Disease and Symptom Care: A Focus on Specific Needs of Patients With Multiple Myeloma
Patients with multiple myeloma (MM) often deal with short- and long-term side effects of the treatment and disease sequelae. Reasons for inadequately managed symptoms are multifactorial (e.g., the patient may fear treatment interruption, the clinician does not assess or address the symptoms) and can affect patients’ ability to remain on the recommended treatment. This article provides background surrounding this supplement’s development and describes the importance of symptom assessment and management.
AT A GLANCE
- Patients with MM are vulnerable to disease- and treatment-related symptoms often because of older age, cumulative morbidities, and medication side effects.
- Guidelines for nursing management of side effects in patients with MM are absent or require updating.
- The International Myeloma Foundation Nurse Leadership Board aimed to address symptoms that patients with MM often self-manage and provide evidence-based updates for nursing symptom care in MM.
Jump to a section
Many patients with multiple myeloma (MM) live with uncontrolled or inadequately managed disease- or treatment-related symptoms, such as fatigue, diarrhea, peripheral neuropathy, and pain, despite the best efforts of healthcare providers to prevent and control these symptoms (Faiman, Stricker, et al., 2017). Patients with MM are particularly vulnerable to symptoms because of older average age, cumulative morbidities, and medication side effects. An enhanced understanding of the underlying disease mechanisms of MM has led to the development of novel and highly effective drugs from existing drug classes, as well as drugs with new mechanisms of action, such as monoclonal antibodies (e.g., daratumumab, elotuzumab) and the exportin 1 (XPO1) protein inhibitor selinexor (Faiman, Gleason, Colson, McNeill, & Catamero, 2016; Turner et al., 2016). Many patients now survive well beyond the previously projected five-year survival period. MM, particularly standard-risk MM, is viewed as a chronic illness because patients are living with the disease for more than 10 years (Kumar et al., 2012, 2014). However, disease- and treatment-related side effects negatively affect patients’ responses to therapy and quality of life (QOL) (Kumar et al., 2014), underscoring the need for supportive care for patients with MM (Faiman & Valent, 2016). Short-term side effects, such as myelosuppression with immunomodulatory drugs (e.g., lenalidomide, pomalidomide) or long-term effects of peripheral neuropathy secondary to proteosome inhibitors or the disease itself can be devastating to the individual. Nurses function in a range of capacities on the front lines of patient care and hold vital roles, such as coordinators and facilitators of care. Nurses provide care in infusion areas, act as outpatient care coordinators, and provide inpatient bedside nursing care. Throughout the continuum of care, nurses form unique relationships with patients and their caregivers. These relationships are important because patients are more likely to report symptoms to a nurse with whom they have a trusted relationship (Tariman & Szubski, 2015). Therefore, nurses are well positioned to identify, intervene in, and effectively manage disease- and treatment-related symptoms in patients with MM, improving MM treatment quality, treatment adherence, and patient QOL.
Standard treatments for MM follow continuous and maintenance protocols. Effective symptom management is a critical component of treatment adherence in MM. Continuous therapy is ongoing treatment administered without a clear stopping point intended to suppress the development of malignant clones (Faiman & Valent, 2016). Maintenance therapy is a less intense treatment designed to achieve or maintain a patient’s remission status. With ongoing treatment administration, treatment-related symptoms and disease status should be monitored continuously. Continuous and maintenance treatments are standard of care in managing MM, with several studies demonstrating their benefit for progression-free and overall survival (Attal et al., 2012; Benboubker et al., 2014; Durie et al., 2015).
The International Myeloma Foundation (IMF) Nurse Leadership Board (NLB) has previously published supplements on MM symptom management, with articles published in 2008 on myelosuppression, venous thromboembolic events, peripheral neuropathy, steroids, and gastrointestinal issues (Faiman, Bilotti, Mangan, & Rogers, 2008; Miceli, Colson, Gavino, & Lilleby, 2008; Rome, Doss, Miller, & Westphal, 2008; Smith, Bertolotti, Curran, & Jenkins, 2008; Tariman, Love, McCullagh, & Sandifer, 2008) and articles published in 2011 on renal health, bone health, functional mobility, and sexuality (Faiman, Mangan, Spong, & Tariman, 2011; Miceli, Colson, Faiman, Miller, & Tariman, 2011; Richards, Bertolotti, Doss, & McCullagh 2011; Rome, Jenkins, & Lilleby, 2011). In addition, a review of the literature established that evidence-based nursing recommendations for the management of oncologic emergencies, anxiety, fatigue, and depression are lacking (Faiman, Moran, et al., 2017). As a result, the IMF NLB updated its recommendations dating back to as early as 2008 and developed strategies for treatment adherence and graded recommendations for evidence-based best practices for MM patient care, with particular attention paid to newer drugs. The updated IMF NLB recommendations are presented in this supplement, along with practical patient education and healthcare provider tip sheets to provide valid, peer-reviewed teaching aids for nurses, clinicians, and patients. Given the availability of newly approved drugs, this supplement also provides an update about new therapeutic combinations and clinical indications for treatment agents.
Symptoms
A symptom is defined as a subjective experience that reflects changes in the physical functioning, cognition, or sensations of an individual (Dodd et al., 2001). The consequences of poorly controlled physical symptoms create major public health problems associated with decreased QOL and potential for increased healthcare-related costs and decreased adherence to therapy (Andrew, Derry, Taylor, Straube, & Phillips, 2014). Patients with inadequately controlled symptoms often cannot work, perform common household tasks, or conduct necessary activities of daily living. For patients with cancer, the inability to perform these basic functions can lead to depression, demoralization, and the lack of willingness to continue treatment (Vehling & Mehnert, 2014).
Multiple Myeloma Symptoms
Common symptoms of MM include pain, fatigue, peripheral neuropathy, and shortness of breath, and symptom severity can range from mild to severe (Faiman, Stricker, et al., 2017; Jones et al., 2013). Side effects of treatment include myelosuppression, fatigue, diarrhea, increased risk for infection, and peripheral neuropathy, which can exacerbate symptom severity and negatively affect QOL. Cumulative physiologic and psychological effects of symptoms, such as peripheral neuropathy, can lead to low QOL and limit patient access of new drugs to treat MM. The symptom burden of disease and treatments in MM can be substantial. All patients with MM experience symptoms of the disease or treatment to some extent, but their specific symptoms and symptom severity vary throughout the disease course (Howell et al., 2013). Variations in patient-reported symptoms may relate to differences between individuals, healthcare teams, and illness duration.
Symptoms rarely occur in isolation in patients with MM. Instead, clusters of complex symptoms may develop throughout the disease course. Symptoms may interact (e.g., patient develops steroid-induced hyperglycemia, which causes peripheral neuropathy symptoms to worsen), and symptoms may progress through various stages over time (Brant, Beck, & Miaskowski, 2010). New symptoms can result from MM treatment and, over time, place the patient at risk for worsening QOL, polypharmacy, and issues with self-management of multiple chronic illnesses and adherence to therapy (Tuchman et al., 2014).
Barriers to the effective identification of disease- and treatment-related symptoms and the influence these symptoms have on health-related QOL relate to the patient, provider, and healthcare system. Unfortunately, a paucity of research in MM symptoms exists, including why patients accept the symptoms as part of the disease, underestimate symptom severity, and fail to report symptoms to the healthcare provider (Potrata, Cavet, Blair, Howe, & Molassiotis, 2011).
Recommendations for Disease and Symptom Management
The IMF NLB was formed in 2006 and is comprised of 20 members. These nurse leaders see an average of 50 patients with MM per week and have from 9–33 years of myeloma nursing experience, with an average of 18 years of experience (IMF NLB, personal communication, May 27, 2017). The nurses conduct regular conference calls, meet face-to-face at least annually to discuss myeloma-related nursing issues, and strive to address gaps in education and patient care. Members of the IMF NLB have established best practice recommendations to manage MM and its symptoms.
This supplement includes five articles, addressing management of MM and MM treatment symptoms. The authors used Melnyk and Fineout-Overholt’s (2011) levels of evidence as a systematic framework to appraise and grade each of the IMF NLB’s consensus statements and to provide evidence-based recommendations for the management of patients with MM (see Figure 1). The rating system has seven levels of evidence based on qualitative studies, case-control studies, cohort studies, reports of expert committees, and opinions of authorities in the field. 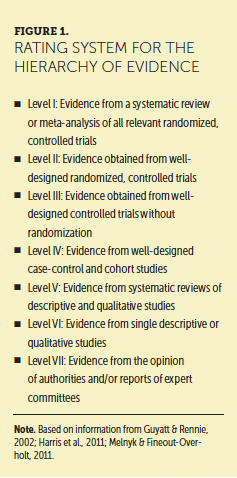
Catamero et al. (2017) focus on psychosocial needs in patients with MM and provides assessment tools and evidence for intervention on cancer-related fatigue, anxiety, depression, and sexual dysfunction. Faiman, Doss, et al. (2017) review organ health considerations, with attention to kidney, gastrointestinal, and peripheral neuropathy issues in MM. A thorough review of research, meta-analyses, and expert opinions was conducted, and best practice recommendations to assess these disease- and treatment-related symptoms were provided. Noonan, Rome, Faiman, and Verina (2017) highlight cardiovascular issues, such as deep vein thrombosis and cardiotoxicity. Nursing considerations for assessment, monitoring, and intervention are included in this article. Rome, Noonan, Bertolotti, and Miceli (2017) provide an in-depth overview of bone health and functional considerations in MM. Brigle et al. (2017) provide an overview of oncologic emergencies in MM. Key recommendations for the prevention and treatment of common emergencies, such as hypercalcemia of malignancy, spinal cord compression, renal failure, and myelosuppression, are emphasized. Also included in this supplement are patient education and healthcare provider tip sheets that readers can share with colleagues and patients.
The IMF NLB aims to improve the care and self-care of patients with MM and to create new professional activities, such as this supplement, and address the unmet needs of patients and the nurses who care for them. It is the hope of the IMF NLB that these peer-reviewed, evidenced-based recommendations will be accepted as a standard of nursing care for patients to manage short- and long-term side effects and symptoms and improve QOL.
The author gratefully acknowledges Rafat Abonour, MD, Brian G.M. Durie, MD, and Diane P. Moran, RN, MA, EdM, at the International Myeloma Foundation for their review of this manuscript.
About the Author(s)
Beth Faiman, PhD, MSN, APRN-BC, AOCN®, is a nurse practitioner in the Department of Hematology and Medical Oncology at the Cleveland Clinic Taussig Cancer Institute in Ohio. The author takes full responsibility for this content. This supplement was supported by the International Myeloma Foundation, with funding from Celgene Corporation, Karyopharm Therapeutics, and Takeda Oncology. Writing and editorial support was provided by Eubio Medical Communications. Faiman consults and serves on speakers bureaus for Amgen, Bristol-Myers Squibb, Celgene Corporation, and Takeda Oncology, and has received support from Celgene Corporation and Takeda Oncology. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Faiman can be reached at faimanb@ccf.org, with copy to CJONEditor@ons.org. (Submitted June 2017. Accepted July 17, 2017.)
References
Andrew, R., Derry, S., Taylor, R.S., Straube, S., & Phillips, C.J. (2014). The costs and consequences of adequately managed chronic non-cancer pain and chronic neuropathic pain. Pain Practice, 14, 79–94. https://doi.org/10.1111/papr.12050
Attal, M., Lauwers-Cances, V., Marit, G., Caillot, D., Moreau, P., Facon, T., . . . Harousseau, J.L. (2012). Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. New England Journal of Medicine, 366, 1782–1791.
Benboubker, L., Dimopoulos, M.A., Dispenzieri, A., Catalano, J., Belch, A.R., Cavo, M., . . . Facon, T. (2014). Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma. New England Journal of Medicine, 371, 906–917.
Brant, J.M., Beck, S., & Miaskowski, C. (2010). Building dynamic models and theories to advance the science of symptom management research. Journal of Advanced Nursing, 66, 228–240. https://doi.org/10.1111/j.1365-2648.2009.05179.x
Brigle, K., Pierre, A., Faiman, B., Finley-Oliver, E., Miceli, T., & Tariman, J. (2017). Myelosuppression, bone disease, and acute renal failure: Evidence-based recommendations for oncologic emergencies. Clinical Journal of Oncology Nursing, 21(Suppl. 5), 61–75. https://doi.org/10.1188.CJON.S5.61-75
Catamero, D., Noonan, K., Richards, T., Faiman, B., Manchulenko, C., Devine, H., . . . Gleason, C. (2017). Distress, fatigue, and sexuality: Understanding and treating concerns and symptoms in multiple myeloma survivors. Clinical Journal of Oncology Nursing, 21(Suppl. 5), 7–18. https://doi.org/10.1188.CJON.S5.7-18
Dodd, M., Janson, S., Facione, N., Faucett, J., Froelicher, E.S., Humphreys, J., . . . Taylor, D. (2001). Advancing the science of symptom management. Journal of Advanced Nursing, 33, 668–676.
Durie, B., Hoering, A., Rajkumar, S.V., Abidi, M.H., Epstein, J., Kahanic, S.P., . . . Dispenzieri, A. (2015). Bortezomib, lenalidomide and dexamethasone in patients (pts) with previously untreated multiple myeloma without an intent for immediate autologous stem cell transplant (ASCT): Results of the randomized phase III trial SWOG S0777. Blood, 126(23), 25.
Faiman, B., & Valent, J. (2016). Assessment and monitoring of patients receiving chemotherapy for multiple myeloma: Strategies to improve outcomes. Blood and Lymphatic Cancer: Targets and Therapy, 6, 21–35.
Faiman, B., Bilotti, E., Mangan, P.A., & Rogers, K. (2008). Steroid-associated side effects in patients with multiple myeloma: Consensus statement of the IMF Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(Suppl. 3), 53–63. https://doi.org/10.1188/08.CJON.S1.53-62
Faiman, B., Doss, D., Colson, K., Mangan, P., King, T., & Tariman, J. (2017). Renal, GI, and peripheral nerves: Evidence-based recommendations for the management of symptoms and care for patients with multiple myeloma. Clinical Journal of Oncology Nursing, 21(Suppl. 5), 19–36. https://doi.org/10.1188.CJON.S5.19-36
Faiman, B., Gleason, C., Colson, K., McNeill, A., & Catamero, D. (2016). Sequencing and integration of clinical trials. Journal of the Advanced Practitioner in Oncology, 7, 17–29.
Faiman, B., Moran, D., Gleason, C., Richards, T., Catamero, D., King, T., . . . Tariman, J.D. (2017). Symptom management and adherence in multiple myeloma (MM): A plan to disseminate best-practice guidelines for nurses [Abstract NP-288]. Paper presented at the 16th International Myeloma Workshop, New Delhi, India. Retrieved from https://show.jspargo.com/IMW/files/2017IMWAbstractBook.pdf
Faiman, B.M., Mangan, P., Spong, J., & Tariman, J.D. (2011). Renal complications in multiple myeloma and related disorders: Survivorship care plan of the International Myeloma Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl. 4), 66–76. https://doi.org/10.1188/11.CJON.S1.66-76
Faiman, B., Stricker, C., Harris, D, Chapman, A, Garber, G, Chapman, S, . . . Wujcik, D. (2017). Patient reported symptoms, concerns and provider intervention in patients with multiple myeloma [Abstract NS-283]. Paper presented at the 16th International Myeloma Workshop, New Delhi, India. Retrieved from http://bit.ly/2ldni41
Guyatt, G., & Rennie, D. (2002). Users’ guides to the medical literature. Chicago, IL: American Medical Association.
Harris, R.P., Hefland, M., Woolf, S.H., Lohr, K.N., Mulrow, C.D., Teutsch, S.M., & Atkins, D. (2001). Current methods of the U.S. Preventive Services task force: A review of the process. American Journal of Preventive Medicine, 20(3 Suppl.), 21–35.
Howell, D.A., Smith, A.G., Jack, A., Patmore, R., Macleod, U., Mironska, E., & Roman, E. (2013). Time-to-diagnosis and symptoms of myeloma, lymphomas and leukaemias: A report from the Haematological Malignancy Research Network. BMC Hematology, 13, 9.
Jones, D., Vichaya, E.G., Wang, X.S., Williams, L.A., Shah, N.D., Thomas, S.K., . . . Mendoza, T.R. (2013). Validation of the MD Anderson smyptom inventory multiple myeloma module. Journal of Hematology and Oncology, 6, 13.
Kumar, S.K., Dispenzieri, A., Gertz, M.A., Lacy, M.Q,, Lust, J.A., Hayman, S.R., . . . Rajkumar, S.V. (2012). Continued improvement in survival in multiple myeloma and the impact of novel agents. Blood, 120, 3972.
Kumar, S.K., Dispenzieri, A., Lacy, M.Q., Gertz, M.A., Buadi, F.K., Pandey, S., . . . Rajkumar, S.V. (2014). Continued improvement in survival in multiple myeloma: Changes in early mortality and outcomes in older patients. Leukemia, 28, 1122–1128.
Melnyk, B.M., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing and healthcare: A guide to best practice (2nd ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Miceli, T., Colson, K., Gavino, M., & Lilleby, K. (2008). Myelosuppression associated with novel therapies in patients with multiple myeloma: Consensus statement of the IMF Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(Suppl. 3), 13–19. https://doi.org/10.1188/08.CJON.S1.13-19
Miceli, T.S., Colson, K., Faiman, B.M., Miller, K., & Tariman, J.D. (2011). Maintaining bone health in patients with multiple myeloma: Survivorship care plan of the International Myeloma Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl.), 9–23.
Noonan, K., Rome, S., Faiman, B., & Verina, D. (2017). Heart and lung complications: Assessment and prevention of venous thromboembolism and cardiovascular disease in patients with multiple myeloma. Clinical Journal of Oncology Nursing, 21(Suppl. 5), 37–46. https://doi.org/10.1188.CJON.S5.37-46
Potrata, B., Cavet, J., Blair, S., Howe, T., & Molassiotis, A. (2011). Understanding distress and distressing experiences in patients living with multiple myeloma: An exploratory study. Psycho-Oncology, 20, 127–134.
Richards, T.A., Bertolotti, P.A., Doss, D., & McCullagh, E.J. (2011). Sexual dysfunction in multiple myeloma: Survivorship care plan of the International Myeloma Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl.), 53–65.
Rome, S., Doss, D., Miller, K., & Westphal, J. (2008). Thromboembolic events associated with novel therapies in patients with multiple myeloma: Consensus statement of the IMF Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(Suppl. 3), 21–28.
Rome, S., Jenkins, B.S., & Lilleby, K.E. (2011). Mobility and safety in the multiple myeloma survivor: Survivorship care plan of the International Myeloma Foundation Nurse Leadership Board. Clinical Journal of Oncology Nursing, 15(Suppl.), 41–52. https:// doi.org/10.1188/11.CJON.S1.41-52
Rome, S., Noonan, K., Bertolotti, P., & Miceli, T. (2017). Bone health, pain, and mobility: Evidence-based recommendations for patients with multiple myeloma. Clinical Journal of Oncology Nursing, 21(Suppl. 5), 47–59. https://doi.org/10.1188.CJON.S5.47-59
Smith, L.C., Bertolotti, P., Curran, K., & Jenkins, B. (2008). Gastrointestinal intestinal side effects associated with novel therapies in patients with multiple myeloma: Consensus statement of the IMF Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(Suppl. 3), 37–52. https://doi.org/10.1188/08.CJON.S1.37-51
Tariman, J.D., Love, G., McCullagh, E.J., & Sandifer, S. (2008). Peripheral neuropathy associated with novel therapies in patients with multiple myeloma: Consensus statement of the IMF Nurse Leadership Board. Clinical Journal of Oncology Nursing, 12(Suppl. 3), 29–35. https://doi.org/10.1188/08.CJON.S1.29-35
Tariman, J.D., & Szubski, K.L. (2015). The evolving role of the nurse during the cancer treatment decision-making process: A literature review. Clinical Journal of Oncology Nursing, 19, 548–556. https://doi.org/10.1188/15.CJON.548-556
Tuchman, S.A., Shapiro, G.R., Ershler, W.B., Badros, A., Cohen, H.J., Dispenzieri, A., . . . Yates, J.W. (2014). Multiple myeloma in the very old: An IASIA conference report. Journal of the National Cancer Institute, 106(5), dju067. https://doi.org/10.1093/jnci/dju067
Turner, J.G., Dawson, J.L., Grant, S., Shain, K.H., Dalton, W.S., Dai, Y., . . . Sullivan, D.M. (2016). Treatment of acquired drug resistance in multiple myeloma by combination therapy with XPO1 and topoisomerase II inhibitors. Journal of Hematology and Oncology, 9, 73.
Vehling, S., & Mehnert, A. (2014). Symptom burden, loss of dignity, and demoralization in patients with cancer: A mediation model. Psycho-Oncology, 23, 283–290. https://doi.org/10.1002/pon.3417




