Involvement in Decision Making and Satisfaction With Treatment Among Partners of Patients With Newly Diagnosed Localized Prostate Cancer
Purpose/Objectives: To examine partner involvement in treatment decision making for localized prostate cancer, congruence between partner involvement and patient preference, reasons for partner noninvolvement, and partner satisfaction with patient treatment.
Design: Cross-sectional exploratory study.
Setting: 100 counties in North Carolina.
Sample: 281 partners of men with newly diagnosed localized prostate cancer.
Methods: Participants completed a phone survey. Logistic regression analyses were used.
Main Research Variables: Partners’ involvement in treatment decision making, partner satisfaction with treatment, activities of partner involvement, and reasons for noninvolvement.
Findings: Of the 228 partners (81%) related to decision making, 205 (73%) were very satisfied with the treatment the patients received, and partner involvement was congruent with patient preference in 242 partners (86%). Partners reported several reasons for noninvolvement: agreeing with whatever the patient decides, trusting the doctor’s decisions, believing that the patient should make the decision, respecting the patient’s decision, and being concerned with the impact on their relationship if they chose the wrong treatment.
Conclusions: Most partners engaged in multiple activities during treatment decision making for localized prostate cancer and were satisfied with the patient’s treatment. Partner involvement was mostly congruent with patient preference.
Implications for Nursing: Partners’ active involvement in treatment decision making for localized prostate cancer (e.g., being involved in patients’ conversations with doctors) should be encouraged and facilitated for those who prefer this type of decision making.
Jump to a section
Prostate cancer is the most frequently diagnosed cancer among men in the United States (American Cancer Society, 2015; National Cancer Institute, 2014), with the vast majority (81%) of the diagnosed cases being localized and potentially curable (National Cancer Institute, 2014). Treatment decision making is a taxing process for patients with localized prostate cancer because of a large number of available treatment options (e.g., active surveillance, different types of prostatectomy, various forms of radiation with or without hormonal therapy) (National Comprehensive Cancer Network, 2015). For patients in a sexual relationship, healthcare providers treating prostate cancer commonly recommend that the patient’s partner be involved in treatment decision making (Boehmer & Clark, 2001). However, existing research often describes treatment decision making as a dyadic process between the patient and healthcare providers (Zeliadt et al., 2006), with little emphasis on partner involvement. Most descriptive (Berry et al., 2006; Diefenbach & Mohamed, 2007; Shaw, Scott, & Ferrante, 2013) and intervention studies (Berry et al., 2013; Lin, Aaronson, Knight, Carroll, & Dudley, 2009) about treatment decision making for prostate cancer have focused on the patients’ concerns and satisfaction with treatment decision making. However, partners play an important role in how well patients with prostate cancer manage their illness (Ervik, Nordøy, & Asplund, 2013; Wootten et al., 2014; Wu, Mohamed, Winkel, & Diefenbach, 2013). Partners provide informational support (e.g., gathering information, helping patients understand information) and emotional support (e.g., comfort, companionship) (Laidsaar-Powell et al., 2013; Sinfield, Baker, Agarwal, & Tarrant, 2008; Srirangam et al., 2003; Street et al., 2010). Previous research found that some partners were completely excluded from the treatment decision-making process for prostate cancer, and other couples had a joint decision-making style in which the partner discussed treatment issues with the patient (Boehmer & Clark, 2001). Limited research explores how partners are involved in treatment decision making, whether partner involvement is congruent with the patient’s expectation, and whether partner involvement is related to satisfaction with the patient’s cancer treatment. Finally, little is known about the reasons for partner noninvolvement in treatment decision making.
To address these gaps, this exploratory study examined partners’ involvement in treatment decision making for patients with newly diagnosed localized prostate cancer. The researchers described partner preferences for and actual involvement in treatment decision making, congruence between partner involvement and patient preference, reasons for partner noninvolvement, and the relationship between partner involvement in treatment decision making and satisfaction with the patient’s treatment.
Methods
Participants
Partners were eligible if they (a) were aged 21 years or older, (b) were identified as the partner by a patient who was diagnosed with localized prostate cancer within the past three months and consented to participate in the study, and (c) understood and spoke English. To keep the focus of this investigation on the patient’s cancer diagnosis and management, the researchers excluded partners if they had been diagnosed with cancer within the previous year or if they were receiving active treatment for cancer. All partners who met these criteria were included, regardless of their race, gender, or ethnicity.
Procedure
Institutional review board approval was obtained from the University of North Carolina at Chapel Hill. Participants were recruited through the North Carolina Prostate Cancer Comparative Effectiveness and Survivorship Study (NC ProCESS) (Chen et al., 2015). NC ProCESS aimed to examine the effectiveness of different treatment options using a prospective, population-based cohort of men with newly diagnosed localized prostate cancer enrolled throughout 100 counties in North Carolina using the Rapid Case Ascertainment of the North Carolina Central Cancer Registry.
NC ProCESS participants recruited during October 2011 and September 2012 were asked for permission to contact their partners regarding the study. After patient permission was received, a research assistant phoned the partner within two days to explain the details of the study and to screen for eligibility. For eligible partners who agreed to participate, a phone interview was scheduled within one week of the eligibility screening. The research assistants obtained informed consent by phone after mailing the written consent form to the partners and providing explicit explanation about the study to ensure the partner that the study materials were strictly confidential and would not affect patient care. Each interview was recorded and lasted about 30–60 minutes. To minimize the potential influence on treatment decision making, the phone interview was done after the patient made treatment decisions (i.e., within 1–3 months of treatment). Participants received a $30 gift certificate by mail when they completed the interview. The research assistants, who all had prior phone survey experience, received 64 hours of training about patient eligibility criteria, informed consent, and phone interview techniques. Weekly meetings were held, and interviews were randomly checked to ensure fidelity of the phone survey.
Measurement
Researcher-developed questionnaires were used in the phone survey. The questions regarding partner involvement in treatment decision making were developed based on a literature review and the opinions of urologic and radiation oncologists. These questions were categorized into five domains. The patient’s and his partner’s preference for and actual partner involvement in treatment decision making reported by partners included three items with dichotomized “yes” or “no” responses. Partner satisfaction with treatment included one five-point Likert-type item with responses ranging from “not at all” to “a lot.” In the current study, partner satisfaction with the treatment patients received was categorized into “very satisfied” (i.e., those who responded “a lot”) and “less than very satisfied” (including those whose responses were “not at all,” “a little,” “somewhat,” and “moderately satisfied”). Activities of partner involvement included six items with dichotomized “yes” or “no” responses (e.g., gathering information, visiting the doctor together). Reasons for partner noninvolvement in decision making each included seven five-point Likert-type items with responses ranging from “not at all” to “a lot.” In the current study, the researchers dichotomized the responses into “yes” (i.e., presence of the reason, including “moderately” and “a lot”) and “no” (i.e., absence of the reason, including “not at all,” “a little,” and “somewhat”). Congruence of partner involvement in treatment decision making and patient preference was derived from tabulating the question asking about patient preference of partner involvement (“yes” if the patient preferred partner involvement and “no” if the patient preferred partner noninvolvement) and the question about partner evaluation of his or her actual involvement (“yes” if the partner was involved and “no” if the partner was not involved). Partner involvement in treatment decision making was considered congruent with patient preference if the partner’s responses to both questions were the same (i.e., patient preferred involvement and partner was involved or patient did not expect involvement and partner was not involved). The researchers considered partner involvement in treatment decision making discordant if the partner’s responses to these two questions were different (i.e., patient preferred involvement and partner was not involved or patient did not expect involvement and partner was involved). The researchers also obtained patient and partner demographic information (see Table 1).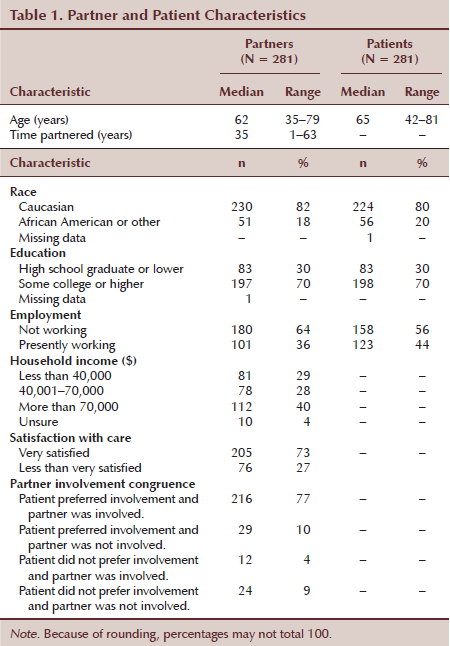
Data Analysis
The researchers analyzed the data using SAS®, version 9.3. The researchers first assessed bivariate relationships between each of the characteristics of interest using chi-squared tests for categorical characteristics and t tests for continuous characteristics. The researchers used logistic regression to examine the potential relationship between activities of partner involvement in treatment (e.g., having conversations with the doctor) and partner satisfaction with patient treatment. After fitting the full model with all possible partner involvement activities, the researchers used backwards elimination to obtain a reduced model, sequentially eliminating any partner involvement activity that was not significant at the alpha = 0.05 level. In the full and reduced models, the researchers controlled for the demographic variables of patient age and partner employment status because these variables were statistically associated with partner treatment satisfaction in bivariate analyses.
Results
Among 488 patients who received information about this project, 389 (80%) had partners and gave permission and contact information for the research staff to contact their partners. The researchers approached 316 partners (65%) successfully (contact information for 73 partners [15%] was not current) and completed informed consent and questionnaires for 281 partners (58%). The recruitment rate was 89%.
Overall, 228 partners (81%) reported involvement in treatment decision making, 205 (73%) reported being very satisfied with treatment the patients received, and 242 (86%) reported that their involvement in treatment decision making was congruent with patient preference.
Regarding the activities of partner involvement, partners most frequently worked as a team with the patient (n = 267, 95%), discussed treatment options with the patient (n = 247, 88%), went to doctor appointments with the patient (n = 244, 87%), were involved in conversations with providers (n = 230, 82%), and gathered information for the patient (n = 191, 68%). Partners less frequently helped the patient get a second opinion (n = 67, 24%). Two hundred twenty-eight of the partners (81%) reported being involved in multiple activities related to patient care.
In bivariate analyses (see Table 2), among the partner and patient characteristics, patient age and partner employment were significantly associated with partners being very satisfied with treatment. Among the partner involvement activities, the following variables were associated with partner satisfaction with patient treatment: partner involvement congruence, partners who went to doctor visits with the patients for their cancer diagnosis, partners who were involved in the patients’ conversations with their doctor, and partners who discussed different treatment options with the patients.
[[{"type":"media","view_mode":"media_original","fid":"19236","attributes":{"alt":"","class":"media-image","height":"937","typeof":"foaf:Image","width":"667"}}]]
In the full model of multivariate analysis that included all variables that were statistically significant in bivariate analyses (see Table 3), partner employment status was statistically significant (p < 0.05) and conversations with doctors were marginally significant (p = 0.07). In the reduced model, partner involvement in the patients’ conversations with their doctor were more likely to be associated with partner satisfaction with the patients’ treatment. Partners who were not working also had higher odds of being very satisfied with treatment. 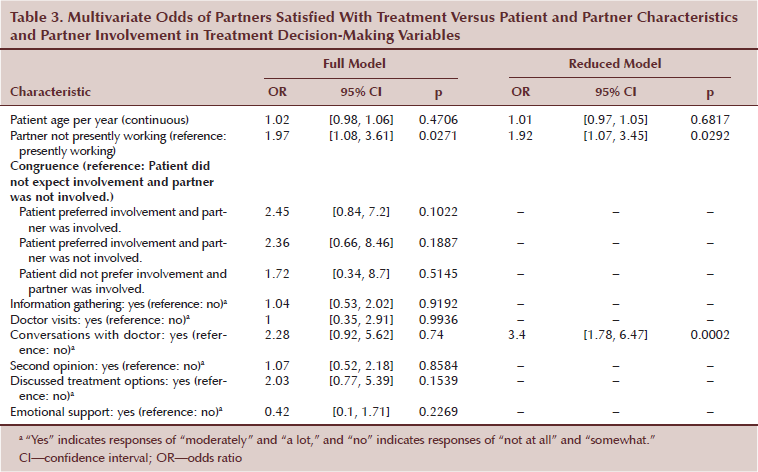
Discussion
The current study systematically examined partner involvement in treatment decision making for men with localized prostate cancer and satisfaction with the treatment they received. The researchers’ findings supported that the majority of the partners engaged in different activities during treatment decision making; most partners reported that their involvement in treatment decision making was congruent with patient preference, and most partners who were involved in decision making were very satisfied with the patients’ treatment. The researchers’ identification of the reasons for partner noninvolvement in decision making and the factors that were related to partner satisfaction with the patients’ treatment (e.g., participating in conversations with the patient’s doctor) have implications for clinical practice and additional intervention research.
The researchers’ findings indicate that providers and researchers need to pay attention to the different relationship dynamics related to partner involvement when promoting shared decision making and family involvement. Couples’ relationship dynamics provide a contextual background against which treatment decisions are negotiated and made (Boehmer & Clark, 2001; Schumm, Skea, McKee, & N’Dow, 2010). In the current study, 25 partners (9%) were not involved in treatment decision making because the patients did not want them to be involved. This result indicates that researchers and clinicians need to be mindful of the potentially different preferences in partner involvement and provide preference-sensitive care accordingly. In addition, 213 participants (76%) had partner involvement congruent with patient preference, whereas 28 (10%) did not get involved although the patients wanted them to be involved, and 11 (4%) were involved although the patients did not want them to be involved. The researchers’ results indicate that, in addition to the differing perceptions of prostate cancer–related issues (e.g., quality of life, the impact of sexual functioning) between patients and their partners (Rivers et al., 2011), some couples also are challenged by their incongruence in partner involvement. Involving partners in treatment decisions can be beneficial because of the negative impact of prostate cancer diagnosis and treatment on the well-being of the patient, his partner (Street et al., 2010; Venetis, Magsamen-Conrad, Checton, & Greene, 2014), and their relationship (Green, Wells, & Laakso, 2011; Wu et al., 2013). Additional decision aid interventions may need to resolve this incongruence or tailor materials based on couples’ preferred type of decision-making involvement styles to achieve better treatment satisfaction.
Among partners who indicated that they were not involved (see Figure 1), one of the most frequently reported reasons was that the partner believed the treatment decision was an independent decision for the patient or his healthcare provider. In previous studies, about 40% of the partners of men with localized prostate cancer preferred to take a passive role in treatment decision making (Davison et al., 2002) or wanted to avoid influencing the patient because they did not want to put additional pressure on him (Davison et al., 2002; Srirangam et al., 2003). In the current study, 94 partners (33%) who reported no involvement in treatment decision making had concerns with the negative effects a wrongly chosen decision may have on their relationship with the patient. Although the population was relatively small, the current study reminds researchers and clinicians of the dilemma that some partners may face when clinicians promote shared decision making for men with localized prostate cancer and their partner. Provider encouragement of the partner to ask questions during cancer-related clinic visits has been associated with more patient–partner interaction during the treatment decision-making process (Zeliadt et al., 2011). Additional research may need to target the common reasons for partner noninvolvement and ensure the positive effects of partner involvement to promote the benefits of shared decision making for patients and their partners.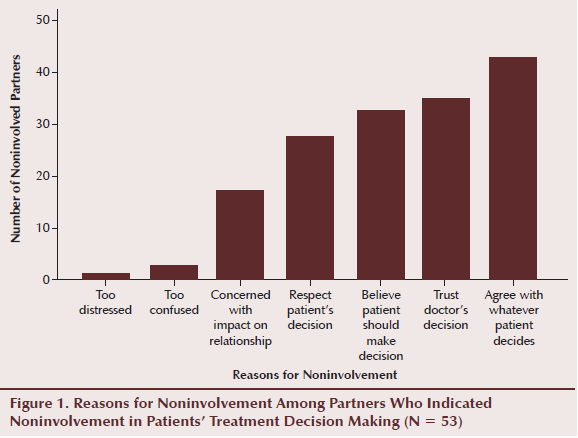
The researchers found that partners who were involved in conversations with the patient’s doctor were more likely to be very satisfied with the patient’s treatment than when partners were not involved in the conversations. When partners directly communicate with the patients’ doctor, their questions and concerns about the different treatment options are addressed and their awareness of the outcomes of various treatments may be enhanced. Therefore, they can better understand the treatment their male partner receives and feel more confident in the treatment decision, which in turn may forestall potential distress and increase their satisfaction with the patient’s treatment.
Lastly, the researchers found an association between partners who were not working and partner satisfaction with treatment. Partners who were not working may have had more time to be involved in information-seeking activities that could lead to higher confidence levels and more satisfaction about the treatment decision. Intervention efforts may focus on providing working partners with the tools they need to become involved and more satisfied with the patient’s care.
The current study had key strengths, including the generalizability of the results compared to previous studies that used convenience samples. The participants in the current study were recruited throughout 100 counties in North Carolina using the Central Cancer Registry and were diverse in their racial/ethnic backgrounds, socioeconomic status, rural/urban residence, and treatment location (community versus cancer hospitals). In addition, the researchers collected the data within three months after the patients made their treatment decision, which improves the recall and reliability of the reported results. Previous studies relied on information recalled months to years after the initial diagnosis and treatment (Feltwell & Rees, 2004; Hall, Boyd, Lippert, & Theodorescu, 2003; Sinfield et al., 2008; Srirangam et al., 2003; Street et al., 2010), which can be inaccurate and biased (Litwin & McGuigan, 1999).
One limitation of the current study is that the assessment of partner satisfaction was only measured immediately after patients received their treatment. Additional research is needed to explore whether the findings hold in long-term follow-up. In addition, the researchers relied on the literature and expert opinion to create the survey used to assess partner involvement in treatment decisions because a validated survey does not exist. Lastly, although the current study surveyed patients and partners throughout North Carolina and had a recruitment rate of 89%, it still has limitations in generalizability. The patients who denied their partners’ participation may have been self-selected, and the patients who permitted their partners to be contacted may have been more likely to involve their partners in treatment decision making than patients who declined to have their partners contacted. Additional studies should collect data of patients who decline to involve their partners in the study and compare characteristics of these patients with those who allow partner involvement. In addition, although 56 participants (20%) in the current study were African American, additional studies should oversample a higher percentage of African American men to increase generalizability because African American men have a disproportionately higher incidence of prostate cancer than non-Hispanic Caucasian men (American Cancer Society, 2015; National Cancer Institute, 2014).
Implications for Nursing
The findings from the current study have several implications for nurses because they play an important role in helping men and their partners make prostate cancer treatment decisions (Davison, Oliffe, Pickles, & Mroz, 2009; Maliski, Clerkin, & Litwin, 2004). Nurses—including nurse case managers—often assess patient preferences for treatment decision making and, in turn, can relay these preferences to other care providers such as urologists (Maliski et al., 2004). Nurses must be aware that many patients and their partners want partner involvement in treatment decision making and that involving partners in discussions about treatment decisions, if both parties prefer this type of involvement, may lead to better patient and partner satisfaction with treatment. 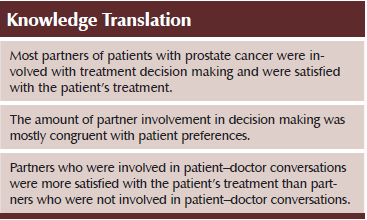
Conclusion
The current study contributes to the literature in several ways. The findings highlight how partners are involved in the treatment decision-making process for men with newly diagnosed localized prostate cancer and how this involvement relates to partner satisfaction with the treatment received. The current study also illuminates the level of congruence between patient preference for partner involvement and actual partner involvement, as well as why some partners choose not to be involved in treatment decision making. Partners of men with prostate cancer represent a group of individuals who have been understudied, and the current study provides clues as to how to harness decision making in prostate cancer care that best meets the various needs of patients and their partners.
References
American Cancer Society. (2015). Cancer facts and figures 2015. Retrieved from http://www.cancer.org/acs/groups/content/@editorial/documents/document/…
Berry, D.L., Ellis, W.J., Russell, K.J., Blasko, J.C., Bush, N., Blumenstein, B., & Lange, P.H. (2006). Factors that predict treatment choice and satisfaction with the decision in men with localized prostate cancer. Clinical Genitourinary Cancer, 5, 219–226. doi:10.3816/CGC.2006.n.040
Berry, D.L., Halpenny, B., Hong, F., Wolpin, S., Lober, W.B., Russell, K.J., . . . Swanson, G. (2013). The Personal Patient Profile-Prostate decision support for men with localized prostate cancer: A multi-center randomized trial. Urologic Oncology, 31, 1012–1021. doi:10.1016/j.urolonc.2011.10.004
Boehmer, U., & Clark, J.A. (2001). Married couples’ perspectives on prostate cancer diagnosis and treatment decision-making. Psycho-Oncology, 10, 147–155. doi:10.1002/pon.504
Chen, R.C., Carpenter, W.R., Kim, M., Hendrix, L.H., Agans, R.P., Meyer, A.M., . . . Godley, P.A. (2015). Design of the North Carolina Prostate Cancer Comparative Effectiveness and Survivorship Study (NC ProCESS). Journal of Comparative Effectiveness Research, 4, 3–9. doi:10.2217/cer.14.67
Davison, B.J., Gleave, M.E., Goldenberg, S.L., Degner, L.F., Hoffart, D., & Berkowitz, J. (2002). Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nursing, 25, 42–49. doi:10.1097/00002820-200202000-00009
Davison, B.J., Oliffe, J.L., Pickles, T., & Mroz, L. (2009). Factors influencing men undertaking active surveillance for the management of low-risk prostate cancer. Oncology Nursing Forum, 36, 89–96. doi:10.1188/09.ONF.89-96
Diefenbach, M.A., & Mohamed, N.E. (2007). Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Investigation, 25, 449–457. doi:10.1080/07357900701359460
Ervik, B., Nordøy, T., & Asplund, K. (2013). In the middle and on the sideline: The experience of spouses of men with prostate cancer. Cancer Nursing, 36(3), E7–E14. doi:10.1097/NCC.0b013e31824fe1ef
Feltwell, A.K., & Rees, C.E. (2004). The information-seeking behaviours of partners of men with prostate cancer: A qualitative pilot study. Patient Education and Counseling, 54, 179–185. doi:10.1016/S0738-3991(03)00212-X
Green, H.J., Wells, D.J.N., & Laakso, L. (2011). Coping in men with prostate cancer and their partners: A quantitative and qualitative study. European Journal of Cancer Care, 20, 237–247. doi:10.1111/j.1365-2354.2010.01225.x
Hall, J.D., Boyd, J.C., Lippert, M.C., & Theodorescu, D. (2003). Why patients choose prostatectomy or brachytherapy for localized prostate cancer: Results of a descriptive survey. Urology, 61, 402–407. doi:10.1016/S0090-4295(02)02162-3
Laidsaar-Powell, R.C., Butow, P.N., Bu, S., Charles, C., Gafni, A., Lam, W.W.T., . . . Juraskova, I. (2013). Physician-patient-companion communication and decision-making: A systematic review of triadic medical consultations. Patient Education and Counseling, 91, 3–13.
Lin, G.A., Aaronson, D.S., Knight, S.J., Carroll, P.R., & Dudley, R.A. (2009). Patient decision aids for prostate cancer treatment: A systematic review of the literature. CA: A Cancer Journal for Clinicians, 59, 379–390. doi:10.3322/caac.20039
Litwin, M.S., & McGuigan, K.A. (1999). Accuracy of recall in health-related quality-of-life assessment among men treated for prostate cancer. Journal of Clinical Oncology, 17, 2882–2888.
Maliski, S.L., Clerkin, B., & Litwin, M.S. (2004). Describing a nurse case manager intervention to empower low-income men with prostate cancer. Oncology Nursing Forum, 31, 57–64. doi:10.1188/04.ONF.57-64
National Cancer Institute. (2014). SEER stat fact sheets: Prostate cancer. Retrieved from http://seer.cancer.gov/statfacts/html/prost.html
National Comprehensive Cancer Network. (2015). NCCN Clinical Practice Guidelines in Oncology: Prostate cancer [v.1.2015]. Retrieved from http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf
Rivers, B.M., August, E.M., Gwede, C.K., Hart, A., Jr., Donovan, K.A., Pow-Sang, J.M., & Quinn, G.P. (2011). Psychosocial issues related to sexual functioning among African-American prostate cancer survivors and their spouses. Psycho-Oncology, 20, 106–110.
Schumm, K., Skea, Z., McKee, L., & N’Dow, J. (2010). ‘They’re doing surgery on two people’: A meta-ethnography of the influences on couples’ treatment decision making for prostate cancer. Health Expectations, 13, 335–349. doi:10.1111/j.1369-7625.2010.00624.x
Shaw, E.K., Scott, J.G., & Ferrante, J.M. (2013). The influence of family ties on men’s prostate cancer screening, biopsy, and treatment decisions. American Journal of Men’s Health, 7, 461–471.
Sinfield, P., Baker, R., Agarwal, S., & Tarrant, C. (2008). Patient-centred care: What are the experiences of prostate cancer patients and their partners? Patient Education and Counseling, 73, 91–96.
Srirangam, S.J., Pearson, E., Grose, C., Brown, S.C., Collins, G.N., & O’Reilly, P.H. (2003). Partner’s influence on patient preference for treatment in early prostate cancer. BJU International, 92, 365–369. doi:10.1046/j.1464-410X.2003.04355.x
Street, A.F., Couper, J.W., Love, A.W., Bloch, S., Kissane, D.W., & Street, B.C. (2010). Psychosocial adaptation in female partners of men with prostate cancer. European Journal of Cancer Care, 19, 234–242. doi:10.1111/j.1365-2354.2008.01012.x
Venetis, M.K., Magsamen-Conrad, K., Checton, M.G., & Greene, K. (2014). Cancer communication and partner burden: An exploratory study. Journal of Communication, 64, 82–102.
Wootten, A.C., Abbott, J.M., Osborne, D., Austin, D.W., Klein, B., Costello, A.J., & Murphy, D.G. (2014). The impact of prostate cancer on partners: A qualitative exploration. Psycho-Oncology, 23, 1252–1258. doi:10.1002/pon.3552
Wu, L.M., Mohamed, N.E., Winkel, G., & Diefenbach, M.A. (2013). Patient and spouse illness beliefs and quality of life in prostate cancer patients. Psychology and Health, 28, 355–368. doi:10.1080/08870446.2012.722219
Zeliadt, S.B., Penson, D.F., Moinpour, C.M., Blough, D.K., Fedorenko, C.R., Hall, I.J., . . . Ramsey, S.D. (2011). Provider and partner interactions in the treatment decision-making process for newly diagnosed localized prostate cancer. BJU International, 108, 851–856. doi:10.1111/j.1464-410x.2010.09945.x
Zeliadt, S.B., Ramsey, S.D., Penson, D.F., Hall, I.J., Ekwueme, D.U., Stroud, L., & Lee, J.W. (2006). Why do men choose one treatment over another? A review of patient decision making for localized prostate cancer. Cancer, 106, 1865–1874. doi:10.1002/cncr.21822
About the Author(s)
Yael Symes, MSPH, is a student in the School of Public Health at the University of North Carolina (UNC) at Chapel Hill; Lixin Song, PhD, is an assistant professor in the School of Nursing at UNC at Chapel Hill and at the UNC Lineberger Comprehensive Cancer Center; and Rachael G. Heineman, BA, is a graduate research assistant in the School of Public Health; Brittney D. Barbosa, BS, is a social and clinical research assistant in the Department of Radiation Oncology; Kimberly Tatum, BA, is a research assistant, and Giselle Greene, BA, BSN, is a project coordinator, both in the School of Nursing; Mark Weaver, PhD, is a research assistant professor in the School of Medicine; and Ronald C. Chen, MD, MPH, is an associate professor in the Department of Radiation Oncology, all at UNC at Chapel Hill. This study was funded by the University Cancer Research Fund from the UNC Lineberger Comprehensive Cancer Center, and the North Carolina Prostate Cancer Comparative Effectiveness and Survivorship Study was funded by the Agency for Healthcare Research and Quality of the U.S. Department of Health. Song was supported by two awards (Nos. KL2TR001109 and UL1TR001111) from the National Institute of Health/National Center for Advancing Translational Sciences through the North Carolina Translational and Clinical Sciences Institute. Song can be reached at lsong@unc.edu, with copy to editor at ONFEditor@ons.org. (Submitted February 2015. Accepted for publication May 9, 2015.)

