the examination room and tells the nurse she prefers to stand because she has been sitting all day. In reality, she cannot fit into the chairs at the cancer center because they all have arms on them and she is too wide.
The medical student comes in to talk with Mrs. D and complete the physical assessment. The examination table is too narrow for her to comfortably lie down, so the student quickly and clumsily assesses her for lymphadenopathy and splenomegaly and auscultates her chest for breath and heart sounds. While waiting to see her doctor, she hears the student laughing with one of his colleagues about Mrs. D and her weight. When her oncologist comes into the room, he quickly puts her at ease with his kind nature. Unfortunately, the computed tomography–guided biopsy did not yield a sufficient sample to histologically confirm an aggressive form of lymphoma. Although the positron-emission tomography (PET) scan and blood work results were suggestive of a new, aggressive lymphoma, she could not be enrolled into the clinical trial without tissue confirmation. The radiologists were not in favor of attempting a second biopsy because of her size, and her asthma and sleep apnea did not make her a good surgical candidate for an open biopsy.
Mrs. D has no palpable nodes to biopsy and her doctor agrees that the risks of open biopsy are too high. He recommends that she proceed with standard second-line chemotherapy and request the opinion of the stem cell transplantation clinic. The best chance at cure for her would be salvage chemotherapy followed by allogeneic stem cell transplantation. He tells her up front that her size and respiratory conditions may be a deterring factor; however, he will strongly recommend a transplantation because she is young and otherwise healthy. Aside from an inhaler and a proton pump inhibitor to treat gastroesophageal reflux disease, she does not take any other regular medications.
Mrs. D has tried “every diet out there” and has been trying to lose weight for years with little success. Her doctor suggests that she see the dietitian at the cancer center and start walking every day. He shows her about a moblie application he uses to track his calories and exercise on his phone, and Mrs. D is encouraged by his support.
After she leaves the clinic, the oncologist calls the pharmacist to discuss Mrs. D’s chemotherapy dosing. He recalls that, when she was treated five years prior, her doses were capped at 2 m2 because of potentially more severe myelosuppression and the high cost of the monoclonal antibody.
Background
Oncology clinicians addressing weight issues have previously been more focused on cancer-related cachexia and weight loss rather than extreme weight and the associated morbidities (Dobbins, Decorby, & Choi, 2013). The National Institutes of Health ([NIH], 2012) defined obesity as a condition of abnormally high and unhealthy body fat proportion. Obesity is most accurately measured in clinical practice using BMI, a simple, inexpensive calculation of body composition thought to be a more accurate measure than weight alone but one that does not differentiate between lean muscle mass and adipose tissue (Horowitz & Wright, 2015).
Obesity rates are rising to epidemic proportions globally, particularly in Western industrialized countries, with 35% of American adults and 17% of adolescents and children considered obese (Berger, 2014; NIH, 2012). The World Health Organization ([WHO], 2006) classifies obesity as a BMI greater than 30 kg/m2 and severe obesity as a BMI greater than 40 kg/m2. If current trends continue, 60% of the world’s population will be overweight or obese by 2030 (Horowitz & Wright, 2015; Ligibel et al., 2014). Severe obesity (BMI > 40 kg/m2) is also on the rise, accounting for an estimated 1 in 20 adults in the United States, compared with 1 in 35 in the late 1990s (Ferrante et al., 2010). Obesity is quickly overtaking tobacco as the leading preventable cause of cancer, with an estimated 3-4 million cases of cancer globally preventable by healthier eating and increasing physical activity (Dobbins et al., 2013; Ligibel et al., 2014).
Increasing weight and body fat composition also has an impact on cancer detection and staging. Obese women are less likely to engage in breast and cervical screening practices, and individuals in the United Kingdom with a BMI greater than 40 kg/m2 were least likely to participate in colorectal screening (Beeken, Wilson, McDonald, & Wardle, 2014; Ferrante et al., 2010). Excessive adipose tissue makes physical assessment more difficult, and patients with a BMI greater than 35 kg/m2 may have deeper and wider pelvic structures, which make internal examinations problematic (Beeken et al., 2014). A retrospective review of 324 primary surgical patients found that patients with a BMI greater than 40 kg/m2 are seven times less likely to undergo complete surgical staging for endometrial cancer compared with individuals with a BMI less than 40 kg/m2 (Krills, Salani, Bristow, Gerardi, & Ibeanu, 2012). Finally, healthcare provider bias against the need for screening, feelings of discomfort and embarrassment, as well as patient’s fears of guilt, humiliation, and shame pose significant barriers to addressing the issue of obesity in clinical care with patients and family members (Harris, 2008).
Evidence links obesity to esophageal, endometrial, breast (postmenopausal), colon, rectum, kidney, pancreas, gallbladder, and thyroid cancers. Obesity is a poor prognostic indicator in other malignancies as well (Berger, 2014; Demark-Wahnefried et al., 2012; Dobbins et al., 2013; NIH, 2012). Studies show that obese patients with cancer have inferior clinical outcomes than non-obese patients, but the underlying pathogenesis is multifactorial and not clearly understood (see Figure 1). Obese patients are at risk for developing multiple medical conditions, such as coronary artery disease, stroke and cerebrovascular events, hypertension, diabetes mellitus, osteoarthritis, and respiratory complications (Binks & Pyke, 2008; Horowitz & Wright, 2015). Severe obesity is associated with even more potential comorbidities (Horowitz & Wright, 2015). Obstructive hyperventilation syndrome is present in 30% of people with a BMI greater than 35 kg/m2, asthma is more severe and more common, and liver disease or fatty hepatitis is present in 25% of severely obese patients (Binks & Pyke, 2008; Brodsky, 1998; Horowitz & Wright, 2015). NIH (2012) reported that about 4% and 7% of male and female cancer deaths per year, respectively, are related to obesity, with 40% of endometrial cancer deaths attributable to obesity.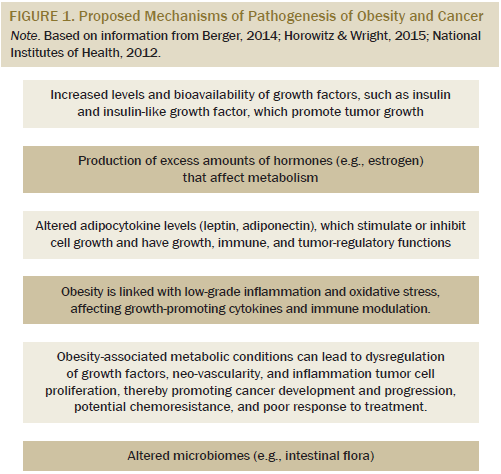
Effect of Severe Obesity on Cancer Interventions
Chemotherapy: The American Society of Clinical Oncology (ASCO) released a position statement on chemotherapy dosing in obese patients to address evidence that as many as 40% of obese patients were receiving substandard chemotherapy doses that were not based on actual body weight (Griggs et al., 2012). The panel recommended that full weight–based doses be used to treat obese patients, particularly when treatment intent was curative. No evidence exists that short- or long-term toxicity, including myelosuppression, is increased with full-weight dosing, with reduced dosing resulting in inferior progression-free survival and overall survival with higher recurrence rates. Although limited data is available on dosing in morbid obesity, the same principles are recommended by the expert panel (Griggs et al., 2012).
Body mass and increasing weight have implications on the pharmacokinetics of chemotherapy agents. Obesity affects metabolic dysregulation, drug absorption, metabolism, and excretion, and severe obesity affects hypertension and diabetes, affecting kidney function and drug elimination and, thereby, decreasing drug effectiveness (Harris, 2008; Horowitz & Wright, 2015). The practice of routinely dose-reducing chemotherapy based on an individual’s extreme weight places them at the disadvantage of being under-prescribed and potentially receiving less overall benefit.
Surgery: The surgical risks for obese patients are greater than non-obese patients (Amri, Bordeianou, Sylla, & Berger, 2014; Binks & Pyke, 2008; Brodsky, 1998) and include the following:
• Body positioning in the operating room table
• Airway management
• Effectiveness of analgesia
• Increased risk of thromboembolic events
• Impact of comorbidities on healing
• Increased oxygen requirements
• Impaired ventilation/perfusion
• Difficulty with early mobilization
• Increased risk of postoperative complications
In a retrospective chart review of 1,048 individuals surgically treated for colorectal cancer during an eight-year period, Amri et al. (2014) found that, for each progressive BMI category (healthy, overweight, obese, severe obesity), the overall risk of wound infection and delayed healing also increased. Obesity is suspected to be associated with greater difficulty with surgical resection and potentially higher postoperative complications (Benoist, Panis, & Alves, 2000; Khoury, Stocchi, & Geisler, 2011).
Implications for Nursing
Obesity and severe or extreme obesity is becoming a complex health and societal problem that healthcare providers must begin to acknowledge and address within the oncology community. Oncology nurses are well positioned to make a difference in all aspects of patient care, from suspicion and initial diagnosis to survivorship and palliation, with obesity being a potentially modifiable risk factor for cancer development and relapse (NIH, 2012). The case of Mrs. D highlights how simple tasks and aspects of oncology nursing care are hindered by severe obesity.
ASCO’s Cancer Prevention Committee and Cancer Survivorship Committees convened a working group in 2012 and identified the following priorities to address the obesity–cancer link: (a) increase provider and patient education and awareness, (b) develop clinical tools and resources to address obesity and energy balance with patients, (c) promote research, and (d) develop and advocate policies (Ligibel et al., 2014). These priorities provide the framework for nursing action. The first step is to start the conversation with patients, family members, and colleagues about weight and its link to cancer to help raise awareness and dispel myths within the cancer community. At all parts of the cancer journey, patients should be counseled about good nutrition, weight loss, the importance of physical activity, cancer screening, and early intervention. Appropriate referrals to nutrition services, physiotherapy, medical rehabilitation, endocrinology, behavioral sciences, and exercise physiology are necessary (Ligibel et al., 2014).
Nurses are not immune to the struggles with weight and weight loss. Initiating conversations with patients about lifestyle changes may be more difficult for overweight or obese nurses, but cannot be overlooked. Data, although limited, have helped researchers identify at-risk patient populations to target, such as low-income poorly educated women and non-Hispanic Black men, to encourage lifestyle modifications and cancer screening practices. Additional research is needed to identify specific interventions aimed at engaging the severely obese patient with cancer, and randomized, controlled trials need to be designed that target obese patients. Obese and severely obese patients with cancer have unique needs which have yet to be fully identified and understood.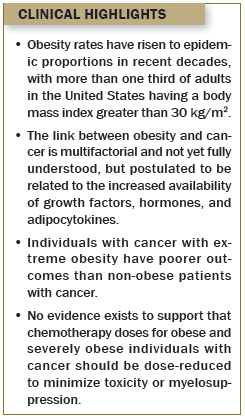
Conclusion
Work environments and institutions must be adapted to accommodate patients of all sizes. Diagnostic imaging machines must be designed to be wider and capable of accommodating larger weights and girths to ensure access to imaging for all patients. Institutions need to invest in equipment to assist clinicians with physical assessment, including wider examination tables, larger blood pressure cuffs, and larger wheelchairs. Oncology nurses can lobby and advocate for the tools necessary to perform optimal patient care and for the resources and policies necessary to minimize personal and patient risk and physical injury.
References
Amri, R., Bordeianou, L., Sylla, P., & Berger, D. (2014). Obesity, outcomes and quality of care: Body mass index increases the risk of wound-related complications in colon cancer surgery. American Journal of Surgery, 207, 17–23. doi:10.1016/j.am jsurg.2013.05.016
Beeken, R., Wilson, R., McDonald, L., & Wardle, J. (2014). Body mass index and cancer screening: Findings from the English longitudinal study of ageing. Journal of Medical Screening, 21, 76–81. doi:10.1177/0969141314531409
Benoist, S., Panis, Y., & Alves, A. (2000). Impact of obesity on surgical outcomes after colorectal resection. American Journal of Surgery, 179, 275–281. doi:10.1016/S0002-9610(00)00337-8
Berger, N. (2014). Obesity and cancer pathogenesis. Annals of the New York Academy of Sciences, 1311, 57–76. doi:10.1111/nyas .12416
Binks, A., & Pyke, M. (2008). Anaesthesia in the obese patient. Anaesthesia and Intensive Care Medicine, 9(7), 299–302. doi:10 .1016/j.mpaic.2008.04.018
Brodsky, J.B. (1998). Morbid obesity. Current Anesthesia and Critical Care, 9, 249–254. doi:10.1016/S0953-7112(98)80044-6
Demark-Wahnefried, W., Platz, E., Ligibel, J., Blair, C., Courneya, K., Meyerhardt, J., & Ganz, P. (2012). The role of obesity in cancer survival and recurrence. Cancer Epidemiology, Biomarkers and Prevention, 21, 1244–1259. doi:10.1158/1055-9965.EPI -12-0485
Dobbins, M., Decorby, K., & Choi, B.C.K. (2013). The association between obesity and cancer risk: A meta-analysis of observational studies from 1985–2011. Preventive Medicine, 4, 1–16. doi:10.5402 /2013/680536
Ferrante, J.M., Fyffe, D.C., Vega, M., Piasecki, A., Ohman-Strickland, P., & Crabtree, B. (2010). Family physicians’ barriers to cancer screening in extremely obese patients. Obesity, 18, 1153–1159. doi:10.1038/oby.2009.481
Griggs, J., Mangu, P., Anderson, H., Balaban, E., Dignam, J., Hyrniuk, W., & Morrison, V. (2012). Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 30, 1553–1561. doi:10.1200/JCO.2011.39.9436
Harris, H. (2008). Nursing care of the morbidly obese patient. Nursing Made Incredibly Easy, 6(3), 34–43. doi:10.1097/01.NME .0000316727.99731.4d
Horowitz, N.S., & Wright, A.A. (2015). Impact of obesity on chemotherapy management and outcomes in women with gynecologic malignancies. Gynecologic Oncology, 138, 201–206. doi:10.1016/j.ygyno.2015.04.002
Khoury, W., Stocchi, W., & Geisler, D. (2011). Outcomes after laparoscopic intestinal resection in obese versus non-obese patients. British Journal of Surgery, 98, 293–298. doi:10.1002/bjs.7313
Krills, L., Salani, R., Bristow, R., Gerardi, M., & Ibeanu, O. (2012). Impact of morbid obesity on surgical staging of patients with endometrial cancer. Gynecologic Oncology, 127(1, Suppl.), S24. doi:10.1016/j .ygyno.2012.07.067
Ligibel, J.A., Alfano, C., Courneya, K., Demark-Wahnefried, W., Burger, R., Chlebowski, R., . . . Hudis, C.A. (2014). American Society of Clinical Oncology position statement on obesity and cancer. Journal of Clinical Oncology, 32, 1–8. doi:10.1200/JCO.2014.58.4680
National Institutes of Health. (2012). Obesity and cancer risk. Retrieved from http://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesi…
World Health Organization. (2006). BMI classification. Retrieved from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
About the Author(s)
Streu is a clinical nurse specialist at CancerCare Manitoba in Winnipeg, Canada. No financial relationships to disclose. Streu can be reached at erin.streu@cancercare.mb.ca, with copy to editor at ONFEditor@ons.org.

